If you're like most people, you think that heart disease is a problem for others. But heart disease is the number one killer in the U.S. It is also a major cause of disability. There are many different forms of heart disease. The most common cause of heart disease is narrowing or blockage of the coronary arteries, the blood vessels that supply blood to the heart itself. This is called coronary artery disease and happens slowly over time. It's the major reason people have heart attacks.
Other kinds of heart problems may happen to the valves in the heart, or the heart may not pump well and cause heart failure. Some people are born with heart disease.
You can help reduce your risk of heart disease by taking steps to control factors that put you at greater risk:
NIH: National Heart, Lung, and Blood Institute
Coronary heart disease—often simply called heart disease—is the main form of heart disease. It is a disorder of the blood vessels of the heart that can lead to heart attack. A heart attack happens when an artery becomes blocked, preventing oxygen and nutrients from getting to the heart. Heart disease is one of several cardiovascular diseases, which are diseases of the heart and blood vessel system. Other cardiovascular diseases include stroke, high blood pressure, angina (chest pain), and rheumatic heart disease.
One reason some women aren't too concerned about heart disease is that they think it can be "cured" with surgery or medication. This is a myth. Heart disease is a lifelong condition—once you get it, you'll always have it. True, procedures such as bypass surgery and percutaneous coronary intervention can help blood and oxygen flow to the heart more easily. But the arteries remain damaged, which means you are more likely to have a heart attack. What's more, the condition of your blood vessels will steadily worsen unless you make changes in your daily habits. Many women die of complications from heart disease, or become permanently disabled. That's why it is so vital to take action to prevent and control this disease. More information is available on cardiovascular diseases on the NHLBI Health Topics Website.
Next: What Are the Risk Factors for Heart Disease?
Risk factors are conditions or habits that make a person more likely to develop a disease. They can also increase the chances that an existing disease will get worse. Important risk factors for heart disease that you can do something about are:
Some risk factors, such as age and family history of early heart disease, can't be changed. For women, age becomes a risk factor at 55. After menopause, women are more apt to get heart disease, in part because their body's production of estrogen drops. Women who have gone through early menopause, either naturally or because they have had a hysterectomy, are twice as likely to develop heart disease as women of the same age who have not yet gone through menopause.
Another reason for the increasing risk is that middle age is a time when women tend to develop risk factors for heart disease. Family history of early heart disease is another risk factor that can't be changed. If your father or brother had a heart attack before age 55, or if your mother or sister had one before age 65, you are more likely to get heart disease yourself. Preeclampsia is another heart disease risk factor that you can't control. However, if you've had the condition, you should take extra care to try and control other heart disease risk factors.
You can make the changes gradually, one at a time. But making them is very important. Other women may wonder: If I have just one risk factor for heart disease—say, I'm overweight or I have high blood cholesterol—aren't I more or less "safe"? Absolutely not. Each risk factor greatly increases a woman's chance of developing heart disease. But having more than one risk factor is especially serious, because risk factors tend to "gang up" and worsen each other's effects. So, the message is clear: Every woman needs to take her heart disease risk seriously—and take action now to reduce that risk.
Next: How do I find out if I am at risk for heart disease?
Last Updated: July 10, 2014
The first step toward heart health is becoming aware of your own personal risk for heart disease. Some risks, such as smoking cigarettes, are obvious: every woman knows whether or not she smokes. But other risk factors, such as high blood pressure or high blood cholesterol, generally don't have obvious signs or symptoms. So you'll need to gather some information to create your personal "heart profile."
You and Your Doctor: A Heart Healthy Partnership
A crucial step in determining your risk is to see your doctor for a thorough checkup. Your doctor can be an important partner in helping you set and reach goals for heart health. But don't wait for your doctor to mention heart disease or its risk factors. Many doctors don't routinely bring up the subject with women patients. Here are some tips for establishing good, clear communication between you and your doctor:
Speak up. Tell your doctor you want to keep your heart healthy and would like help in achieving that goal. Ask questions about your chances of developing heart disease and how you can lower your risk. See "Questions To Ask Your Doctor" on page 15 of The Healthy Heart Handbook for Women ![]() (2.47MB). Also ask for tests that will determine your personal risk factors. (See "Check It Out"
(2.47MB). Also ask for tests that will determine your personal risk factors. (See "Check It Out" ![]() (46KB) on page 16 of The Healthy Heart Handbook for Women.)
(46KB) on page 16 of The Healthy Heart Handbook for Women.)
Keep tabs on treatment. If you already are being treated for heart disease or heart disease risk factors, ask your doctor to review your treatment plan with you. Ask: Is what I'm doing in line with the latest recommendations? Are my treatments working? Are my risk factors under control? If your doctor recommends a medical procedure, ask about its benefits and risks. Find out if you will need to be hospitalized and for how long, and what to expect during the recovery period.
Be open. When your doctor asks you questions, answer as honestly and fully as you can. While certain topics may seem quite personal, discussing them openly can help your doctor find out your chances of developing heart disease. It can also help your doctor work with you to reduce your risk. If you already have heart disease, briefly describe each of your symptoms. Include when each symptom started, how often it happens, and whether it has been getting worse.
Keep it simple. If you don't understand something your doctor says, ask for an explanation in simple language. Be especially sure you understand how to take any medication you are given. If you are worried about understanding what the doctor says, or if you have trouble hearing, bring a friend or relative with you to your appointment. You may want to ask that person to write down the doctor's instructions for you.
Next: What should I know about menopausal hormone therapy and heart disease?
Last Updated: February 29, 2012
Menopausal hormone therapy once seemed the answer for many of the conditions women face as they age. It was thought that hormone therapy could ward off heart disease, osteoporosis, and cancer, while improving women's quality of life. But beginning in July 2002, findings emerged from clinical trials that showed this was not so. In fact, long-term use of hormone therapy poses serious risks and may increase the risk of heart attack and stroke. The findings come from the Women's Health Initiative (WHI), launched in 1991 to test ways to prevent a number of medical disorders in postmenopausal women. It consists of a set of clinical studies on hormone therapy, diet modification, and calcium and vitamin D supplements; an observational study; and a community prevention study.
The two hormone therapy clinical studies were both stopped early because of serious risks and the failure to prevent heart disease. Briefly, the estrogen-plus-progestin therapy increased women's risk for heart attacks, stroke, blood clots, and breast cancer. These risks diminished after stopping estrogen-plus-progestin. Estrogen-plus-progestin also doubled the risk of dementia and did not protect women against memory loss. However, the therapy had some benefits: It reduced the risk for colorectal cancer and bone fractures. Estrogen-alone therapy increased the risk for stroke and venous thrombosis (blood clot, usually in one of the deep veins of the legs). It had no effect on heart disease and colorectal cancer, and an uncertain effect on breast cancer. Estrogen alone gave no protection against memory loss, and there were more cases of dementia in those who took the therapy than those on the placebo, although the increase was not statistically significant. Estrogen alone reduced the risk for bone fractures.
While questions remain, the findings make possible some advice about using hormone therapy: Estrogen alone or with progestin should not be used to prevent heart disease. Talk with your doctor about other ways of preventing heart attack and stroke, including lifestyle changes and medicines such as cholesterol-lowering statins and blood pressure drugs.
If You Have Heart Disease: Menopausal hormone therapy was once thought to lower the risk of heart attack and stroke for women with heart disease. But research now shows that women with heart disease should not take it. Menopausal hormone therapy can involve the use of estrogen alone or estrogen plus progestin. For women with heart disease, estrogen alone will not prevent heart attacks, and estrogen plus progestin increases the risk for heart attack during the first few years of use. Estrogen plus progestin also increases the risk for blood clots, stroke, and breast cancer.
Source: National Heart, Lung, & Blood Institute, NIH
Your heart is a muscular organ that pumps blood to your body. Your heart is at the center of your circulatory system. This system consists of a network of blood vessels, such as arteries, veins, and capillaries. These blood vessels carry blood to and from all areas of your body.
An electrical system controls your heart and uses electrical signals to contract the heart's walls. When the walls contract, blood is pumped into your circulatory system. Inlet and outlet valves in your heart chambers ensure that blood flows in the right direction.
Your heart is vital to your health and nearly everything that goes on in your body. Without the heart's pumping action, blood can't move throughout your body.
Your blood carries the oxygen and nutrients that your organs need to work well. Blood also carries carbon dioxide (a waste product) to your lungs so you can breathe it out.
A healthy heart supplies your body with the right amount of blood at the rate needed to work well. If disease or injury weakens your heart, your body's organs won't receive enough blood to work normally.
Your heart is located under your ribcage in the center of your chest between your right and left lungs. Its muscular walls beat, or contract, pumping blood to all parts of your body.
The size of your heart can vary depending on your age, size, and the condition of your heart. A normal, healthy, adult heart usually is the size of an average clenched adult fist. Some diseases can cause the heart to enlarge.
Below is a picture of the outside of a normal, healthy, human heart.
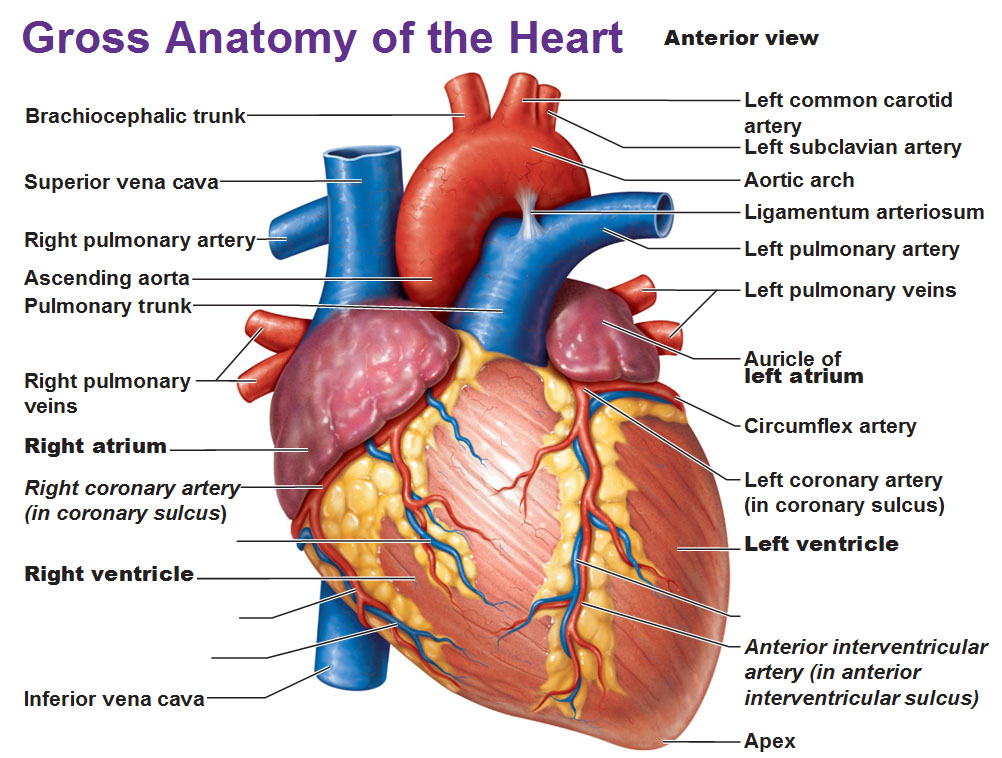

Figure A shows the location of the heart in the body. Figure B shows the front surface of the heart, including the coronary arteries and major blood vessels.
In figure B, the heart is the muscle in the lower half of the picture. The heart has four chambers. The heart's upper chambers, the right and left atria (AY-tree-uh), are shown in purple. The heart's lower chambers, the right and left ventricles (VEN-trih-kuls), are shown in red.
Some of the main blood vessels (arteries and veins) that make up your circulatory system are directly connected to the heart.
In figure B above, the superior and inferior vena cavae are shown in blue to the left of the heart muscle as you look at the picture. These veins are the largest veins in your body.
After your body's organs and tissues have used the oxygen in your blood, the vena cavae carry the oxygen-poor blood back to the right atrium of your heart.
The superior vena cava carries oxygen-poor blood from the upper parts of your body, including your head, chest, arms, and neck. The inferior vena cava carries oxygen-poor blood from the lower parts of your body.
The oxygen-poor blood from the vena cavae flows into your heart's right atrium and then to the right ventricle. From the right ventricle, the blood is pumped through the pulmonary (PULL-mun-ary) arteries (shown in blue in the center of figure B) to your lungs.
Once in the lungs, the blood travels through many small, thin blood vessels called capillaries. There, the blood picks up more oxygen and transfers carbon dioxide to the lungs—a process called gas exchange. To learn more about gas exchange, go to the Health Topics How the Lungs Work article.
The oxygen-rich blood passes from your lungs back to your heart through the pulmonary veins (shown in red to the left of the right atrium in figure B).
Oxygen-rich blood from your lungs passes through the pulmonary veins (shown in red to the right of the left atrium in figure B above). The blood enters the left atrium and is pumped into the left ventricle.
From the left ventricle, the oxygen-rich blood is pumped to the rest of your body through the aorta. The aorta is the main artery that carries oxygen-rich blood to your body.
Like all of your organs, your heart needs oxygen-rich blood. As blood is pumped out of your heart's left ventricle, some of it flows into the coronary arteries (shown in red in figure B).
Your coronary arteries are located on your heart's surface at the beginning of the aorta. They carry oxygen-rich blood to all parts of your heart.
Below is a picture of the inside of a normal, healthy, human heart.
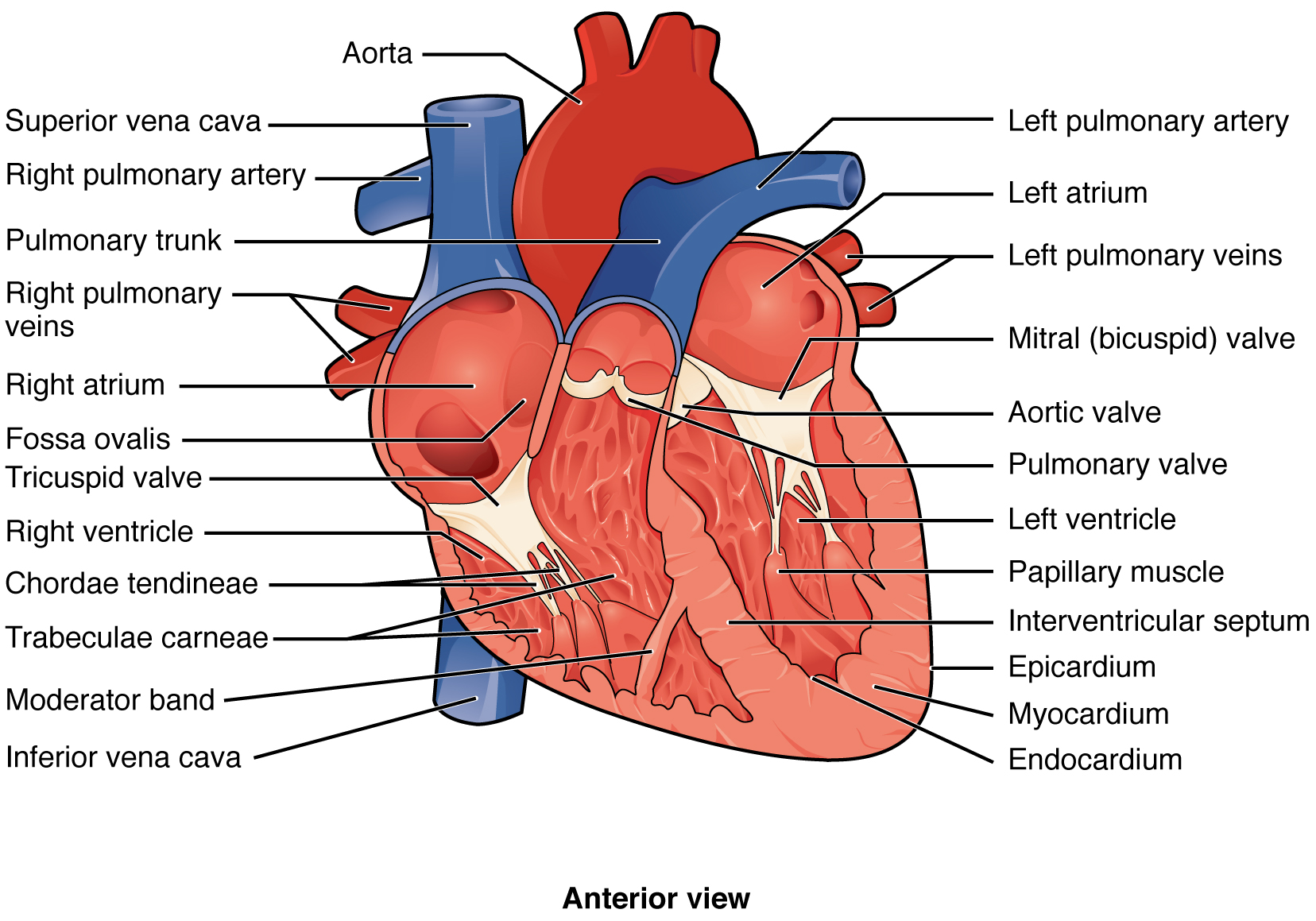
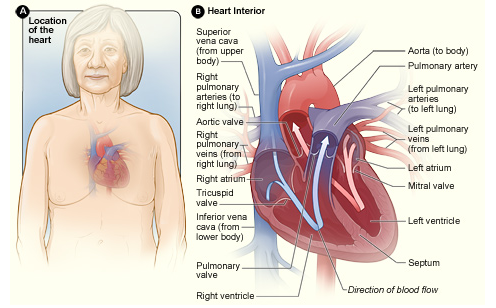
Figure A shows the location of the heart in the body. Figure B shows a cross-section of a healthy heart and its inside structures. The blue arrow shows the direction in which oxygen-poor blood flows through the heart to the lungs. The red arrow shows the direction in which oxygen-rich blood flows from the lungs into the heart and then out to the body.
Figure B shows the inside of your heart and how it's divided into four chambers. The two upper chambers of your heart are called the atria. They receive and collect blood.
The two lower chambers of your heart are called ventricles. The ventricles pump blood out of your heart to other parts of your body.
An internal wall of tissue divides the right and left sides of your heart. This wall is called the septum.
The area of the septum that divides the atria is called the atrial or interatrial septum. The area of the septum that divides the ventricles is called the ventricular or interventricular septum.
Figure B shows your heart's four valves. Shown counterclockwise in the picture, the valves include the aortic (ay-OR-tik) valve, the tricuspid (tri-CUSS-pid) valve, the pulmonary valve, and the mitral (MI-trul) valve.
The arrows in figure B show the direction that blood flows through your heart. The light blue arrow shows that blood enters the right atrium of your heart from the superior and inferior vena cavae.
From the right atrium, blood is pumped into the right ventricle. From the right ventricle, blood is pumped to your lungs through the pulmonary arteries.
The light red arrow shows oxygen-rich blood coming from your lungs through the pulmonary veins into your heart's left atrium. From the left atrium, the blood is pumped into the left ventricle. The left ventricle pumps the blood to the rest of your body through the aorta.
For the heart to work well, your blood must flow in only one direction. Your heart's valves make this possible. Both of your heart's ventricles have an "in" (inlet) valve from the atria and an "out" (outlet) valve leading to your arteries.
Healthy valves open and close in exact coordination with the pumping action of your heart's atria and ventricles. Each valve has a set of flaps called leaflets or cusps that seal or open the valve. This allows blood to pass through the chambers and into your arteries without backing up or flowing backward.
The animation below shows how your heart pumps blood. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
The animation shows how blood flows through the heart as it contracts and relaxes.
Almost everyone has heard the real or recorded sound of a heartbeat. When your heart beats, it makes a "lub-DUB" sound. Between the time you hear "lub" and "DUB," blood is pumped through your heart and circulatory system.
A heartbeat may seem like a simple, repeated event. However, it's a complex series of very precise and coordinated events. These events take place inside and around your heart.
Each side of your heart uses an inlet valve to help move blood between the atrium and ventricle. The tricuspid valve does this between the right atrium and ventricle. The mitral valve does this between the left atrium and ventricle. The "lub" is the sound of the tricuspid and mitral valves closing.
Each of your heart's ventricles also has an outlet valve. The right ventricle uses the pulmonary valve to help move blood into the pulmonary arteries. The left ventricle uses the aortic valve to do the same for the aorta. The "DUB" is the sound of the aortic and pulmonary valves closing.
Each heartbeat has two basic parts: diastole (di-AS-toe-lee) and systole (SIS-toe-lee).
During diastole, the atria and ventricles of your heart relax and begin to fill with blood. At the end of diastole, your heart's atria contract (atrial systole) and pump blood into the ventricles.
The atria then begin to relax. Next, your heart's ventricles contract (ventricular systole) and pump blood out of your heart.
Your heart uses its four valves to ensure your blood flows in only one direction. Healthy valves open and close in coordination with the pumping action of your heart's atria and ventricles.
Each valve has a set of flaps called leaflets or cusps that seal or open the valve. The cusps allow pumped blood to pass through the chambers and into your blood vessels without backing up or flowing backward.
Oxygen-poor blood from the vena cavae fills your heart's right atrium. The atrium contracts (atrial systole). The tricuspid valve located between the right atrium and ventricle opens for a short time and then shuts. This allows blood to enter the right ventricle without flowing back into the right atrium.
When your heart's right ventricle fills with blood, it contracts (ventricular systole). The pulmonary valve located between your right ventricle and pulmonary artery opens and closes quickly.
This allows blood to enter into your pulmonary arteries without flowing back into the right ventricle. This is important because the right ventricle begins to refill with more blood through the tricuspid valve. Blood travels through the pulmonary arteries to your lungs to pick up oxygen.
Oxygen-rich blood returns from the lungs to your heart's left atrium through the pulmonary veins. As your heart's left atrium fills with blood, it contracts. This event is called atrial systole.
The mitral valve located between the left atrium and left ventricle opens and closes quickly. This allows blood to pass from the left atrium into the left ventricle without flowing backward.
As the left ventricle fills with blood, it contracts. This event is called ventricular systole. The aortic valve located between the left ventricle and aorta opens and closes quickly. This allows blood to flow into the aorta. The aorta is the main artery that carries blood from your heart to the rest of your body.
The aortic valve closes quickly to prevent blood from flowing back into the left ventricle, which already is filling up with new blood.
When your heart pumps blood through your arteries, it creates a pulse that you can feel on the arteries close to the skin's surface. For example, you can feel the pulse on the artery inside of your wrist, below your thumb.
You can count how many times your heart beats by taking your pulse. You will need a watch with a second hand.
To find your pulse, gently place your index and middle fingers on the artery located on the inner wrist of either arm, below your thumb. You should feel a pulsing or tapping against your fingers.
Watch the second hand and count the number of pulses you feel in 30 seconds. Double that number to find out your heart rate or pulse for 1 minute.
The usual resting pulse for an adult is 60 to 100 beats per minute. To find your resting pulse, count your pulse after you have been sitting or resting quietly for at least 10 minutes.
Your heart and blood vessels make up your overall blood circulatory system. Your blood circulatory system is made up of four subsystems.
Arterial circulation is the part of your circulatory system that involves arteries, like the aorta and pulmonary arteries. Arteries are blood vessels that carry blood away from your heart. (The exception is the coronary arteries, which supply your heart muscle with oxygen-rich blood.)
Healthy arteries are strong and elastic (stretchy). They become narrow between heartbeats, and they help keep your blood pressure consistent. This helps blood move through your body.
Arteries branch into smaller blood vessels called arterioles (ar-TEER-e-ols). Arteries and arterioles have strong, flexible walls that allow them to adjust the amount and rate of blood flowing to parts of your body.
Venous circulation is the part of your circulatory system that involves veins, like the vena cavae and pulmonary veins. Veins are blood vessels that carry blood to your heart.
Veins have thinner walls than arteries. Veins can widen as the amount of blood passing through them increases.
Capillary circulation is the part of your circulatory system where oxygen, nutrients, and waste pass between your blood and parts of your body.
Capillaries are very small blood vessels. They connect the arterial and venous circulatory subsystems.
The importance of capillaries lies in their very thin walls. Oxygen and nutrients in your blood can pass through the walls of the capillaries to the parts of your body that need them to work normally.
Capillaries' thin walls also allow waste products like carbon dioxide to pass from your body's organs and tissues into the blood, where it's taken away to your lungs.
Pulmonary circulation is the movement of blood from the heart to the lungs and back to the heart again. Pulmonary circulation includes both arterial and venous circulation.
Oxygen-poor blood is pumped to the lungs from the heart (arterial circulation). Oxygen-rich blood moves from the lungs to the heart through the pulmonary veins (venous circulation).
Pulmonary circulation also includes capillary circulation. Oxygen you breathe in from the air passes through your lungs into your blood through the many capillaries in the lungs. Oxygen-rich blood moves through your pulmonary veins to the left side of your heart and out of the aorta to the rest of your body.
Capillaries in the lungs also remove carbon dioxide from your blood so that your lungs can breathe the carbon dioxide out into the air.
he animation below shows how your heart's electrical system works. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
The animation shows how the heart's internal electrical system causes the heart to pump blood.
Your heart's electrical system controls all the events that occur when your heart pumps blood. The electrical system also is called the cardiac conduction system. If you've ever seen the heart test called an EKG (electrocardiogram), you've seen a graphical picture of the heart's electrical activity.
Your heart's electrical system is made up of three main parts:
A heartbeat is a complex series of events. These events take place inside and around your heart. A heartbeat is a single cycle in which your heart's chambers relax and contract to pump blood. This cycle includes the opening and closing of the inlet and outlet valves of the right and left ventricles of your heart.
Each heartbeat has two basic parts: diastole and systole. During diastole, the atria and ventricles of your heart relax and begin to fill with blood.
At the end of diastole, your heart's atria contract (atrial systole) and pump blood into the ventricles. The atria then begin to relax. Your heart's ventricles then contract (ventricular systole), pumping blood out of your heart.
Each beat of your heart is set in motion by an electrical signal from within your heart muscle. In a normal, healthy heart, each beat begins with a signal from the SA node. This is why the SA node sometimes is called your heart's natural pacemaker. Your pulse, or heart rate, is the number of signals the SA node produces per minute.
The signal is generated as the vena cavae fill your heart's right atrium with blood from other parts of your body. The signal spreads across the cells of your heart's right and left atria.
This signal causes the atria to contract. This action pushes blood through the open valves from the atria into both ventricles.
The signal arrives at the AV node near the ventricles. It slows for an instant to allow your heart's right and left ventricles to fill with blood. The signal is released and moves along a pathway called the bundle of His, which is located in the walls of your heart's ventricles.
From the bundle of His, the signal fibers divide into left and right bundle branches through the Purkinje fibers. These fibers connect directly to the cells in the walls of your heart's left and right ventricles (see yellow on the picture in the animation).
The signal spreads across the cells of your ventricle walls, and both ventricles contract. However, this doesn't happen at exactly the same moment.
The left ventricle contracts an instant before the right ventricle. This pushes blood through the pulmonary valve (for the right ventricle) to your lungs, and through the aortic valve (for the left ventricle) to the rest of your body.
As the signal passes, the walls of the ventricles relax and await the next signal.
This process continues over and over as the atria refill with blood and more electrical signals come from the SA node.
Your heart is made up of many parts working together to pump blood. In a healthy heart, all the parts work well so that your heart pumps blood normally. As a result, all parts of your body that depend on the heart to deliver blood also stay healthy.
Heart disease can disrupt a heart's normal electrical system and pumping functions. Diseases and conditions of the heart's muscle make it hard for your heart to properly pump blood.
Damaged or diseased blood vessels make the heart work harder than normal. Problems with the heart's electrical system, called arrhythmias (ah-RITH-me-ahs), can make it hard for the heart to pump blood efficiently.
Health Topics has many articles about heart diseases and conditions. For more information, go to the Health Topics home page.
Source: National Heart, Lung, & Blood Institute, NIH
What Is Coronary Heart Disease?
Coronary heart disease (CHD) is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
When plaque builds up in the arteries, the condition is called atherosclerosis (ATH-er-o-skler-O-sis). The buildup of plaque occurs over many years.

Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart.
If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. Over time, ruptured plaque also hardens and narrows the coronary arteries.
If the flow of oxygen-rich blood to your heart muscle is reduced or blocked, angina (an-JI-nuh or AN-juh-nuh) or a heart attack can occur.
Angina is chest pain or discomfort. It may feel like pressure or squeezing in your chest. The pain also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion.
A heart attack occurs if the flow of oxygen-rich blood to a section of heart muscle is cut off. If blood flow isn’t restored quickly, the section of heart muscle begins to die. Without quick treatment, a heart attack can lead to serious health problems or death.
Over time, CHD can weaken the heart muscle and lead to heart failure and arrhythmias (ah-RITH-me-ahs). Heart failure is a condition in which your heart can't pump enough blood to meet your body’s needs. Arrhythmias are problems with the rate or rhythm of the heartbeat.
CHD is the most common type of heart disease. In the United States, CHD is the #1 cause of death for both men and women. Lifestyle changes, medicines, and medical procedures can help prevent or treat CHD. These treatments may reduce the risk of related health problems.
Research suggests that coronary heart disease (CHD) starts when certain factors damage the inner layers of the coronary arteries. These factors include:
Plaque might begin to build up where the arteries are damaged. The buildup of plaque in the coronary arteries may start in childhood.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause angina (chest pain or discomfort).
If the plaque ruptures, blood cell fragments called platelets (PLATE-lets) stick to the site of the injury. They may clump together to form blood clots.
Blood clots can further narrow the coronary arteries and worsen angina. If a clot becomes large enough, it can mostly or completely block a coronary artery and cause a heart attack.
In the United States, coronary heart disease (CHD) is a leading cause of death for both men and women. Each year, about 375,000 Americans die from CHD.
Certain traits, conditions, or habits may raise your risk for CHD. The more risk factors you have, the more likely you are to develop the disease.
You can control many risk factors, which may help prevent or delay CHD.
Although older age and a family history of early heart disease are risk factors, it doesn't mean that you’ll develop CHD if you have one or both. Controlling other risk factors often can lessen genetic influences and help prevent CHD, even in older adults.
Researchers continue to study other possible risk factors for CHD.
High levels of a protein called C-reactive protein (CRP) in the blood may raise the risk of CHD and heart attack. High levels of CRP are a sign of inflammation in the body.
Inflammation is the body's response to injury or infection. Damage to the arteries' inner walls may trigger inflammation and help plaque grow.
Research is under way to find out whether reducing inflammation and lowering CRP levels also can reduce the risk of CHD and heart attack.
High levels of triglycerides (tri-GLIH-seh-rides) in the blood also may raise the risk of CHD, especially in women. Triglycerides are a type of fat.
Other conditions and factors also may contribute to CHD, including:
For more detailed information, go to the Health Topics Coronary Heart Disease Risk Factors article.
A common symptom of coronary heart disease (CHD) is angina. Angina is chest pain or discomfort that occurs if an area of your heart muscle doesn't get enough oxygen-rich blood.
Angina may feel like pressure or squeezing in your chest. You also may feel it in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion. The pain tends to get worse with activity and go away with rest. Emotional stress also can trigger the pain.
Another common symptom of CHD is shortness of breath. This symptom occurs if CHD causes heart failure. When you have heart failure, your heart can't pump enough blood to meet your body’s needs. Fluid builds up in your lungs, making it hard to breathe.
The severity of these symptoms varies. They may get more severe as the buildup of plaque continues to narrow the coronary arteries.
Some people who have CHD have no signs or symptoms—a condition called silent CHD. The disease might not be diagnosed until a person has signs or symptoms of a heart attack, heart failure, or an arrhythmia (an irregular heartbeat).
A heart attack occurs if the flow of oxygen-rich blood to a section of heart muscle is cut off. This can happen if an area of plaque in a coronary artery ruptures (breaks open).
Blood cell fragments called platelets stick to the site of the injury and may clump together to form blood clots. If a clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn’t treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
Figure A shows the location of the heart in the body. Figure B is an overview of a heart and coronary artery showing damage (dead heart muscle) caused by a heart attack. Figure C is a cross-section of the coronary artery with plaque buildup and a blood clot.
The most common heart attack symptom is chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest that often lasts for more than a few minutes or goes away and comes back.
The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain. The feeling can be mild or severe. Heart attack pain sometimes feels like indigestion or heartburn.
The symptoms of angina can be similar to the symptoms of a heart attack. Angina pain usually lasts for only a few minutes and goes away with rest.
Chest pain or discomfort that doesn’t go away or changes from its usual pattern (for example, occurs more often or while you’re resting) might be a sign of a heart attack. If you don’t know whether your chest pain is angina or a heart attack, call 9–1–1.
All chest pain should be checked by a doctor.
Other common signs and symptoms of a heart attack include:
For more information, go to the Health Topics Heart Attack article.
Heart failure is a condition in which your heart can't pump enough blood to meet your body’s needs. Heart failure doesn't mean that your heart has stopped or is about to stop working.
The most common signs and symptoms of heart failure are shortness of breath or trouble breathing; fatigue; and swelling in the ankles, feet, legs, stomach, and veins in the neck.
All of these symptoms are the result of fluid buildup in your body. When symptoms start, you may feel tired and short of breath after routine physical effort, like climbing stairs.
For more information, go to the Health Topics Heart Failure article.
An arrhythmia is a problem with the rate or rhythm of the heartbeat. When you have an arrhythmia, you may notice that your heart is skipping beats or beating too fast.
Some people describe arrhythmias as a fluttering feeling in the chest. These feelings are called palpitations (pal-pih-TA-shuns).
Some arrhythmias can cause your heart to suddenly stop beating. This condition is called sudden cardiac arrest (SCA). SCA usually causes death if it's not treated within minutes.
For more information, go to the Health Topics Arrhythmia article.
Your doctor will diagnose coronary heart disease (CHD) based on your medical and family histories, your risk factors for CHD, a physical exam, and the results from tests and procedures.
No single test can diagnose CHD. If your doctor thinks you have CHD, he or she may recommend one or more of the following tests.
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage due to CHD and signs of a previous or current heart attack.
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can't exercise, you may be given medicine to raise your heart rate.
When your heart is working hard and beating fast, it needs more blood and oxygen. Plaque-narrowed arteries can't supply enough oxygen-rich blood to meet your heart's needs.
A stress test can show possible signs and symptoms of CHD, such as:
If you can't exercise for as long as what is considered normal for someone your age, your heart may not be getting enough oxygen-rich blood. However, other factors also can prevent you from exercising long enough (for example, lung diseases, anemia, or poor general fitness).
As part of some stress tests, pictures are taken of your heart while you exercise and while you rest. These imaging stress tests can show how well blood is flowing in your heart and how well your heart pumps blood when it beats.
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The picture shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can show areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
A chest x ray takes pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels.
A chest x ray can reveal signs of heart failure, as well as lung disorders and other causes of symptoms not related to CHD.
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels might be a sign that you're at risk for CHD.
Your doctor may recommend coronary angiography (an-jee-OG-rah-fee) if other tests or factors show that you're likely to have CHD. This test uses dye and special x rays to show the insides of your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-eh-ter-ih-ZA-shun).
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through your coronary arteries. The dye lets your doctor study the flow of blood through your heart and blood vessels.
Cardiac catheterization usually is done in a hospital. You're awake during the procedure. It usually causes little or no pain, although you may feel some soreness in the blood vessel where your doctor inserts the catheter.
Treatments for coronary heart disease (CHD) include lifestyle changes, medicines, and medical procedures. Treatment goals may include:
Making lifestyle changes often can help prevent or treat CHD. Lifestyle changes might be the only treatment that some people need.
A healthy diet is an important part of a healthy lifestyle. Following a healthy diet can prevent or reduce high blood pressure and high blood cholesterol and help you maintain a healthy weight.
For information about healthy eating, go to the National Heart, Lung, and Blood Institute's (NHLBI's) Aim for a Healthy Weight Web site. This site provides practical tips on healthy eating, physical activity, and controlling your weight.
Therapeutic Lifestyle Changes (TLC). Your doctor may recommend TLC if you have high blood cholesterol. TLC is a three-part program that includes a healthy diet, physical activity, and weight management.
With the TLC diet, less than 7 percent of your daily calories should come from saturated fat. This kind of fat is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods.
No more than 25 to 35 percent of your daily calories should come from all fats, including saturated, trans, monounsaturated, and polyunsaturated fats.
You also should have less than 200 mg a day of cholesterol. The amounts of cholesterol and the types of fat in prepared foods can be found on the foods' Nutrition Facts labels.
Foods high in soluble fiber also are part of a healthy diet. They help prevent the digestive tract from absorbing cholesterol. These foods include:
A diet rich in fruits and vegetables can increase important cholesterol-lowering compounds in your diet. These compounds, called plant stanols or sterols, work like soluble fiber.
A healthy diet also includes some types of fish, such as salmon, tuna (canned or fresh), and mackerel. These fish are a good source of omega-3 fatty acids. These acids may help protect the heart from blood clots and inflammation and reduce the risk of heart attack. Try to have about two fish meals every week.
You also should try to limit the amount of sodium (salt) that you eat. This means choosing low-salt and "no added salt" foods and seasonings at the table or while cooking. The Nutrition Facts label on food packaging shows the amount of sodium in the item.
Try to limit drinks that contain alcohol. Too much alcohol will raise your blood pressure and triglyceride level. (Triglycerides are a type of fat found in the blood.) Alcohol also adds extra calories, which will cause weight gain.
Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. One drink is a glass of wine, beer, or a small amount of hard liquor.
For more information about TLC, go to the NHLBI's "Your Guide to Lowering Your Cholesterol With TLC."
Dietary Approaches to Stop Hypertension (DASH). Your doctor may recommend the DASH eating plan if you have high blood pressure. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart healthy and low in fat, cholesterol, and sodium.
DASH also focuses on fat-free or low-fat milk and dairy products, fish, poultry, and nuts. The DASH eating plan is reduced in red meats (including lean red meats), sweets, added sugars, and sugar-containing beverages. It's rich in nutrients, protein, and fiber.
The DASH eating plan is a good healthy eating plan, even for those who don’t have high blood pressure. For more information, go to the NHLBI’s "Your Guide to Lowering Your Blood Pressure With DASH."
Routine physical activity can lower many CHD risk factors, including LDL ("bad") cholesterol, high blood pressure, and excess weight.
Physical activity also can lower your risk for diabetes and raise your HDL cholesterol level. HDL is the "good" cholesterol that helps prevent CHD.
Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. The more active you are, the more you will benefit.
For more information about physical activity, go to the U.S. Department of Health and Human Services' "2008 Physical Activity Guidelines for Americans," the Health Topics Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Maintaining a healthy weight can lower your risk for CHD. A general goal to aim for is a body mass index (BMI) of less than 25.
BMI measures your weight in relation to your height and gives an estimate of your total body fat. You can use the NHLBI's online BMI calculator to figure out your BMI, or your doctor can help you.
A BMI between 25 and 29.9 is considered overweight. A BMI of 30 or more is considered obese. A BMI of less than 25 is the goal for preventing and treating CHD. Your doctor or other health care provider can help you set an appropriate BMI goal.
For more information about losing weight or maintaining a healthy weight, go to the Health Topics Overweight and Obesity article.
If you smoke, quit. Smoking can raise your risk for CHD and heart attack and worsen other CHD risk factors. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the NHLBI's "Your Guide to a Healthy Heart."
Research shows that the most commonly reported "trigger" for a heart attack is an emotionally upsetting event—particularly one involving anger. Also, some of the ways people cope with stress—such as drinking, smoking, or overeating—aren't healthy.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress.
Physical activity, medicine, and relaxation therapy also can help relieve stress. You may want to consider taking part in a stress management program.
You may need medicines to treat CHD if lifestyle changes aren't enough. Medicines can:
Medicines used to treat CHD include anticoagulants (AN-te-ko-AG-u-lants), also called blood thinners; aspirin and other anticlotting medicines; ACE inhibitors; beta blockers; calcium channel blockers; nitroglycerin; glycoprotein IIb-IIIa; statins; and fish oil and other supplements high in omega-3 fatty acids.
You may need a procedure or surgery to treat CHD. Both angioplasty and CABG are used to treat blocked coronary arteries. You and your doctor can discuss which treatment is right for you.
Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a nonsurgical procedure that opens blocked or narrowed coronary arteries.
A thin, flexible tube with a balloon or other device on the end is threaded through a blood vessel to the narrowed or blocked coronary artery.
Once in place, the balloon is inflated to compress the plaque against the wall of the artery. This restores blood flow through the artery.
During the procedure, the doctor may put a small mesh tube called a stent in the artery. The stent helps prevent blockages in the artery in the months or years after angioplasty.
For more information, go to the Health Topics PCI article.
CABG is a type of surgery. In CABG, arteries or veins from other areas in your body are used to bypass (that is, go around) your narrowed coronary arteries. CABG can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
For more information, go to the Health Topics Coronary Artery Bypass Grafting article.
Your doctor may prescribe cardiac rehabilitation (rehab) for angina or after CABG, angioplasty, or a heart attack. Almost everyone who has CHD can benefit from cardiac rehab.
Cardiac rehab is a medically supervised program that may help improve the health and well-being of people who have heart problems.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians or nutritionists, and psychologists or other mental health specialists.
Rehab has two parts:
For more information, go to the Health Topics Cardiac Rehabilitation article.
Taking action to control your risk factors can help prevent or delay coronary heart disease (CHD). Your risk for CHD increases with the number of risk factors you have.
One step you can take is to adopt a healthy lifestyle. Following a healthy diet is an important part of a healthy lifestyle.
A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, and beans and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
The National Heart, Lung, and Blood Institute's (NHLBI's) Therapeutic Lifestyle Changes (TLC) and Dietary Approaches to Stop Hypertension (DASH) are two programs that promote healthy eating.
If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan. Controlling your weight helps you control CHD risk factors.
Be as physically active as you can. Physical activity can improve your fitness level and your health. Talk with your doctor about what types of activity are safe for you.
For more information about physical activity, go to the Health Topics Physical Activity and Your Heart article and the NHLBI’s “Your Guide to Physical Activity and Your Heart.”
If you smoke, quit. Smoking can damage and tighten blood vessels and raise your risk for CHD. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
For more information about quitting smoking, go to the Health Topics Smoking and Your Heart article and the NHLBI’s “Your Guide to a Healthy Heart.”
Know your family history of health problems related to CHD. If you or someone in your family has CHD, be sure to tell your doctor.
If lifestyle changes aren't enough, you also may need medicines to control your CHD risk factors. Take all of your medicines as prescribed.
For more information about lifestyle changes and medicines, go to "How Is Coronary Heart Disease Treated?"
Coronary heart disease (CHD) can cause serious complications. However, if you follow your doctor's advice and adopt healthy lifestyle habits, you can prevent or reduce the risk of:
Lifestyle changes and medicines can help control CHD. Lifestyle changes include following a healthy diet, being physically active, maintaining a healthy weight, quitting smoking, and managing stress.
For more information about lifestyle changes and medicines, go to "How Is Coronary Heart Disease Treated?"
Work closely with your doctor to control your blood pressure and manage your blood cholesterol and blood sugar levels.
A blood test called a lipoprotein panel will measure your cholesterol and triglyceride levels. A fasting blood glucose test will check your blood sugar level and show whether you're at risk for or have diabetes.
These tests show whether your risk factors are controlled, or whether your doctor needs to adjust your treatment for better results.
Talk with your doctor about how often you should schedule office visits or blood tests. Between those visits, call your doctor if you have any new symptoms or if your symptoms worsen.
CHD raises your risk for a heart attack. Learn the signs and symptoms of a heart attack, and call 9–1–1 if you have any of these symptoms:
Symptoms also may include sleep problems, fatigue (tiredness), and lack of energy.
The symptoms of angina can be similar to the symptoms of a heart attack. Angina pain usually lasts for only a few minutes and goes away with rest.
Chest pain or discomfort that doesn’t go away or changes from its usual pattern (for example, occurs more often or while you’re resting) can be a sign of a heart attack. If you don’t know whether your chest pain is angina or a heart attack, call 9–1–1.
Let the people you see regularly know you're at risk for a heart attack. They can seek emergency care for you if you suddenly faint, collapse, or have other severe symptoms.
Living with CHD may cause fear, anxiety, depression, and stress. You may worry about heart problems or making lifestyle changes that are necessary for your health.
Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to living with CHD. You can see how other people who have the same symptoms have coped with them. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has helped doctors learn more about coronary heart disease (CHD), its risk factors, and ways to prevent and treat the disease.
The NHLBI continues to support research aimed at learning more about CHD. For example, NHLBI-supported research includes studies that:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they’re widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don’t directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You’ll learn about treatments and tests you may receive, and the benefits and risks they may pose. You’ll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you’ll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to CHD, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI’s Children and Clinical Studies Web page.
Source: National Heart, Lung, & Blood Institute, NIH
Risk Factors: What Are Coronary Heart Disease Risk Factors?
Coronary heart disease risk factors are conditions or habits that raise your risk of coronary heart disease (CHD) and heart attack. These risk factors also increase the chance that existing CHD will worsen.
CHD, also called coronary artery disease, is a condition in which a waxy substance called plaque (plak) builds up on the inner walls of the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
Plaque narrows the arteries and reduces blood flow to your heart muscle. Reduced blood flow can cause chest pain, especially when you're active. Eventually, an area of plaque can rupture (break open). This causes a blood clot to form on the surface of the plaque.
If the clot becomes large enough, it can block the flow of oxygen-rich blood to the portion of heart muscle fed by the artery. Blocked blood flow to the heart muscle causes a heart attack.
There are many known CHD risk factors. You can control some risk factors, but not others. Risk factors you can control include:
The risk factors you can't control are age, gender, and family history of CHD.
Many people have at least one CHD risk factor. Your risk of CHD and heart attack increases with the number of risk factors you have and their severity. Also, some risk factors put you at greater risk of CHD and heart attack than others. Examples of these risk factors include smoking and diabetes.
Many CHD risk factors start during childhood. This is even more common now because many children are overweight and don't get enough physical activity. Some CHD risk factors can even develop within the first 10 years of life.
Researchers continue to study and learn more about CHD risk factors.
Following a healthy lifestyle can help you and your children prevent or control many CHD risk factors.
Because many lifestyle habits begin during childhood, parents and families should encourage their children to make heart healthy choices. For example, you and your children can lower your risk of CHD if you maintain a healthy weight, follow a healthy diet, do physical activity regularly, and don't smoke.
If you already have CHD, lifestyle changes can help you control your risk factors. This may prevent CHD from worsening. Even if you're in your seventies or eighties, a healthy lifestyle can lower your risk of dying from CHD.
If lifestyle changes aren't enough, your doctor may recommend other treatments to help control your risk factors.
Your doctor can help you find out whether you have CHD risk factors. He or she also can help you create a plan for lowering your risk of CHD, heart attack, and other heart problems.
If you have children, talk with their doctors about their heart health and whether they have CHD risk factors. If they do, ask your doctor to help create a treatment plan to reduce or control these risk factors.
High blood cholesterol is a condition in which your blood has too much cholesterol—a waxy, fat-like substance. The higher your blood cholesterol level, the greater your risk of coronary heart disease (CHD) and heart attack.
Cholesterol travels through the bloodstream in small packages called lipoproteins (LI-po-pro-teens). Two major kinds of lipoproteins carry cholesterol throughout your body:
Many factors affect your cholesterol levels. For example, after menopause, women's LDL cholesterol levels tend to rise, and their HDL cholesterol levels tend to fall. Other factors—such as age, gender, diet, and physical activity—also affect your cholesterol levels.
Healthy levels of both LDL and HDL cholesterol will prevent plaque from building up in your arteries. Routine blood tests can show whether your blood cholesterol levels are healthy. Talk with your doctor about having your cholesterol tested and what the results mean.
Children also can have unhealthy cholesterol levels, especially if they're overweight or their parents have high blood cholesterol. Talk with your child's doctor about testing your child' cholesterol levels.
To learn more about high blood cholesterol and how to manage the condition, go to the Health Topics High Blood Cholesterol article.
Triglycerides are a type of fat found in the blood. Some studies suggest that a high level of triglycerides in the blood may raise the risk of CHD, especially in women.
"Blood pressure" is the force of blood pushing against the walls of your arteries as your heart pumps blood. If this pressure rises and stays high over time, it can damage your heart and lead to plaque buildup.
Blood pressure is measured as systolic (sis-TOL-ik) and diastolic (di-a-STOL-ik) pressures. "Systolic" refers to blood pressure when the heart beats while pumping blood. "Diastolic" refers to blood pressure when the heart is at rest between beats.
You most often will see blood pressure numbers written with the systolic number above or before the diastolic number, such as 120/80 mmHg. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
All levels above 120/80 mmHg raise your risk of CHD. This risk grows as blood pressure levels rise. Only one of the two blood pressure numbers has to be above normal to put you at greater risk of CHD and heart attack.
Often, high blood pressure has no signs or symptoms. However, the condition can be detected using a simple test that involves placing a blood pressure cuff around your arm.
Most adults should have their blood pressure checked at least once a year. If you have high blood pressure, you'll likely need to be checked more often. Talk with your doctor about how often you should have your blood pressure checked.
Children also can develop high blood pressure, especially if they're overweight. Your child's doctor should check your child's blood pressure at each routine checkup.
In children, blood pressure normally rises with age and body size. Newborns often have very low blood pressure numbers, while older teens have numbers similar to adults. The ranges for normal blood pressure and high blood pressure generally are lower for youth than for adults.
Your child should have routine blood pressure checks starting at 3 years of age. To find out whether a child has high blood pressure, a doctor will compare the child's blood pressure numbers to average numbers for his or her age, gender, and height.
Both children and adults are more likely to develop high blood pressure if they're overweight or have diabetes.
For more information about high blood pressure and how to manage the condition, go to the Health Topics High Blood Pressure article.
Diabetes is a disease in which the body's blood sugar level is too high. The two types of diabetes are type 1 and type 2.
In type 1 diabetes, the body's blood sugar level is high because the body doesn't make enough insulin. Insulin is a hormone that helps move blood sugar into cells, where it's used for energy. In type 2 diabetes, the body's blood sugar level is high mainly because the body doesn't use its insulin properly.
Over time, a high blood sugar level can lead to increased plaque buildup in your arteries. Having diabetes doubles your risk of CHD.
Prediabetes is a condition in which your blood sugar level is higher than normal, but not as high as it is in diabetes. If you have prediabetes and don't take steps to manage it, you'll likely develop type 2 diabetes within 10 years. You're also at higher risk of CHD.
Being overweight or obese raises your risk of type 2 diabetes. With modest weight loss and moderate physical activity, people who have prediabetes may be able to delay or prevent type 2 diabetes. They also may be able to lower their risk of CHD and heart attack. Weight loss and physical activity also can help control diabetes.
Even children can develop type 2 diabetes. Most children who have type 2 diabetes are overweight.
Type 2 diabetes develops over time and sometimes has no symptoms. Go to your doctor or local clinic to have your blood sugar levels tested regularly to check for diabetes and prediabetes.
For more information about diabetes and heart disease, go to the Health Topics Diabetic Heart Disease article. For more information about diabetes and prediabetes, go to the National Institute of Diabetes and Digestive and Kidney Diseases' (NIDDK's) Introduction to Diabetes.
The terms "overweight" and "obesity" refer to body weight that's greater than what is considered healthy for a certain height. More than two-thirds of American adults are overweight, and almost one-third of these adults are obese.
The most useful measure of overweight and obesity is body mass index (BMI). BMI is calculated from your height and weight. In adults, a BMI of 18.5 to 24.9 is considered normal. A BMI of 25 to 29.9 is considered overweight. A BMI of 30 or more is considered obese.
You can use the National Heart, Lung, and Blood Institute's (NHLBI's) online BMI calculator to figure out your BMI, or your doctor can help you.
Overweight is defined differently for children and teens than it is for adults. Children are still growing, and boys and girls mature at different rates. Thus, BMIs for children and teens compare their heights and weights against growth charts that take age and gender into account. This is called BMI-for-age percentile.
For more information about BMI-for-age percentile, go to the Centers for Disease Control and Prevention's (CDC's) BMI-for-age calculator.
Being overweight or obese can raise your risk of CHD and heart attack. This is mainly because overweight and obesity are linked to other CHD risk factors, such as high blood cholesterol and triglyceride levels, high blood pressure, and diabetes.
For more information, go to the Health Topics Overweight and Obesity article.
Smoking tobacco or long-term exposure to secondhand smoke raises your risk of CHD and heart attack.
Smoking triggers a buildup of plaque in your arteries. Smoking also increases the risk of blood clots forming in your arteries. Blood clots can block plaque-narrowed arteries and cause a heart attack.
Some research shows that smoking raises your risk of CHD in part by lowering HDL cholesterol levels.
The more you smoke, the greater your risk of heart attack. Studies show that if you quit smoking, you cut your risk of heart attack in half within a year. The benefits of quitting smoking occur no matter how long or how much you've smoked.
Most people who smoke start when they're teens. Parents can help prevent their children from smoking by not smoking themselves. Talk with your child about the health dangers of smoking and ways to overcome peer pressure to smoke.
For more information, including tips on how to quit smoking, go to the Health Topics Smoking and Your Heart article and the NHLBI's "Your Guide to a Healthy Heart."
For more information about children and smoking, go to the U.S. Department of Health and Human Services' (HHS') Kids and Smoking Web page and the CDC's Smoking and Tobacco Use Web page.
Inactive people are nearly twice as likely to develop CHD as those who are active. A lack of physical activity can worsen other CHD risk factors, such as high blood cholesterol and triglyceride levels, high blood pressure, diabetes and prediabetes, and overweight and obesity.
It's important for children and adults to make physical activity part of their daily routines. One reason many Americans aren't active enough is because of hours spent in front of TVs and computers doing work, schoolwork, and leisure activities.
Some experts advise that children and teens should reduce screen time because it limits time for physical activity. They recommend that children aged 2 and older should spend no more than 2 hours a day watching TV or using a computer (except for school work).
Being physically active is one of the most important things you can do to keep your heart healthy. The good news is that even modest amounts of physical activity are good for your health. The more active you are, the more you will benefit.
For more information, go to HHS' "2008 Physical Activity Guidelines for Americans," the Health Topics Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
An unhealthy diet can raise your risk of CHD. For example, foods that are high in saturated and trans fats and cholesterol raise LDL cholesterol. Thus, you should try to limit these foods.
Saturated fats are found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods. Trans fats are found in some fried and processed foods. Cholesterol is found in eggs, many meats, dairy products, commercial baked goods, and certain types of shellfish.
It's also important to limit foods that are high in sodium (salt) and added sugars. A high-salt diet can raise your risk of high blood pressure.
Added sugars will give you extra calories without nutrients like vitamins and minerals. This can cause you to gain weight, which raises your risk of CHD. Added sugars are found in many desserts, canned fruits packed in syrup, fruit drinks, and nondiet sodas.
You also should try to limit how much alcohol you drink. Too much alcohol will raise your blood pressure. It also will add calories, which can cause weight gain.
Stress and anxiety may play a role in causing CHD. Stress and anxiety also can trigger your arteries to tighten. This can raise your blood pressure and your risk of heart attack.
The most commonly reported trigger for a heart attack is an emotionally upsetting event, especially one involving anger. Stress also may indirectly raise your risk of CHD if it makes you more likely to smoke or overeat foods high in fat and sugar.
As you get older, your risk of CHD and heart attack rises. This is in part due to the slow buildup of plaque inside your heart arteries, which can start during childhood.
In men, the risk of CHD increases faster after age 45. In women, the risk of CHD increases faster after age 55.
Most people have some plaque buildup in their heart arteries by the time they're in their seventies. However, only about 25 percent of those people have chest pain, heart attacks, or other signs of CHD.
Before age 55, women have a lower risk of CHD than men. This is because before menopause, estrogen provides women some protection against CHD. After age 55, however, the risk of CHD increases similarly in both women and men.
Some risk factors may affect CHD risk differently in women than in men. For example, diabetes raises the risk of CHD more in women.
Also, some risk factors for heart disease only affect women, such as preeclampsia (pre-e-KLAMP-se-ah). Preeclampsia is a condition that can develop during pregnancy. The two main signs of preeclampsia are a rise in blood pressure and excess protein in the urine.
Preeclampsia is linked to an increased lifetime risk of heart disease, including CHD, heart attack, heart failure, and high blood pressure. (Likewise, having heart disease risk factors, such as diabetes or obesity, increases your risk of preeclampsia.)
Family history plays a role in CHD risk. Your risk increases if your father or a brother was diagnosed with CHD before 55 years of age, or if your mother or a sister was diagnosed with CHD before 65 years of age.
However, having a family history of CHD doesn't mean that you will have it too. This is especially true if your affected family member smoked or had other CHD risk factors that were not well treated.
Making lifestyle changes and taking medicines to treat other risk factors often cen lessen genetic influences and stop or slow the progress of CHD.
You can prevent and control many coronary heart disease (CHD) risk factors with lifestyle changes and medicines. Examples of these controllable risk factors include high blood cholesterol, high blood pressure, and overweight and obesity. Only a few risk factors—such as age, gender, and family history—can't be controlled.
To reduce your risk of CHD and heart attack, try to control each risk factor you can. The good news is that many lifestyle changes help control several CHD risk factors at the same time. For example, physical activity may lower your blood pressure, help control diabetes and prediabetes, reduce stress, and help control your weight.
Many lifestyle habits begin during childhood. Thus, parents and families should encourage their children to make heart healthy choices, such as following a healthy diet and being physically active. Make following a healthy lifestyle a family goal.
To achieve this goal, you should learn about key health measures, such as weight, body mass index (BMI), waist circumference, and your child's BMI-for-age percentile. For more information about BMI in adults and children, go to "Coronary Heart Disease Risk Factors."
Be aware of your and your family members' blood pressure, blood cholesterol, and blood sugar levels. Once you know these numbers, you can work to bring them into, or keep them within, a healthy range.
Making lifestyle changes can be hard. But if you make these changes as a family, it may be easier for everyone to prevent or control their CHD risk factors.
For tips on how to help your children adopt healthy habits, visit the National Heart, Lung, and Blood Institute's (NHLBI's) We Can!® Ways to Enhance Children's Activity & Nutrition Web site.
A healthy lifestyle can lower the risk of CHD. If you already have CHD, a healthy lifestyle may prevent it from getting worse. A healthy lifestyle includes:
A healthy diet is an important part of a healthy lifestyle. To lower your risk of CHD and heart attack, you and your family should follow a diet that is:
Research suggests that drinking small to moderate amounts of alcohol regularly also can lower your risk of CHD. One drink a day can lower your risk by raising your high-density lipoprotein (HDL), or "good," cholesterol level. One drink is a glass of wine, beer, or a small amount of hard liquor.
If you don't drink, this isn't a recommendation to start using alcohol. If you're pregnant, if you're planning to become pregnant, or if you have another health condition that could make alcohol use harmful, you shouldn't drink.
Also, too much alcohol can cause you to gain weight and raise your blood pressure and triglyceride level. In women, even one drink a day may raise the risk of certain types of cancer.
Teach your children how to make healthy food choices. For example, have them help you shop for and make healthy foods. Set a good example by following the same heart healthy diet that you ask your children to follow.
For more information about following a healthy diet, go to the NHLBI's Aim for a Healthy Weight Web site, "Your Guide to a Healthy Heart," "Your Guide to Lowering Your Blood Pressure With DASH," and "Your Guide to Lowering Your Cholesterol With TLC." All of these resources provide general information about healthy eating.
You don't have to be an athlete to lower your risk of CHD. You can benefit from as little as 60 minutes of moderate-intensity aerobic activity per week.
For major health benefits, adults should do at least 150 minutes (2.5 hours) of moderate-intensity aerobic activity or 75 minutes (1 hour and 15 minutes) of vigorous-intensity aerobic activity each week.
Another option is to do a combination of both. A general rule is that 2 minutes of moderate-intensity activity counts the same as 1 minute of vigorous-intensity activity.
The more active you are, the more you'll benefit. If you're obese, or if you haven't been active in the past, start physical activity slowly and build up the intensity over time.
Children and youth should do 60 minutes or more of physical activity every day. A great way to encourage physical activity is to do it as a family. You also may want to limit your children's TV, video, and computer time to encourage them to be more active.
If you have CHD or symptoms such as chest pain and dizziness, talk with your doctor before you start a new exercise plan. Find out how much and what kinds of physical activity are safe for you. Avoid exercising outdoors when air pollution levels are high or the temperature is very hot or cold.
For more information about physical activity, go to the U.S. Department of Health and Human Services' (HHS') "2008 Physical Activity Guidelines for Americans," the Health Topics Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Following a healthy diet and being physically active can help you maintain a healthy weight. Controlling your weight helps you control CHD risk factors.
If you're overweight or obese, try to lose weight. A loss of just 5 to 10 percent of your current weight can lower your risk of CHD.
To lose weight, cut back your calorie intake and do more physical activity. Eat smaller portions and choose lower calorie foods. Don't feel that you have to finish the entrees served at restaurants. Many restaurant portions are oversized and have too many calories for the average person.
For overweight children and teens, slowing the rate of weight gain is important. However, reduced-calorie diets aren't advised, unless approved by a doctor.
If you smoke, quit. Smoking can raise your risk of CHD and heart attack and worsen other CHD risk factors. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
You can help your children avoid smoking or quit smoking. Talk with them about the health effects of smoking. Teach them how to handle peer pressure to smoke.
Teens who have parents who smoke are more likely to smoke themselves. Set a good example by not smoking or quitting smoking. Set firm rules about no tobacco use in your home.
If you have a child who smokes, help him or her create a plan to quit. Offer your child information and resources on how to quit. Stress the natural rewards that come with quitting, such as freedom from addiction, better fitness and sports performance, and improved appearance. Reinforce the decision to quit with praise.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the NHLBI's "Your Guide to a Healthy Heart."
For more information about children and smoking, go to HHS' Kids and Smoking Web page and the Centers for Disease Control and Prevention's Smoking and Tobacco Use Web page.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress.
Physical activity, medicine, and relaxation therapy also can help relieve stress. You may want to consider taking part in a stress management program.
If making lifestyle changes is hard for you, try taking things one step at a time. Learn about the benefits of lifestyle changes. Talk with your doctor, and read some of the resources in "Links to Other Information About Coronary Heart Disease Risk Factors."
Figure out what's stopping you from making or sticking to your lifestyle changes. Try to find ways to overcome these issues. For example, if you're too tired to exercise after work, you may want to try working out before you go to work.
Make a plan to carry out your lifestyle changes that includes specific, realistic goals. Act on your plan and work toward your goals. You may want to do so with the help of a support group or supportive friends and family.
Reward yourself for the gains you've made. Think about what you need to do to maintain your lifestyle changes and avoid unhealthy habits.
Don't give up if you go off your diet or exercise plan or start smoking again. Instead, find out what you need to do to get back on track so you can meet your goals. Many people find that it takes more than one try to make long-term lifestyle changes.
Changing the eating and activity habits of children takes time. Start with small, easy steps. For example, cut out after-dinner snacks or go for an after-dinner walk instead of watching TV.
Set a good example, and try to get your children involved in choosing a new healthy step to take each day. If you make lifestyle changes a group effort, it will make them easier.
Sometimes lifestyle changes aren't enough to control your blood pressure, cholesterol levels, or other CHD risk factors. Your doctor also may prescribe medicines. For example, you may need medicines to:
Take your medicines as prescribed. Don't cut back on the dosage unless your doctor tells you to. If you have side effects or other problems related to your medicines, talk with your doctor. He or she may be able to provide other options.
You should still follow a heart healthy lifestyle, even if you take medicines to control your CHD risk factors.
Source: NHLBI, NIH
In the United States, 1 in 4 women dies from heart disease. In fact, coronary heart disease (CHD)—the most common type of heart disease—is the #1 killer of both men and women in the United States.
Other types of heart disease, such as coronary microvascular disease (MVD) and broken heart syndrome, also pose a risk for women. These disorders, which mainly affect women, are not as well understood as CHD. However, research is ongoing to learn more about coronary MVD and broken heart syndrome.
This article focuses on CHD and its complications. However, it also includes general information about coronary MVD and broken heart syndrome.
CHD is a disease in which plaque (plak) builds up on the inner walls of your coronary arteries. These arteries carry oxygen-rich blood to your heart. When plaque builds up in the arteries, the condition is called atherosclerosis (ath-er-o-skler-O-sis).
Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque can harden or rupture (break open).
Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause chest pain or discomfort called angina (an-JI-nuh or AN-juh-nuh).
If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. This is the most common cause of a heart attack. Over time, ruptured plaque also hardens and narrows the coronary arteries.


Plaque also can develop within the walls of the coronary arteries. Tests that show the insides of the coronary arteries may look normal in people who have this pattern of plaque. Studies are under way to see whether this type of plaque buildup occurs more often in women than in men and why.
In addition to angina and heart attack, CHD can cause other serious heart problems. The disease may lead to heart failure, irregular heartbeats called arrhythmias (ah-RITH-me-ahs), and sudden cardiac arrest (SCA).
Coronary MVD is heart disease that affects the heart's tiny arteries. This disease is also called cardiac syndrome X or nonobstructive CHD. In coronary MVD, the walls of the heart's tiny arteries are damaged or diseased.

Women are more likely than men to have coronary MVD. Many researchers think that a drop in estrogen levels during menopause combined with other heart disease risk factors causes coronary MVD.
Although death rates from heart disease have dropped in the last 30 years, they haven't dropped as much in women as in men. This may be the result of coronary MVD.
Standard tests for CHD are not designed to detect coronary MVD. Thus, test results for women who have coronary MVD may show that they are at low risk for heart disease.
Research is ongoing to learn more about coronary MVD and its causes.
Women are also more likely than men to have a condition called broken heart syndrome. In this recently recognized heart problem, extreme emotional stress can lead to severe (but often short-term) heart muscle failure.
Broken heart syndrome is also called stress-induced cardiomyopathy (KAR-de-o-mi-OP-ah-thee) or takotsubo cardiomyopathy.
Doctors may misdiagnose broken heart syndrome as a heart attack because it has similar symptoms and test results. However, there's no evidence of blocked heart arteries in broken heart syndrome, and most people have a full and quick recovery.
Researchers are just starting to explore what causes this disorder and how to diagnose and treat it. Often, patients who have broken heart syndrome have previously been healthy.
Women tend to have CHD about 10 years later than men. However, CHD remains the #1 killer of women in the United States.
The good news is that you can control many CHD risk factors. CHD risk factors are conditions or habits that raise your risk for CHD and heart attack. These risk factors also can increase the chance that existing CHD will worsen.
Lifestyle changes, medicines, and medical or surgical procedures can help women lower their risk for CHD. Thus, early and ongoing CHD prevention is important.
More information about heart disease in women is available through the National Heart, Lung, and Blood Institute's The Heart Truth® campaign.
®The Heart Truth is a registered trademark of the U.S. Department of Health and Human Services.
Research suggests that coronary heart disease (CHD) begins with damage to the lining and inner layers of the coronary (heart) arteries. Several factors contribute to this damage. They include:
Plaque may begin to build up where the arteries are damaged. The buildup of plaque in the coronary arteries may start in childhood.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause chest pain or discomfort called angina.
If the plaque ruptures, blood cell fragments called platelets (PLATE-lets) stick to the site of the injury. They may clump together to form blood clots.
Blood clots can further narrow the coronary arteries and worsen angina. If a clot becomes large enough, it can mostly or completely block a coronary artery and cause a heart attack.
In addition to the factors above, low estrogen levels before or after menopause may play a role in causing coronary microvascular disease (MVD). Coronary MVD is heart disease that affects the heart's tiny arteries.
The cause of broken heart syndrome isn't yet known. However, a sudden release of stress hormones may play a role in causing the disorder. Most cases of broken heart syndrome occur in women who have gone through menopause.
Certain traits, conditions, or habits may raise your risk for coronary heart disease (CHD). These conditions are known as risk factors. Risk factors also increase the chance that existing CHD will worsen.
Women generally have the same CHD risk factors as men. However, some risk factors may affect women differently than men. For example, diabetes raises the risk of CHD more in women. Also, some risk factors, such as birth control pills and menopause, only affect women.
There are many known CHD risk factors. Your risk for CHD and heart attack rises with the number of risk factors you have and their severity. Risk factors tend to "gang up" and worsen each other's effects.
Having just one risk factor doubles your risk for CHD. Having two risk factors increases your risk for CHD fourfold. Having three or more risk factors increases your risk for CHD more than tenfold.
Also, some risk factors, such as smoking and diabetes, put you at greater risk for CHD and heart attack than others.
More than 75 percent of women aged 40 to 60 have one or more risk factors for CHD. Many risk factors start during childhood; some even develop within the first 10 years of life. You can control most risk factors, but some you can't.
For more information about CHD risk factors, go to the Health Topics Coronary Heart Disease Risk Factors article. To find out whether you're at risk for CHD, talk with your doctor or health care provider.
Smoking is the most powerful risk factor that women can control. Smoking tobacco or long-term exposure to secondhand smoke raises your risk for CHD and heart attack.
Smoking exposes you to carbon monoxide. This chemical robs your blood of oxygen and triggers a buildup of plaque in your arteries.
Smoking also increases the risk of blood clots forming in your arteries. Blood clots can block plaque-narrowed arteries and cause a heart attack. The more you smoke, the greater your risk for a heart attack.
Even women who smoke fewer than two cigarettes a day are at increased risk for CHD.
Cholesterol travels in the bloodstream in small packages called lipoproteins (LI-po-pro-teens). The two major kinds of lipoproteins are low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol.
LDL cholesterol is sometimes called "bad" cholesterol. This is because it carries cholesterol to tissues, including your heart arteries. HDL cholesterol is sometimes called "good" cholesterol. This is because it helps remove cholesterol from your arteries.
A blood test called a lipoprotein panel is used to measure cholesterol levels. This test gives information about your total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides (a type of fat found in the blood).
Cholesterol levels are measured in milligrams (mg) of cholesterol per deciliter (dL) of blood. A woman's risk for CHD increases if she has a total cholesterol level greater than 200 mg/dL, an LDL cholesterol level greater than 100 mg/dL, or an HDL cholesterol level less than 50 mg/dL.
A triglyceride level greater than 150 mg/dL also increases a woman's risk for CHD. A woman's HDL cholesterol and triglyceride levels predict her risk for CHD better than her total cholesterol or LDL cholesterol levels.
Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps blood. If this pressure rises and stays high over time, it can damage the body in many ways.
Women who have blood pressure greater than 120/80 mmHg are at increased risk for CHD. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
High blood pressure is defined differently for people who have diabetes or chronic kidney disease. If you have one of these diseases, work with your doctor to set a healthy blood pressure goal.
Diabetes is a disease in which the body's blood sugar level is too high. This is because the body doesn't make enough insulin or doesn't use its insulin properly.
Insulin is a hormone that helps move blood sugar into cells, where it's used for energy. Over time, a high blood sugar level can lead to increased plaque buildup in your arteries.
Prediabetes is a condition in which your blood sugar level is higher than normal, but not as high as it is in diabetes. Prediabetes puts you at higher risk for both diabetes and CHD.
Diabetes and prediabetes raise the risk of CHD more in women than in men. In fact, having diabetes doubles a woman's risk of developing CHD.
Before menopause, estrogen provides women some protection against CHD. However, in women who have diabetes, the disease counters the protective effects of estrogen.
The terms "overweight" and "obesity" refer to body weight that's greater than what is considered healthy for a certain height.
The most useful measure of overweight and obesity is body mass index (BMI). BMI is calculated from your height and weight. In adults, a BMI of 18.5 to 24.9 is considered normal. A BMI of 25 to 29.9 is considered overweight. A BMI of 30 or more is considered obese.
You can use the National Heart, Lung, and Blood Institute's (NHLBI's) online BMI calculator to figure out your BMI, or your doctor can help you.
Studies suggest that where extra weight occurs on the body may predict CHD risk better than BMI. Women who carry much of their fat around the waist are at greatest risk for CHD. These women have "apple-shaped" figures.
Women who carry most of their fat on their hips and thighs—that is, those who have "pear-shaped" figures—are at lower risk for CHD.
To fully know how excess weight affects your CHD risk, you should know your BMI and waist measurement. If you have a BMI greater than 24.9 and a waist measurement greater than 35 inches, you're at increased risk for CHD.
If your waist measurement divided by your hip measurement is greater than 0.9, you're also at increased risk for CHD.
Studies also suggest that women whose weight goes up and down dramatically (typically due to unhealthy dieting) are at increased risk for CHD. These swings in weight can lower HDL cholesterol levels.
Metabolic syndrome is the name for a group of risk factors that raises your risk for CHD and other health problems, such as diabetes and stroke. A diagnosis of metabolic syndrome is made if you have at least three of the following risk factors:
Metabolic syndrome is more common in African American women and Mexican American women than in men of the same racial groups. The condition affects White women and men about equally.
Women who smoke and take birth control pills are at very high risk for CHD, especially if they're older than 35. For women who take birth control pills but don't smoke, the risk of CHD isn't fully known.
Inactive people are nearly twice as likely to develop CHD as those who are physically active. A lack of physical activity can worsen other CHD risk factors, such as high blood cholesterol and triglyceride levels, high blood pressure, diabetes and prediabetes, and overweight and obesity.
An unhealthy diet can raise your risk for CHD. For example, foods that are high in saturated and trans fats and cholesterol raise your LDL cholesterol level. A high-sodium (salt) diet can raise your risk for high blood pressure.
Foods with added sugars will give you extra calories without nutrients, such as vitamins and minerals. This can cause you to gain weight, which raises your risk for CHD.
Too much alcohol also can cause you to gain weight, and it will raise your blood pressure.
Stress may play a role in causing CHD. Stress can trigger your arteries to narrow. This can raise your blood pressure and your risk for a heart attack.
Getting upset or angry also can trigger a heart attack. Stress also may indirectly raise your risk for CHD if it makes you more likely to smoke or overeat foods high in fat and sugar.
People who are depressed are two to three times more likely to develop CHD than people who are not. Depression is twice as common in women as in men.
Anemia (uh-NEE-me-eh) is a condition in which your blood has a lower than normal number of red blood cells.
The condition also can occur if your red blood cells don't contain enough hemoglobin (HEE-muh-glow-bin). Hemoglobin is an iron-rich protein that carries oxygen from your lungs to the rest of your organs.
If you have anemia, your organs don't get enough oxygen-rich blood. This causes your heart to work harder, which may raise your risk for CHD.
Anemia has many causes. For more information, go to the Health Topics Anemia article.
Sleep apnea is a common disorder that causes pauses in breathing or shallow breaths while you sleep. Breathing pauses can last from a few seconds to minutes. They often occur 5 to 30 times or more an hour.
Typically, normal breathing starts again after the pause, sometimes with a loud snort or choking sound. Major signs of sleep apnea are snoring and daytime sleepiness.
When you stop breathing, the lack of oxygen triggers your body's stress hormones. This causes blood pressure to rise and makes the blood more likely to clot.
Untreated sleep apnea can raise your risk for high blood pressure, diabetes, and even a heart attack or stroke.
Women are more likely to develop sleep apnea after menopause.
As you get older, your risk for CHD and heart attack rises. This is due in part to the slow buildup of plaque inside your heart arteries, which can start during childhood.
Before age 55, women have a lower risk for CHD than men. Estrogen provides women with some protection against CHD before menopause. After age 55, however, the risk of CHD increases in both women and men.
You may have gone through early menopause, either naturally or because you had your ovaries removed. If so, you're twice as likely to develop CHD as women of the same age who aren't yet menopausal.
Another reason why women are at increased risk for CHD after age 55 is that middle age is when you tend to develop other CHD risk factors.
Women who have gone through menopause also are at increased risk for broken heart syndrome. (For more information, go to the section on emerging risk factors below.)
Family history plays a role in CHD risk. Your risk increases if your father or a brother was diagnosed with CHD before 55 years of age, or if your mother or a sister was diagnosed with CHD before 65 years of age.
Also, a family history of stroke—especially a mother's stroke history—can help predict the risk of heart attack in women.
Having a family history of CHD or stroke doesn't mean that you'll develop heart disease. This is especially true if your affected family member smoked or had other risk factors that were not well treated.
Making lifestyle changes and taking medicines to treat risk factors often can lessen genetic influences and prevent or delay heart problems.
Preeclampsia (pre-e-KLAMP-se-ah) is a condition that develops during pregnancy. The two main signs of preeclampsia are a rise in blood pressure and excess protein in the urine.
These signs usually occur during the second half of pregnancy and go away after delivery. However, your risk of developing high blood pressure later in life increases after having preeclampsia.
Preeclampsia also is linked to an increased lifetime risk of heart disease, including CHD, heart attack, and heart failure. (Likewise, having heart disease risk factors, such as diabetes or obesity, increases your risk for preeclampsia.)
If you had preeclampsia during pregnancy, you're twice as likely to develop heart disease as women who haven't had the condition. You're also more likely to develop heart disease earlier in life.
Preeclampsia is a heart disease risk factor that you can't control. However, if you've had the condition, you should take extra care to try and control other heart disease risk factors.
The more severe your preeclampsia was, the greater your risk for heart disease. Let your doctor know that you had preeclampsia so he or she can assess your heart disease risk and how to reduce it.
Research suggests that inflammation plays a role in causing CHD. Inflammation is the body's response to injury or infection. Damage to the arteries' inner walls seems to trigger inflammation and help plaque grow.
High blood levels of a protein called C-reactive protein (CRP) are a sign of inflammation in the body. Research suggests that women who have high blood levels of CRP are at increased risk for heart attack.
Also, some inflammatory diseases, such as lupus and rheumatoid arthritis, may increase the risk for CHD.
Some studies suggest that women who have migraine headaches may be at greater risk for CHD. This is especially true for women who have migraines with auras (visual disturbances), such as flashes of light or zig-zag lines.
Low bone density and low intake of folate and vitamin B6 also may raise a woman's risk for CHD.
More research is needed to find out whether calcium supplements with or without vitamin D affect CHD risk. You may want to talk with your doctor to find out whether these types of supplements are right for you.
Researchers are just starting to learn about broken heart syndrome risk factors. Most women who have this disorder are White and have gone through menopause.
Many of these women have other heart disease risk factors, such as high blood pressure, high blood cholesterol, diabetes, and smoking. However, these risk factors tend to be less common in women who have broken heart syndrome than in women who have CHD.

The signs and symptoms of coronary heart disease (CHD) may differ between women and men. Some women who have CHD have no signs or symptoms. This is called silent CHD.
Silent CHD may not be diagnosed until a woman has signs and symptoms of a heart attack, heart failure, or an arrhythmia (irregular heartbeat).
Other women who have CHD will have signs and symptoms of the disease.
A common symptom of CHD is angina. Angina is chest pain or discomfort that occurs when your heart muscle doesn't get enough oxygen-rich blood.
In men, angina often feels like pressure or squeezing in the chest. This feeling may extend to the arms. Women can also have these angina symptoms. But women also tend to describe a sharp, burning chest pain. Women are more likely to have pain in the neck, jaw, throat, abdomen, or back.
In men, angina tends to worsen with physical activity and go away with rest. Women are more likely than men to have angina while they're resting or sleeping.
In women who have coronary microvascular disease, angina often occurs during routine daily activities, such as shopping or cooking, rather than while exercising. Mental stress also is more likely to trigger angina pain in women than in men.
The severity of angina varies. The pain may get worse or occur more often as the buildup of plaque continues to narrow the coronary (heart) arteries.
The most common heart attack symptom in men and women is chest pain or discomfort. However, only half of women who have heart attacks have chest pain.
Women are more likely than men to report back or neck pain, indigestion, heartburn, nausea (feeling sick to the stomach), vomiting, extreme fatigue (tiredness), or problems breathing.
Heart attacks also can cause upper body discomfort in one or both arms, the back, neck, jaw, or upper part of the stomach. Other heart attack symptoms are light-headedness and dizziness, which occur more often in women than men.
Men are more likely than women to break out in a cold sweat and to report pain in the left arm during a heart attack.
Heart failure is a condition in which your heart can't pump enough blood to meet your body's needs. Heart failure doesn't mean that your heart has stopped or is about to stop working. It means that your heart can't cope with the demands of everyday activities.
Heart failure causes shortness of breath and fatigue that tends to increase with physical exertion. Heart failure also can cause swelling in the feet, ankles, legs, abdomen, and veins in the neck.
An arrhythmia is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
Some people describe arrhythmias as fluttering or thumping feelings or skipped beats in their chests. These feelings are called palpitations.
Some arrhythmias can cause your heart to suddenly stop beating. This condition is called sudden cardiac arrest (SCA). SCA causes loss of consciousness and death if it's not treated right away.
The most common signs and symptoms of broken heart syndrome are chest pain and shortness of breath. In this disorder, these symptoms tend to occur suddenly in people who have no history of heart disease.
Arrhythmias or cardiogenic shock also may occur. Cardiogenic shock is a condition in which a suddenly weakened heart isn't able to pump enough blood to meet the body's needs.
Some of the signs and symptoms of broken heart syndrome differ from those of heart attack. For example, in people who have broken heart syndrome:
Your doctor will diagnose coronary heart disease (CHD) based on your medical and family histories, your risk factors, a physical exam, and the results from tests and procedures.
No single test can diagnose CHD. If your doctor thinks you have CHD, he or she may recommend one or more of the following tests.
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage due to CHD and signs of a previous or current heart attack.
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can't exercise, you may be given medicines to increase your heart rate.
When your heart is working hard and beating fast, it needs more blood and oxygen. Plaque-narrowed coronary (heart) arteries can't supply enough oxygen-rich blood to meet your heart's needs.
A stress test can show possible signs and symptoms of CHD, such as:
If you can't exercise for as long as what is considered normal for someone your age, your heart may not be getting enough oxygen-rich blood. However, other factors also can prevent you from exercising long enough (for example, lung diseases, anemia, or poor general fitness).
As part of some stress tests, pictures are taken of your heart while you exercise and while you rest. These imaging stress tests can show how well blood is flowing in your heart and how well your heart pumps blood when it beats.
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test provides information about the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can show areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
A chest x ray creates pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels.
A chest x ray can reveal signs of heart failure, as well as lung disorders and other causes of symptoms not related to CHD.
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may be a sign that you're at risk for CHD. Blood tests also help detect anemia, a risk factor for CHD.
During a heart attack, heart muscle cells die and release proteins into the bloodstream. Blood tests can measure the amount of these proteins in the bloodstream. High levels of these proteins are a sign of a recent heart attack.
Your doctor may recommend coronary angiography (an-jee-OG-rah-fee) if other tests or factors suggest you have CHD. This test uses dye and special x rays to look inside your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-eh-ter-ih-ZA-shun).
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through your coronary arteries. The dye lets your doctor study the flow of blood through your heart and blood vessels.
Coronary angiography detects blockages in the large coronary arteries. However, the test doesn't detect coronary microvascular disease (MVD). This is because coronary MVD doesn't cause blockages in the large coronary arteries.
Even if the results of your coronary angiography are normal, you may still have chest pain or other CHD symptoms. If so, talk with your doctor about whether you might have coronary MVD.
Your doctor may ask you to fill out a questionnaire called the Duke Activity Status Index. This questionnaire measures how easily you can do routine tasks. It gives your doctor information about how well blood is flowing through your coronary arteries.
Your doctor also may recommend other tests that measure blood flow in the heart, such as a cardiac MRI (magnetic resonance imaging) stress test.
Cardiac MRI uses radio waves, magnets, and a computer to create pictures of your heart as it beats. The test produces both still and moving pictures of your heart and major blood vessels.
Other tests done during cardiac catheterization can check blood flow in the heart's small arteries and the thickness of the artery walls.
If your doctor thinks you have broken heart syndrome, he or she may recommend coronary angiography. Other tests are also used to diagnose this disorder, including blood tests, EKG, echo, and cardiac MRI.
Treatment for coronary heart disease (CHD) usually is the same for both women and men. Treatment may include lifestyle changes, medicines, medical and surgical procedures, and cardiac rehabilitation (rehab).
The goals of treatment are to:
Making lifestyle changes can help prevent or treat CHD. These changes may be the only treatment that some people need.
If you smoke or use tobacco, try to quit. Smoking can raise your risk for CHD and heart attack and worsen other CHD risk factors. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
If you find it hard to quit smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's (NHLBI's) "Your Guide to a Healthy Heart."
A healthy diet is an important part of a healthy lifestyle. A healthy diet includes a variety of vegetables and fruits. These foods can be fresh, canned, frozen, or dried. A good rule is to try to fill half of your plate with vegetables and fruits.
A healthy diet also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
Choose and prepare foods with little sodium (salt). Too much salt can raise your risk for high blood pressure. Studies show that following the Dietary Approaches to Stop Hypertension (DASH) eating plan can lower blood pressure.
Try to avoid foods and drinks that are high in added sugars. For example, drink water instead of sugary drinks, like soda.
Also, try to limit the amount of solid fats and refined grains that you eat. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
If you drink alcohol, do so in moderation. Research suggests that regularly drinking small to moderate amounts of alcohol may lower the risk of CHD. Women should have no more than one alcoholic drink a day.
One drink a day can lower your CHD risk by raising your HDL cholesterol level. One drink is a glass of wine, beer, or a small amount of hard liquor.
If you don't drink, this isn't a recommendation to start using alcohol. Also, you shouldn't drink if you're pregnant, if you're planning to become pregnant, or if you have another health condition that could make alcohol use harmful.
Too much alcohol can cause you to gain weight and raise your blood pressure and triglyceride level. In women, even one drink a day may raise the risk of certain types of cancer.
For more information about following a healthy diet, go to the NHLBI's "Your Guide to Lowering Your Blood Pressure With DASH" and the U.S. Department of Agriculture's ChooseMyPlate.gov Web site. Both resources provide general information about healthy eating.
Regular physical activity can lower many CHD risk factors, including high LDL cholesterol, high blood pressure, and excess weight.
Physical activity also can lower your risk for diabetes and raise your HDL cholesterol level. (HDL cholesterol helps remove cholesterol from your arteries.)
Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. Walking is an excellent heart healthy exercise. The more active you are, the more you will benefit.
For more information about physical activity, go to the U.S. Department of Health and Human Services' "2008 Physical Activity Guidelines for Americans," the Health Topics Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Overweight and obesity are risk factors for CHD. If you're overweight or obese, try to lose weight. Cut back your calorie intake and do more physical activity. Eat smaller portions and choose lower calorie foods. Your health care provider may refer you to a dietitian to help you manage your weight.
A BMI of less than 25 and a waist circumference of 35 inches or less is the goal for preventing and treating CHD. BMI measures your weight in relation to your height and gives an estimate of your total body fat. You can use the NHLBI's online BMI calculator to figure out your BMI, or your doctor can help you.
To measure your waist, stand and place a tape measure around your middle, just above your hipbones. Measure your waist just after you breathe out. Make sure the tape is snug but doesn't squeeze the flesh.
For more information about losing weight or maintaining a healthy weight, go to the NHLBI's Aim for a Healthy Weight Web site.
Research shows that getting upset or angry can trigger a heart attack. Also, some of the ways people cope with stress—such as drinking, smoking, or overeating—aren't heart healthy.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health.
Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress. Physical activity, yoga, and relaxation therapy also can help relieve stress. You may want to consider taking part in a stress management program.
Depression can double or triple your risk for CHD. Depression also makes it hard to maintain a heart healthy lifestyle.
Talk with your doctor if you have symptoms of depression, such as feeling hopeless or not taking interest in daily activities. He or she may recommend counseling or prescribe medicines to help you manage the condition.
You may need medicines to treat CHD if lifestyle changes aren't enough. Medicines can help:
Women who have coronary microvascular disease and anemia may benefit from taking medicine to treat the anemia.
Women who have broken heart syndrome also may need medicines. Doctors may prescribe medicines to relieve fluid buildup, treat blood pressure problems, prevent blood clots, and manage stress hormones. Most people who have broken heart syndrome make a full recovery within weeks.
Take all of your medicines as prescribed. If you have side effects or other problems related to your medicines, tell your doctor. He or she may be able to provide other options.
Recent studies have shown that menopausal hormone therapy (MHT) doesn't prevent CHD. Some studies have even shown that MHT increases women's risk for CHD, stroke, and breast cancer.
However, these studies tested MHT on women who had been postmenopausal for at least several years. During that time, they could have already developed CHD.
Research is ongoing to see whether MHT helps prevent CHD when taken right when menopause starts. While questions remain, current findings suggest MHT shouldn't routinely be used to prevent or treat CHD.
Ask your doctor about other ways to prevent or treat CHD, including lifestyle changes and medicines. For more information about MHT, go to the NHLBI's Postmenopausal Hormone Therapy Web site.
You may need a procedure or surgery to treat CHD. Both angioplasty and CABG are used as treatments. You and your doctor can discuss which treatment is right for you.
Percutaneous coronary intervention (PCI), commonly known as angioplasty (AN-jee-oh-plas-tee), is a nonsurgical procedure that opens blocked or narrowed coronary arteries.
A thin, flexible tube with a balloon or other device on the end is threaded through a blood vessel to the narrowed or blocked coronary artery. Once in place, the balloon is inflated to compress the plaque against the wall of the artery. This restores blood flow through the artery.
PCI can improve blood flow to your heart and relieve chest pain. A small mesh tube called a stent usually is placed in the artery to help keep it open after the procedure.
For more information, go to the Health Topics PCI article.
CABG is a type of surgery. During CABG, a surgeon removes arteries or veins from other areas in your body and uses them to bypass (that is, go around) narrowed or blocked coronary arteries.
CABG can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
For more information, go to the Health Topics Coronary Artery Bypass Grafting article.
Your doctor may prescribe cardiac rehab for angina or after angioplasty, CABG, or a heart attack. Almost everyone who has CHD can benefit from cardiac rehab.
Cardiac rehab is a medically supervised program that can improve the health and well-being of people who have heart problems.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians or nutritionists, and psychologists or other mental health specialists.
Cardiac rehab has two parts:
For more information, go to the Health Topics Cardiac Rehabilitation article.
Taking action to control your risk factors can help prevent or delay coronary heart disease (CHD). Your risk for CHD increases with the number of CHD risk factors you have.
One step you can take is to adopt a heart healthy lifestyle. A heart healthy lifestyle should be part of a lifelong approach to healthy living.
For example, if you smoke, try to quit. Smoking can raise your risk for CHD and heart attack and worsen other CHD risk factors. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
For more information about quitting smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's (NHLBI's) "Your Guide to a Healthy Heart."
Following a healthy diet also is an important part of a healthy lifestyle. A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
The NHLBI's Therapeutic Lifestyle Changes (TLC) and Dietary Approaches to Stop Hypertension (DASH) are two programs that promote healthy eating.
If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan. Controlling your weight helps you control CHD risk factors.
Be as physically active as you can. Physical activity can improve your fitness level and your health. Talk with your doctor about what types of activity are safe for you.
For more information about physical activity, go to the Health Topics Physical Activity and Your Heart article and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Know your family history of CHD. If you or someone in your family has CHD, be sure to tell your doctor.
If lifestyle changes aren't enough, you also may need medicines to control your CHD risk factors. Take all of your medicines as prescribed.
For more information about lifestyle changes and medicines, go to "How Is Heart Disease Treated?"
If you have coronary heart disease (CHD), you can take steps to control its risk factors and prevent complications. Lifestyle changes and ongoing care can help you manage the disease.
Having CHD raises your risk for a heart attack. Thus, knowing the warning signs of a heart attack is important. If you think you're having a heart attack, call 9–1–1 right away. For more detailed information about heart attack warning signs, go to the section on warning signs below.
Adopting a heart healthy lifestyle can help you control CHD risk factors. However, making lifestyle changes can be a challenge.
Try to take things one step at a time. Learn about the benefits of lifestyle changes, and make a plan with specific, realistic goals. Reward yourself for your progress.
The good news is that many lifestyle changes help control several CHD risk factors at the same time. For example, physical activity lowers your blood pressure and LDL cholesterol level, helps control diabetes and prediabetes, reduces stress, and helps control your weight.
For more information about adopting a heart healthy lifestyle, go to the section of this article titled "How Is Heart Disease Treated?" You also can visit the Health Topics Coronary Heart Disease Risk Factors article for more information.
Your CHD risk factors can change over time, so having ongoing care is important. Your doctor will track your blood pressure, blood cholesterol, and blood sugar levels with routine tests. These tests will show whether your doctor needs to adjust your treatment.
Ask your doctor how often you should schedule followup visits and blood tests. Between visits, call your doctor if you have any new symptoms or if your symptoms worsen.
You may feel depressed or anxious if you've been diagnosed with CHD. You may worry about heart problems or making lifestyle changes.
Your doctor may recommend medicine, professional counseling, or relaxation therapy if you have depression or anxiety. It's important to treat these conditions because they raise your risk for CHD and heart attack. Depression and anxiety also can make it harder for you to make lifestyle changes.
If you have CHD, learn the warning signs of a heart attack. Heart attack signs and symptoms include:
If you think you're having a heart attack, call 9–1–1 at once. Early treatment can prevent or limit damage to your heart muscle.
If you think you're having a heart attack, do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room.
Let the people you see regularly know you're at risk for a heart attack. They can seek emergency care if you suddenly faint, collapse, or have other severe symptoms.
Most people who have broken heart syndrome make a full recovery within weeks. The risk is low for a repeat episode of this disorder.
To check your heart health, your doctor may recommend echocardiography about a month after you're diagnosed with the syndrome. Talk with your doctor about how often you should schedule followup visits.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to a better understanding of how heart disease affects women. Research also has helped doctors learn more about heart disease, its risk factors, and ways to prevent and treat the disease.
The NHLBI continues to support research aimed at learning more about heart disease. For example, NHLBI-supported research includes studies that:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart disease, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
Source: NHLBI, NIH
Coronary microvascular disease (MVD) is heart disease that affects the tiny coronary (heart) arteries. In coronary MVD, the walls of the heart's tiny arteries are damaged or diseased.
Coronary MVD is different from traditional coronary heart disease (CHD), also called coronary artery disease. In CHD, a waxy substance called plaque (plak) builds up in the large coronary arteries.
Plaque narrows the heart's large arteries and reduces the flow of oxygen-rich blood to your heart muscle. The buildup of plaque also makes it more likely that blood clots will form in your arteries. Blood clots can mostly or completely block blood flow through a coronary artery.
In coronary MVD, however, the heart's tiny arteries are affected. Plaque doesn't create blockages in these vessels as it does in the heart's large arteries.

Studies have shown that women are more likely than men to have coronary MVD. Many researchers think the disease is caused by a drop in estrogen levels during menopause combined with traditional heart disease risk factors.
Both men and women who have coronary MVD often have diabetes or high blood pressure. Some people who have coronary MVD may have inherited heart muscle diseases.
Diagnosing coronary MVD has been a challenge for doctors. Standard tests used to diagnose CHD aren't designed to detect coronary MVD. More research is needed to find the best diagnostic tests and treatments for the disease.
Most of what is known about coronary MVD comes from the National Heart, Lung, and Blood Institute's Wise study (Women's Ischemia Syndrome Evaluation).
The WISE study started in 1996. The goal of the study was to learn more about how heart disease develops in women.
Currently, research is ongoing to learn more about the role of hormones in heart disease and to find better ways to diagnose coronary MVD.
Studies also are under way to learn more about the causes of coronary MVD, how to treat the disease, and the expected health outcomes for people with coronary MVD.
The same risk factors that cause atherosclerosis (ATH-er-o-skler-O-sis) may cause coronary microvascular disease (MVD). Atherosclerosis is a disease in which plaque builds up inside the arteries.
Risk factors for atherosclerosis include:
In women, coronary MVD also may be linked to low estrogen levels occurring before or after menopause. Also, the disease may be linked to anemia or conditions that affect blood clotting. Anemia is thought to slow the growth of cells needed to repair damaged blood vessels.
Researchers continue to explore other possible causes of coronary MVD.
Studies have shown that women are more likely than men to have coronary microvascular disease (MVD). Women at high risk for the disease often have multiple risk factors for atherosclerosis. (For a detailed list of these risk factors, go to "What Causes Coronary Microvascular Disease?")
Women may be at risk for coronary MVD if they have lower than normal levels of estrogen at any point in their adult lives. (This refers to the estrogen that the ovaries produce, not the estrogen used in hormone therapy.)
Low estrogen levels before menopause can raise younger women's risk for coronary MVD. One cause of low estrogen levels in younger women is mental stress. Another cause is a problem with the function of the ovaries.
Women who have high blood pressure before menopause, especially high systolic blood pressure, are at increased risk for coronary MVD. (Systolic blood pressure is the top or first number of a blood pressure measurement.)
After menopause, women tend to have more of the traditional risk factors for atherosclerosis, which also puts them at higher risk for coronary MVD.
Women who have heart disease are more likely to have a worse outcome, such as a heart attack, if they also have anemia. Anemia is thought to slow the growth of cells needed to repair damaged blood vessels.
The signs and symptoms of coronary microvascular disease (MVD) often differ from the signs and symptoms of traditional coronary heart disease (CHD).
Many women with coronary MVD have angina (an-JI-nuh or AN-juh-nuh). Angina is chest pain or discomfort that occurs when your heart muscle doesn't get enough oxygen-rich blood.
Angina may feel like pressure or squeezing in your chest. You also may feel it in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion.
Angina also is a common symptom of CHD. However, the angina that occurs in coronary MVD may differ from the typical angina that occurs in CHD. In coronary MVD, the chest pain usually lasts longer than 10 minutes, and it can last longer than 30 minutes. Typical angina is more common in women older than 65.
Other signs and symptoms of coronary MVD are shortness of breath, sleep problems, fatigue (tiredness), and lack of energy.
Coronary MVD symptoms often are first noticed during routine daily activities (such as shopping, cooking, cleaning, and going to work) and times of mental stress. It's less likely that women will notice these symptoms during physical activity (such as jogging or walking fast).
This differs from CHD, in which symptoms often first appear while a person is being physically active—such as while jogging, walking on a treadmill, or going up stairs.
Your doctor will diagnose coronary microvascular disease (MVD) based on your medical history, a physical exam, and test results. He or she will check to see whether you have any risk factors for heart disease.
For example, your doctor may measure your weight and height to check for overweight or obesity. He or she also may recommend tests for high blood cholesterol, metabolic syndrome, and diabetes.
Your doctor may ask you to describe any chest pain, including when it started and how it changed during physical activity or periods of stress. He or she also may ask about other symptoms, such as fatigue (tiredness), lack of energy, and shortness of breath. Women may be asked about their menopausal status.
Cardiologists and doctors who specialize in family and internal medicine might help diagnose and treat coronary MVD. Cardiologists are doctors who specialize in diagnosing and treating heart diseases and conditions.
The risk factors for coronary MVD and traditional coronary heart disease (CHD) often are the same. Thus, your doctor may recommend tests for CHD, such as:
Unfortunately, standard tests for CHD aren't designed to detect coronary MVD. These tests look for blockages in the large coronary arteries. Coronary MVD affects the tiny coronary arteries.
If test results show that you don't have CHD, your doctor might still diagnose you with coronary MVD. This could happen if signs are present that not enough oxygen is reaching your heart's tiny arteries.
Coronary MVD symptoms often first occur during routine daily tasks. Thus, your doctor may ask you to fill out a questionnaire called the Duke Activity Status Index (DASI). The questionnaire will ask you how well you're able to do daily activities, such as shopping, cooking, and going to work.
The DASI results will help your doctor decide which kind of stress test you should have. The results also give your doctor information about how well blood is flowing through your coronary arteries.
Your doctor also may recommend blood tests, including a test for anemia. Anemia is thought to slow the growth of cells needed to repair damaged blood vessels.
Research is ongoing for better ways to detect and diagnose coronary MVD. Currently, researchers have not agreed on the best way to diagnose the disease.
Relieving pain is one of the main goals of treating coronary microvascular disease (MVD). Treatments also are used to control risk factors and other symptoms.
Treatments may include medicines such as:
If you're diagnosed with coronary MVD and also have anemia, you may benefit from treatment for that condition. Anemia is thought to slow the growth of cells needed to repair damaged blood vessels.
If you're diagnosed with and treated for coronary MVD, you should get ongoing care from your doctor.
Research is under way to find the best treatments for coronary MVD.
No specific studies have been done on how to prevent coronary microvascular disease (MVD).
Researchers don't yet known how or in what way preventing coronary MVD differs from preventing coronary heart disease (CHD). Coronary MVD affects the tiny coronary arteries, while CHD affects the large coronary arteries.
Taking action to control heart disease risk factors can help prevent or delay CHD. You can't control some risk factors, such as older age and family history of heart disease. However, you can take steps to prevent or control other risk factors, such as high blood pressure, overweight and obesity, high blood cholesterol, diabetes, and smoking.
Lifestyle changes and ongoing care can help you lower your risk for heart disease.
Following a healthy diet is an important part of a heart healthy lifestyle. A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
The National Heart, Lung, and Blood Institute's (NHLBI's) Therapeutic Lifestyle Changes (TLC) and Dietary Approaches to Stop Hypertension (DASH) are two programs that promote healthy eating.
If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan. Controlling your weight helps you control heart disease risk factors.
Be as physically active as you can. Physical activity can improve your fitness level and your health. People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. The more active you are, the more you'll benefit.
For more information about physical activity, go to the Health Topics Physical Activity and Your Heart article and the NHLBI's "Your Guide to Physical Activity and Your Heart."
If you smoke, quit. Smoking can damage and tighten your blood vessels. It also can raise your risk for heart disease and heart attack and worsen other heart disease risk factors.
Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke. For more information about quitting smoking, go to the Health Topics Smoking and Your Heart article and the NHLBI's "Your Guide to a Healthy Heart."
Learn how to manage stress, relax, and cope with problems. This can improve your emotional and physical health. Physical activity, medicine, and relaxation therapy can help relieve stress. You also may want to consider taking part in a stress management program.
Learn more about heart disease and the traits, conditions, and habits that can raise your risk for it. Talk with your doctor about your risk factors for heart disease and how to control them.
If lifestyle changes aren't enough, your doctor may prescribe medicines to control your risk factors. Take all of your medicines as your doctor advises.
Know your numbers—ask your doctor for these three tests, and have the results explained to you:
Know your body mass index (BMI) and waist measurement. BMI measures your weight in relation to your height and gives an estimate of your total body fat. You can use the NHLBI's online BMI calculator to figure out your BMI, or your doctor can help you.
In adults, a BMI of 18.5 to 24.9 is considered normal. A BMI of 25 to 29.9 is considered overweight. A BMI of 30 or more is considered obese.
To measure your waistline, stand and place a tape measure around your middle, just above your hipbones. Measure your waist just after you breathe out. A waist measurement of 35 inches or more for women and 40 inches or more for men is a risk factor for heart disease and other health problems.
Know your family history of heart disease. If you or someone in your family has heart disease, tell your doctor.
If you have coronary microvascular disease (MVD), you can take action to control it. Follow the steps described in "How Can Coronary Microvascular Disease Be Prevented?"
Coronary MVD, like traditional coronary heart disease, increases your risk for a heart attack. If you have signs or symptoms of a heart attack, call 9–1–1 at once.
These signs and symptoms may include chest pain, upper body discomfort, shortness of breath, and nausea (feeling sick to your stomach). For more detailed information about the warning signs of a heart attack, go to the section on warning signs below.
If you have coronary MVD, see your doctor regularly to make sure the disease isn't getting worse. Work with your doctor to keep track of your cholesterol, blood pressure, and blood sugar levels. This will help your doctor adjust your treatment as needed.
You may need to see a cardiologist (heart specialist) in addition to your primary care doctor. Talk with your doctor about how often you should schedule office visits or blood tests. Between those visits, call your doctor if you have any new symptoms or your symptoms worsen.
You should:
If you have coronary MVD, learn the warning signs of a heart attack. The signs and symptoms of a heart attack include:
If you think you're having a heart attack, call 9–1–1 at once. Early treatment can prevent or limit damage to your heart muscle. Do not drive to the hospital or let someone else drive you. Instead, call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room.
Let the people you see regularly know you're at risk for a heart attack. They can seek emergency care if you suddenly faint, collapse, or have other severe symptoms.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has helped doctors learn more about heart disease, its risk factors, and ways to prevent and treat the disease.
The NHLBI continues to support research aimed at learning more about heart disease, including coronary microvascular disease (MVD). For example, NHLBI-supported research includes studies that:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
Source: NHLBI, NIH
A stroke is serious, just like a heart attack. Each year in the United States, approximately 795,000 people have a stroke. About 610,000 of these are first or new strokes. On average, one American dies from stroke every four minutes. Stroke is the fourth leading cause of death in the United States, and causes more serious long-term disabilities than any other disease.
Nearly three-quarters of all strokes occur in people over the age of 65. And the risk of having a stroke more than doubles each decade between the ages of 55 and 85.
Stroke occurs in all age groups, in both sexes, and in all races in every country. It can even occur before birth, when the fetus is still in the womb.
Learning about stroke can help you act in time to save a relative, neighbor, or friend. And making changes in your lifestyle can help you prevent stroke.
A stroke is sometimes called a "brain attack." Most often, stroke occurs when blood flow to the brain stops because it is blocked by a clot. When this happens, the brain cells in the immediate area begin to die.
Some brain cells die because they stop getting the oxygen and nutrients they need to function. Other brain cells die because they are damaged by sudden bleeding into or around the brain. The brain cells that don't die immediately remain at risk for death. These cells can linger in a compromised or weakened state for several hours. With timely treatment, these cells can be saved.
New treatments are available that greatly reduce the damage caused by a stroke. But you need to arrive at the hospital as soon as possible after symptoms start to prevent disability and to greatly improve your chances for recovery. Knowing stroke symptoms, calling 911 immediately, and getting to a hospital as quickly as possible are critical.
There are two kinds of stroke. The most common kind of stroke is called ischemic stroke. It accounts for approximately 80 percent of all strokes. An ischemic stroke is caused by a blood clot that blocks or plugs a blood vessel supplying blood to the brain. Blockages that cause ischemic strokes stem from three conditions:
The other kind of stroke is called hemorrhagic stroke. A hemorrhagic stroke is caused by a blood vessel that breaks and bleeds into the brain.
One common cause of a hemorrhagic stroke is a bleeding aneurysm. An aneurysm is a weak or thin spot on an artery wall. Over time, these weak spots stretch or balloon out due to high blood pressure. The thin walls of these ballooning aneurysms can rupture and spill blood into the space surrounding brain cells.
Artery walls can also break open because they become encrusted, or covered with fatty deposits called plaque, eventually lose their elasticity and become brittle, thin, and prone to cracking. Hypertension, or high blood pressure, increases the risk that a brittle artery wall will give way and release blood into the surrounding brain tissue.
The brain is the most complex organ in the human body. It is the seat of intelligence, interpreter of the senses, initiator of all movement, and the controller of behavior. How a stroke affects us depends on which part of the brain is damaged.
Stroke damage in the brain can affect the entire body -- resulting in mild to severe disabilities. These include paralysis, problems with thinking, trouble speaking, and emotional problems.
A common disability that results from stroke is complete paralysis on one side of the body, called hemiplegia. A related disability that is not as debilitating as paralysis is one-sided weakness, or hemiparesis. The paralysis or weakness may affect only the face, an arm, or a leg, or it may affect one entire side of the body and face.
A stroke patient may have problems with the simplest of daily activities, such as walking, dressing, eating, and using the bathroom. Movement problems can result from damage to the part of the brain that controls balance and coordination. Some stroke patients also have trouble swallowing, called dysphagia.
Stroke may cause problems with thinking, awareness, attention, learning, judgment, and memory.
In some cases of stroke, the patient suffers a "neglect" syndrome. The neglect syndrome means that the stroke patient has no knowledge of one side of his or her body, or one side of the visual field, and is unaware of the problem. A stroke patient may be unaware of his or her surroundings, or may be unaware of the mental problems that resulted from the stroke.
Stroke victims often have a problem forming or understanding speech. This problem is called aphasia. Aphasia usually occurs along with similar problems in reading and writing. In most people, language problems result from damage to the left hemisphere of the brain.
Slurred speech due to weakness or incoordination of the muscles involved in speaking is called dysarthria, and is not a problem with language. Because it can result from any weakness or incoordination of the speech muscles, dysarthria can arise from damage to either side of the brain.
A stroke can also lead to emotional problems. Stroke patients may have difficulty controlling their emotions or may express inappropriate emotions in certain situations. One common disability that occurs with many stroke patients is depression.
Post-stroke depression may be more than a general sadness resulting from the stroke incident. It is a serious behavioral problem that can hamper recovery and rehabilitation and may even lead to suicide. Post-stroke depression is treated as any depression is treated, with antidepressant medications and therapy.
Stroke patients may experience pain, uncomfortable numbness, or strange sensations after a stroke. These sensations may be due to many factors, including damage to the sensory regions of the brain, stiff joints, or a disabled limb.
An uncommon type of pain resulting from stroke is called central stroke pain or central pain syndrome or CPS. CPS results from damage to an area called the thalamus. The pain is a mixture of sensations, including heat and cold, burning, tingling, numbness, and sharp stabbing and underlying aching pain.
The pain is often worse in the hands and feet and is made worse by movement and temperature changes, especially cold temperatures. Unfortunately, since most pain medications provide little relief from these sensations, very few treatments or therapies exist to combat CPS.
The brain stem controls vital bodily functions such as breathing, blood pressure and heartbeat. A stroke in the brain stem can be fatal or can leave someone in a “locked-in” state in which the person cannot control anything below the neck. As with other types of stroke, early treatment is crucial.
Knowing the warning signs of stroke and controlling stroke's risk factors can lower your risk of death or disability. If you suffer a stroke, you may not realize it at first. The people around you might not know it, either. Your family, friends, or neighbors may think you are unaware or confused. You may not be able to call 911 on your own. That's why everyone should know the signs of stroke and know how to act fast.
Warning signs are clues your body sends to tell you that your brain is not receiving enough oxygen. If you observe one or more of the following signs of a stroke or "brain attack," don't wait. Call 911 right away!
These are warning signs of a stroke:
Other danger signs that may occur include double vision, drowsiness, and nausea or vomiting.
Sometimes the warning signs of stroke may last only a few moments and then disappear. These brief episodes, known as transient ischemic attacks or TIAs, are sometimes called "mini-strokes."
Although brief, TIAs identify an underlying serious condition that isn't going away without medical help. Unfortunately, since they clear up, many people ignore them. Don't ignore them. Heeding them can save your life.
Stroke is a medical emergency. Every minute counts when someone is having a stroke. The longer blood flow is cut off to the brain, the greater the damage. Immediate treatment can save people’s lives and enhance their chances for successful recovery.
Ischemic strokes, the most common type of strokes, can be treated with a drug called t-PA that dissolves blood clots obstructing blood flow to the brain. The window of opportunity to start treating stroke patients is three hours, but to be evaluated and receive treatment, patients need to get to the hospital within 60 minutes.
Don't wait for the symptoms of stroke to improve or worsen. If you believe you are having a stroke, call 911 immediately. Making the decision to call for medical help can make the difference in avoiding a lifelong disability and in greatly improving your chances for recovery.
If you observe someone having a stroke – if he or she suddenly loses the ability to speak, or move an arm or leg on one side, or experiences facial paralysis on one side – call 911 immediately.
A risk factor is a condition or behavior that increases your chances of getting a disease. Having a risk factor for stroke doesn't mean you'll have a stroke. On the other hand, not having a risk factor doesn't mean you'll avoid a stroke. But your risk of stroke grows as the number and severity of risk factors increase.
These risk factors for stroke cannot be changed by medical treatment or lifestyle changes.
Some of the most important risk factors for stroke that CAN be treated are
High blood pressure, also called hypertension, is by far the most potent risk factor for stroke. If your blood pressure is high, you and your doctor need to work out an individual strategy to bring it down to the normal range. Here are some ways to reduce blood pressure:
Your doctor may prescribe medicines that help lower blood pressure. Controlling blood pressure will also help you avoid heart disease, diabetes, and kidney failure.
Cigarette smoking has been linked to the buildup of fatty substances in the carotid artery, the main neck artery supplying blood to the brain. Blockage of this artery is the leading cause of stroke in Americans. Also, nicotine raises blood pressure, carbon monoxide reduces the amount of oxygen your blood can carry to the brain, and cigarette smoke makes your blood thicker and more likely to clot.
Your doctor can recommend programs and medications that may help you quit smoking. By quitting -- at any age -- you also reduce your risk of lung disease, heart disease, and a number of cancers including lung cancer.
Heart disease, including common heart disorders such as coronary artery disease, valve defects, irregular heart beat, and enlargement of one of the heart's chambers, can result in blood clots that may break loose and block vessels in or leading to the brain. The most common blood vessel disease, caused by the buildup of fatty deposits in the arteries, is called atherosclerosis, also known as hardening of the arteries.
Your doctor will treat your heart disease and may also prescribe medication, such as aspirin, to help prevent the formation of clots. Your doctor may recommend surgery to clean out a clogged neck artery if you match a particular risk profile.
A high level of total cholesterol in the blood is a major risk factor for heart disease, which raises your risk of stroke. Your doctor may recommend changes in your diet or medicines to lower your cholesterol.
Experiencing warning signs and having a history of stroke are also risk factors for stroke. Transient ischemic attacks, or TIAs, are brief episodes of stroke warning signs that may last only a few moments and then go away. If you experience a TIA, get help at once. Call 911.
If you have had a stroke in the past, it's important to reduce your risk of a second stroke. Your brain helps you recover from a stroke by drawing on body systems that now do double duty. That means a second stroke can be twice as bad.
Having diabetes is another risk factor for stroke. You may think this disorder affects only the body's ability to use sugar, or glucose. But it also causes destructive changes in the blood vessels throughout the body, including the brain.
Also, if blood glucose levels are high at the time of a stroke, then brain damage is usually more severe and extensive than when blood glucose is well-controlled. Treating diabetes can delay the onset of complications that increase the risk of stroke.
Stroke is preventable and treatable. A better understanding of the causes of stroke has helped people make lifestyle changes that have cut the stroke death rate nearly in half in the last two decades.
While family history of stroke plays a role in your risk, there are many risk factors you can control:
Physicians have several diagnostic techniques and imaging tools to help diagnose stroke quickly and accurately. The first step in diagnosis is a short neurological examination, or an evaluation of the nervous system.
When a possible stroke patient arrives at a hospital, a health care professional, usually a doctor or nurse, will ask the patient or a companion what happened and when the symptoms began. Blood tests, an electrocardiogram, and a brain scan such as computed tomography or CT, or magnetic resonance imaging or MRI, will often be done.
One test that helps doctors judge the severity of a stroke is the standardized NIH Stroke Scale, developed by the National Institute of Neurological Disorders and Stroke at the National Institutes of Health, or NIH. Health care professionals use the NIH Stroke Scale to measure a patient's neurological deficits by asking the patient to answer questions and to perform several physical and mental tests.
Other scales include the Glasgow Coma Scale, the Hunt and Hess Scale, the Modified Rankin Scale, and the Barthel Index.
Health care professionals also use a variety of imaging techniques to evaluate acute stroke patients. The most widely used is computed tomography or CT scan, sometimes pronounced “CAT” scan, which is comprised of a series of cross-sectional images of the head and brain.
CT scans are sensitive for detecting hemorrhage and are therefore useful for differentiating hemorrhagic stroke, caused by bleeding in the brain, from ischemic stroke, caused by a blockage of blood flow to the brain.
Hemorrhage is the primary reason for avoiding thrombolytic therapy (drugs that break up or dissolve blood clots), the only proven therapy for acute ischemic stroke.
Because thrombolytic therapy might make a hemorrhagic stroke worse, doctors must confirm that the acute symptoms are not due to hemorrhage prior to giving the drug.
A CT scan may show evidence of early ischemia – an area of tissue that is dead or dying due to a loss of blood supply. Ischemic strokes generally show up on a CT scan about six to eight hours after the start of stroke symptoms. Though not as common in practice, CT scans also can be performed with a contrast agent to help visualize a blockage in the large arteries supplying the brain, or detect areas of decreased blood flow to the brain.
Because CT is readily available at all hours at most major hospitals, produces images quickly, and is good for ruling out hemorrhage prior to starting thrombolytic therapy, CT is the most widely used diagnostic imaging technique for acute stroke.
Another imaging technique used in acute stroke patients is the magnetic resonance imaging or MRI scan. MRI uses magnetic fields to detect a variety of changes in the brain and blood vessels caused by a stroke. One effect of ischemic stroke is the slowing of water movement through the injured brain tissue. Because MRI can show this type of injury very soon after stroke symptoms start, MRI has proven useful for diagnosing acute ischemic stroke before it is visible on CT. MRI also allows doctors to visualize blockages in the arteries, identify sites of prior stroke, and create a stroke treatment and prevention plan.
MRI and CT are equally accurate for determining when hemorrhage is present. The benefit of MRI over a CT scan is more accurate and earlier diagnosis of ischemic stroke, especially for smaller strokes and transient ischemic attacks (TIAs). MRI can be more sensitive than CT for detecting other types of neurological disorders that mimic the symptoms of stroke. However, MRI cannot be performed in patients with certain types of metallic or electronic implants, such as pacemakers for the heart.
Although increasingly used in the emergency diagnosis of stroke, MRI is not immediately available at all hours in most hospitals, where CT is used for acute stroke diagnosis. MRI typically takes longer to perform than CT, and therefore may not be the first choice when minutes count.
With stroke, treatment depends on the stage of the disease. There are three treatment stages for stroke: prevention, therapy immediately after stroke, and rehabilitation after stroke. Stroke therapies include medications, surgery, and rehabilitation.
Medication or drug therapy is the most common treatment for stroke. The most popular kinds of drugs to prevent or treat stroke are antithrombotics -- which include antiplatelet agents and anticoagulants -- and thrombolytics.
In treating a stroke that has just occurred, every minute counts. Ischemic strokes -- the most common kind -- can be treated with thrombolytic drugs. These drugs halt the stroke by dissolving the blood clot that is blocking blood flow to the brain. But a person needs to be at the hospital as soon as possible after stroke symptoms start to be evaluated and receive treatment.
A thrombolytic drug known as t-PA can be effective if a person receives it intravenously (in a vein) within 3 hours after his or her stroke symptoms have started. Because there is such a narrow time window for giving t-PA, it is important to note the time any stroke symptoms appear. Since thrombolytic drugs can increase bleeding, t-PA should be used only after the doctor is certain that the patient has suffered an ischemic and not a hemorrhagic stroke.
Antithrombotics prevent the formation of blood clots that can become stuck in an artery of the brain and cause strokes. Antiplatelet drugs prevent clotting by decreasing the activity of platelets, which are blood cells that help blood clot. By reducing the risk of blood clots, these drugs lower the risk of ischemic stroke.
In the case of stroke, doctors prescribe antiplatelet drugs mainly for prevention. The most widely known and used antiplatelet drug is aspirin. Other antiplatelet drugs include clopidogrel, ticlopidine, and dipyridamole.
Anticoagulants reduce the risk of stroke by reducing the clotting property of the blood. The most commonly used oral anticoagulants include warfarin, also known as Coumadin®, dabigatran (Pradaxa) and rivaroxaban (Xarelto). Injectable anticoagulants include heparin, enoxaparin (Lovenox), and dalteparin (Fragmin).
Neuroprotectants are medications or other treatments that protect the brain from secondary injury caused by stroke. Although the FDA (Food and Drug Administration) has not approved any neuroprotectants for use in stroke at this time, many have been tested or are being tested in clinical trials. Cooling of the brain (hypothermia) is beneficial for improving neurological function after a cardiac arrest.

Surgery and vascular procedures can be used to prevent stroke, to treat stroke, or to repair damage to the blood vessels or malformations in and around the brain.

Carotid endarterectomy is a surgical procedure in which a surgeon removes fatty deposits, or plaque, from the inside of one of the carotid arteries. The procedure is performed to prevent stroke. The carotid arteries are located in the neck and are the main suppliers of blood to the brain.
In addition to surgery, a variety of techniques have been developed to allow certain vascular problems to be treated from inside the artery using specialized catheters with the goal of improving blood flow. Vascular is a word that refers to blood vessels, arteries, and veins that carry blood throughout the body.
A catheter is a very thin, flexible tube that can be inserted into one of the major arteries of the leg or arm and then directed through the blood vessels to the diseased artery. Physicians trained in this technique called angiography undergo additional training to treat problems in the arteries of the brain or spinal cord. These physicians are called neurointerventionalists.
The NINDS study, Carotid Revascularization Endarterectomy vs. Stenting Trial, (CREST), compared carotid artery stenting with endarterectomy and found that these two surgical procedures are equally effective in preventing future strokes. Your physician can talk to you about the best option for you. For more information about treating arterial stenosis and preventing stroke, visit http://www.ninds.nih.gov/disorders/stroke/arterial_stenosis_backgrounder.htm.
One useful surgical procedure for treatment of brain aneurysms to prevent hemorrhage, or bleeding around the brain, is a technique called "clipping." An aneurysm is a weak or thin spot that develops on the wall of an artery or vein. Clipping involves an operation to apply a metal clip that closes off the aneurysm from the blood vessel, which greatly reduces the chance that it will bleed.
The detachable coil technique is used by angiographers to treat intracranial aneurysms, or aneurysms that occur inside the skull. Angiographers use a catheter to insert a small platinum coil into the aneurysm, where it triggers clotting of the aneurysm. Stents are sometimes used to keep the normal artery open while the aneurysm clots off.
Arteriovenous malformations are a tangle of blood vessels inside the brain which may carry risk of bleeding. Surgery to remove the blood vessels may be possible in some patients. Angiographers can also sometimes insert a glue-like material to close off the feeding arteries to the tangled vessels. Radiation therapy can be used in small arteriovenous malformations to cause scarring and closing of the malformation over time.
Stroke is the number one cause of serious adult disability in the United States. Stroke disability is devastating to the stroke patient and family, but therapies are available to help rehabilitate patients after stroke.
For most stroke patients, rehabilitation mainly involves physical therapy. The aim of physical therapy is to have the stroke patient relearn simple motor activities such as walking, sitting, standing, lying down, and the process of switching from one type of movement to another.
To achieve this, stroke patients work with physical therapists who use training, exercises, and physical manipulation of the stroke patient's body to restore movement, balance, and coordination.
Another type of therapy to help patients relearn daily activities is occupational therapy. This type of therapy also involves exercise and training. Its goal is to help the stroke patient relearn everyday activities such as eating, drinking and swallowing, dressing, bathing, cooking, reading and writing, and toileting. Occupational therapists seek to help the patient become independent or semi-independent.
Speech and language problems arise when brain damage occurs in the language centers of the brain. Due to the brain's great ability to learn and change, which is called brain plasticity, other areas can adapt to take over some of the lost functions.
Speech therapy helps stroke patients relearn language and speaking skills, or learn other forms of communication. Speech therapy is appropriate for patients who have no problems with cognition or thinking, but have problems understanding speech or written words, or problems forming speech.
Besides helping with language skills, speech therapy also helps stroke patients develop coping skills to deal with the frustration of not being able to communicate fully. With time and patience, a stroke survivor should be able to regain some, and sometimes all, language and speaking abilities.
Many stroke patients require psychological or psychiatric help after a stroke. Psychological problems such as depression, anxiety, frustration, and anger are common disabilities in people who have suffered a stroke.
Talk therapy, along with the right medication, can help ease some of the mental and emotional problems that result from stroke. Sometimes it is helpful for family members of the stroke patient to seek psychological help for themselves as well.
The National Institute of Neurological Disorders and Stroke sponsors a wide range of basic and clinical research aimed at finding better ways to prevent, diagnose, and treat stroke, and to restore functions lost as a result of stroke.
Currently, scientists are studying the risk factors for stroke and the process of brain damage that results from stroke. Some brain damage may be secondary, occurring after the initial death of brain cells caused by the lack of blood flow to the brain tissue.
This secondary brain damage results from a toxic reaction to the primary damage. Researchers are studying this toxic reaction and ways to prevent secondary injury to the brain. Scientists hope to develop neuroprotective agents, or drugs that protect the brain, to prevent this damage.
Scientists are also conducting stroke studies in animals. By studying stroke in animals, researchers hope to get a better picture of what might be happening in human stroke patients. Scientists can also use animal models to test promising therapies for stroke. If a therapy proves helpful for animals, scientists can consider testing the therapy in humans.
One promising area of animal research involves hibernation. The dramatic decrease of blood flow to the brain in hibernating animals is so extensive that it would kill a non-hibernating animal. If scientists can discover how animals hibernate without experiencing brain damage, they may discover ways to stop the brain damage associated with decreased blood flow in stroke patients.
Another study used a vaccine that interferes with inflammation inside blood vessels to reduce the frequency and severity of strokes in animals with high blood pressure and a genetic predisposition to stroke. Researchers hope that the vaccine will work in humans and could be used to prevent many of the strokes that occur each year in people with high risk factors.
Scientists also are working to develop new and better ways to help the brain repair itself to restore important functions to stroke patients. New advances in imaging and rehabilitation have shown that the brain can compensate for functions lost as a result of stroke.
When cells in an area of the brain responsible for a particular function die after a stroke, the patient becomes unable to perform that function. However, the brain's ability to learn and change, called plasticity, and its ability to rewire the connections between its nerve cells means that it can compensate for lost functions. One part of the brain can actually change functions and take up the more important functions of a disabled part.
Clinical trials are scientific studies using volunteers that give researchers a way to test medical advances in humans. Clinical trials test surgical devices and procedures, medications, and rehabilitation therapies. They also test methods to improve lifestyles and mental and social skills.
Clinical trials may compare a new medical approach to a standard one that is already available or to a placebo that contains no active ingredients or to no intervention. Some clinical trials compare interventions that are already available to each other. When a new product or approach is being studied, it is not usually known whether it will be helpful, harmful, or no different than available alternatives (including no intervention). The investigators try to determine the safety and usefulness of the intervention by measuring certain outcomes in the participants.
Scientists are using clinical trials to
Participating in a clinical study contributes to medical knowledge. The results of these studies can make a difference in the care of future patients by providing information about the benefits and risks of therapeutic, preventative, or diagnostic products or interventions.
You can find more information about current stroke clinical trials at the NIH Clinical Trials Registry at www.clinicaltrials.gov. You can search for a trial using criteria such as condition or disease, medication or therapy. Each entry includes a trial description, sponsors, purpose, estimated completion date, eligibility criteria, and contact information.
You can also call the NIH research study information line at 1-800-411-1222, TTY-1-866-411-1010, or e-mail prpl@mail.cc.nih.gov
For more information on stroke, including research sponsored by the National Institute of Neurological Disorders and Stroke, call 1-800-352-9424 or visit the Web site at www.ninds.nih.gov.
Source: NIHSenior, NIH
![]()
Related information
The most common form of heart disease is coronary artery disease (CAD). In CAD, plaque builds up on the walls of the arteries that carry blood to the heart. Over time, this buildup causes the arteries to narrow and harden. This keeps the heart from getting all the blood it needs. Blood clots may develop. If the clot mostly or completely blocks blood flow to the heart, it causes a heart attack. Stroke happens when the brain doesn’t get enough blood. Without enough blood, brain cells start to die.
Heart attack, stroke, and other forms of heart disease are a threat to so many women. But you can take steps to protect your heart and lower your risk. Steps include getting regular physical activity, making healthy food choices, knowing your numbers and taking good care of yourself overall. It is also important to make sure you talk to your doctor about heart health and the use of menopausal hormone therapy or aspirin.
You don't have to become a super athlete, but your body needs to move. The 2008 Physical Activity Guidelines for Americans state that an active lifestyle can lower your risk of early death from heart disease, stroke, and many other health problems. It can also boost your mood. Health benefits are gained by doing the following each week:
So pick an activity you like, and do it often.
Eating fatty, greasy food can make you put on weight. But that's not the only risk. Unhealthy eating has a direct impact on your arteries, your blood pressure, your glucose level, among other things. You don't need to go on a special diet to eat healthy. Just make sure you focus on eating fruits and vegetables, whole grains, fat-free or low-fat dairy products, fish, beans, peas, nuts, and lean meats. The foods you eat should also be low in saturated fat, trans fat, cholesterol (koh-LESS-tur-ol), salt, and added sugars. If you drink alcohol, do it moderately. Women should drink no more than one alcoholic drink per day.
Ask your doctor to check your blood pressure, cholesterol (total, HDL, LDL, and triglycerides) and blood sugar levels. These simple screening tests will give you important information about your heart health. Your doctor can tell you what your numbers mean and what you need to do to protect your heart. Check out the Screening tests and vaccines section on this site to learn how often you need these screening tests.
Stress, anxiety, depression, and lack of sleep have all been linked to increased risk of heart disease. And they're not doing your mind or the rest of your body any good either. You may feel that you don't have enough time to take a break or get enough sleep now. But the possible results of overloading yourself, including heart attack and stroke, aren't worth it. In the midst of all you do, it's important to make time for yourself. Make sure you get the amount of sleep you need each day to wake up feeling refreshed. Take steps to keep stress in check, such as taking time each day to relax and unwind with friends or loved ones. And if you're having trouble coping because of depression, anxiety, or other emotional health issues, get help. Your doctor or a counselor can teach you healthy ways to reduce stress or suggest treatment for depression or other mental health problems. Although we don't know if treating emotional problems or reducing stress lowers heart disease risk, doing so will boost your overall health and well-being.
Once you reach menopause, your ovaries stop making estrogen, which protects against plaque buildup, and your heart disease risk goes up. You might wonder if menopausal hormone therapy (MHT) can help lower the risk. But recent studies confirmed that women should not use MHT to protect against heart disease. Rather, MHT is good at relieving moderate to severe symptoms of menopause and preventing bone loss. For now, the safest option for MHT is to use the lowest dose that helps for the shortest time you need it. Learn more about study findings and the benefits and risks of MHT in our menopause section.
The U.S. Preventive Services Task Force recommends that women ages 55 to 79 take aspirin to lower their risk of ischemic stroke. This is advised when the benefit outweighs the possible harm of gastrointestinal bleeding. The benefit depends on your personal risk of both stroke and gastrointestinal bleeding. You should discuss your risk with your doctor and decide together if taking aspirin is right for you.
![]()

Are you at risk for having a heart attack?
Factors such as your age, cholesterol levels, and blood pressure affect your heart health. Use this Web tool to determine your 10-year risk of having a heart attack.
Heart disease is the leading cause of death in the United States. Reading those words may make you feel like you have no control. But many things can affect whether or not you develop heart disease, some of which you can control. That's why it is important to understand your personal risk factors.
Risk factors are conditions, habits, family history, and other facts about yourself that make you more likely to develop certain diseases. The more risk factors you have, the higher your risk of getting certain diseases. Some risk factors such as age or family history can't be controlled. But many can be controlled by making changes in the way you live. In this section you can learn more about the different kinds of risk factors that you can and can't control.
![]()
Heart disease risk factors you can control

Did you know?
In women, high triglycerides combined with low HDL cholesterol can mean a very high risk of heart disease.
You can control the following risk factors by making lifestyle changes. Your doctor might also suggest medicine to help control some risk factors, such as high blood pressure or high cholesterol.
These are types of fat found in your blood and other parts of your body. The body needs small amounts of them to work, but too much can cause a problem. The extra amounts can cling to, and clog, your arteries. A blood test can measure your levels of:
Blood pressure is the force your blood makes against your artery walls. If this pressure is too high, over time it can damage your artery walls. There are two kinds of pressure. Systolic (siss-TOL-ihk) is the pressure as your heart pumps blood into your arteries. Diastolic (deye-uh-STOL-ihk) is the pressure between beats, when your heart relaxes. To lower your risk of heart disease, your blood pressure should be less than 120 systolic/80 diastolic.
Smoking hurts your heart. The more you smoke, the higher your risk. About half of all heart attacks in women are due to smoking! And, if you smoke and also take birth control pills, you are at even higher risk.
Diabetes is a disease in which blood glucose (sugar) levels are too high. Type 2 diabetes is the most common type. It usually begins after the age of 40, often in people who are overweight or obese. Uncontrolled diabetes can damage artery walls. This risk is even higher in women than men.
The more overweight you are, the higher your risk of heart disease. This is true even if you have no other risk factors. Being overweight also raises your chances of developing diabetes, high blood pressure, and high cholesterol. To lower your risk, your body mass index (BMI) should be between 18.5 and 24.9. A BMI of 30 or higher is considered obese. Use this calculator to find your BMI.
Related information
Like being overweight, lack of physical activity raises your heart disease risk even if you have no other risk factors. Being inactive also increases your chances of developing high blood pressure and diabetes. It also raises your risk of being overweight or obese.
You can improve your health by doing the following each week:
and
So pick an activity you like, and do it often.
Depending on how much you drink, alcohol can greatly raise your risk of heart disease, or help lower it. Heavy drinking can cause many heart-related problems. More than three drinks a day can raise blood pressure and triglyceride levels. Too much alcohol can also damage your heart muscle. However, moderate drinkers are less likely to develop heart disease than people who drink heavily or don't drink at all. For women, moderate means no more than one drink a day. Drinking more than one drink a day increases your risk of certain cancers. And if you're pregnant or planning to become pregnant, you should not drink. Your doctor can help you decide if the heart benefits of moderate drinking outweigh the risks.
Has anyone ever told you that you snore? Loud snoring can be a sign of sleep apnea (AP-nee-uh). Sleep apnea is a sleep disorder that can raise your chances of having a heart attack. With obstructive sleep apnea — the most common type — the tissue in the back of the throat relaxes. This blocks airflow to your lungs. This lowers the oxygen level in your blood, which makes your heart work harder. Sleep apnea often leads to high blood pressure. If you think you might have sleep apnea, talk to your doctor.
Having metabolic (met-uh-BOL-ihk) syndrome doubles your risk of getting heart disease or having a stroke. You have it if you have any three of these five risk factors:
Taking steps to eliminate these risk factors will improve your heart and overall health.
![]()

You can't control these risk factors. But knowing what they are can help you understand your overall risk for heart disease.
Women usually develop heart disease about 10 to 15 years later than men. This is because until menopause, the ovaries produce estrogen. Estrogen protects women against plaque buildup. But at menopause the ovaries stop making estrogen, and your risk goes up. By age 70, women have about the same risk for heart disease as same-aged men. Menopause isn't the only reason getting older is a risk factor. As people age, arteries get stiffer and thicker. Also, systolic blood pressure (the top number) often goes up. These changes contribute to plaque buildup in artery walls.
Women with a father or brother who developed heart disease before age 55 are at higher risk. Women with a mother or sister who developed heart disease before age 65 are also at higher risk. However, young women with a family history may not be aware of this risk. So, they may be less careful about living a heart-healthy lifestyle than men with a family history.
As a group, African Americans are more likely to develop high blood pressure. Research also suggests that racial and ethnic minorities are generally more likely to develop heart disease. The reasons for this greater risk are unclear.
![]()

Emotional and environmental factors can also contribute to your heart disease risk.
Negative emotions like depression, stress, and anxiety can raise your risk of developing heart disease. Researchers aren't exactly sure why this is. Perhaps these emotions lead to unhealthy ways of coping, such as smoking, drink too much, or eating high-fat foods — all which can put your heart health at risk. Research also suggests that depression itself is a risk factor for heart disease. Depression, stress, and other negative emotions may affect the body in ways that trigger plaque buildup or clot formation within the arteries. So, taking care of your emotional health is also an important part of taking care of your heart health. Talk to your doctor or a counselor if you have symptoms of depression or problems coping with daily stressors.
Not getting enough sleep won't just make you cranky, it can also raise your risk of heart disease. Most adults need seven to nine hours of sleep every night. In adults between the ages of 32 and 59, sleeping less than five hours each day can double the risk of high blood pressure. So make sure you're getting enough sleep to wake up feeling refreshed. If you're having trouble sleeping, don't drink caffeine or alcohol before bed and make sure your bedroom is cool and dark. Also, try doing something relaxing before bed and use your bed for sleep and sex only.
Research shows that lower income adults have an increased risk of heart disease. Children born into lower income families are also more likely to have heart disease as adults. This may be because low-income adults are less likely to be physically active, eat a heart-healthy diet, and are more likely to smoke. It can be difficult to eat a heart-healthy diet in lower income neighborhoods. It may also be hard to find a safe place to be physically active. Check with religious or community centers, or the parks department to see if there are any physical activity groups you can join.![]()
Related information
Many people think a heart attack is sudden, like a "movie" heart attack, where someone clutches her chest and falls over. But the truth is that many heart attacks start slowly as mild pain or discomfort. These feelings may even come and go. A heart attack is very serious and you should get to the hospital right away by calling 9-1-1. Learn what to expect at the hospital when you're having a heart attack.
For both women and men, the most common sign of a heart attack is pain or discomfort in the center of the chest. The pain or discomfort can be mild or strong. It can last more than a few minutes, or it can go away and come back. See the figure, "Signs of a Heart Attack," for a full list of heart attack signs.

Women are more likely than men to have the "other" common signs of a heart attack. These include shortness of breath, nausea or vomiting, and pain in the back, neck, or jaw. Sometimes the signs of a heart attack happen suddenly. But they can also develop slowly, over hours, days, and even weeks before a heart attack occurs.
The more heart attack signs that you have, the more likely it is that you are having a heart attack. Also, if you've already had a heart attack, your symptoms may not be the same for another one. Even if you're not sure you're having a heart attack, you should still have it checked out.
If you think you, or someone else, may be having a heart attack, wait no more than a few minutes — five at most — before calling 911. Do not drive yourself or let a friend drive you. You may need medical help on the way to the hospital. Paramedics are trained to treat you on the way to the emergency room.
Getting there quickly is very important. Treatments for opening clogged arteries work best within the first hour after a heart attack starts. Women are more likely than men to die of a heart attack. One reason is that women often have the less-common signs. This can lead to misdiagnosis. If you think you're having a heart attack, get emergency help right away. Don't let anyone tell you that you are overreacting or to wait and see. Ask for tests that can show if you're having a heart attack. It's better to be safe than sorry.
Cardiac arrest
A heart attack is not the same as cardiac arrest. In a heart attack, the heart does not usually stop beating. During cardiac arrest, the heart totally stops beating.
With cardiac arrest, the only way to restart the heart is with a defibrillator (dee-FIB-ruh-lay-tur), a machine that sends an electrical shock to the heart to restore normal rhythm. This treatment must be given as soon as possible. Call 911 and begin CPR immediately. The American Heart Association says that with "hands only" CPR, anyone can give lifesaving treatment to someone having cardiac arrest. Push hard and fast in the center of the chest and keep going until emergency personnel arrive. Do not give CPR for heart attack.
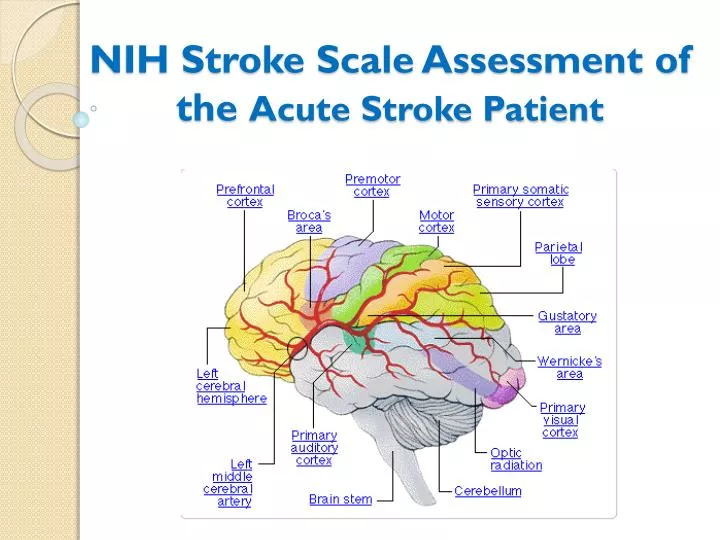
![]()

A stroke happens when part of your brain doesn't get the blood that it needs. It is sometimes called a "brain attack." This is because, like a heart attack, a stroke causes a lack of blood flow. Without blood, your brains cells will start to die within minutes. A stroke is very serious and you should get to the hospital right away by calling 9-1-1. Learn what to expect at the hospital when you're having a stroke.
Strokes happen fast. Some of the most common signs are sudden numbness or weakness on one side of the body, confusion, and trouble walking or speaking. See the figure, "Signs of a Stroke," for a full list of stroke signs.

If you have stroke signs that don't last long, you might have had a "mini-stroke." These small strokes — called a transient ischemic attack (TIA) — may not last long, but they still require treatment. Also, a TIA could be a sign that you are about to have a major stroke. "Mini" or not, these symptoms are an emergency.
If you have or see someone having any stroke symptoms, call 911 right away. Every minute counts! Current stroke treatments can raise the chances of recovering with few or no disabilities. But you must get help right away. These treatments will work only if you get them no later than three hours after your symptoms began. Do not drive yourself or let a friend drive you. You may need medical help on the way to the hospital. Paramedics are trained to treat you on the way to the emergency room.
If you're having a stroke, you may not be able to call 911. In fact, you may not even be able to move or talk! In most stroke cases, it's a family member, coworker, or other bystander who calls 911. That's why everyone should know the signs of stroke and how to react.
Choosing a hospital
The hospital you go to can really matter. You have a better chance of having a good outcome if you're taken to a certified stroke center. They have the staff, equipment, and experience need to treat stroke quickly and correctly. Find the nearest certified stroke center, and give the name and address to your family or caregivers. Tell them that if you have a stroke, you want to be taken to that hospital. Even if you live in a rural area, emergency personnel might be able to take you to a certified center by helicopter.
![]()
:max_bytes(150000):strip_icc()/doctors-preparing-patient-for-mri-scan-493216409-5783a9d33df78c1e1f11ab1b.jpg)
You've had a sudden onset of numbness and paralysis or other symptoms of stroke, and you or a companion have called 911. Now what? What happens when you get to the hospital?
Once you get to the hospital, these things will happen quickly:
What happens if the doctor decides I've had a stroke?
The next step will be to use one or more brain imaging tests to see where the stroke is located. The two main methods are computed tomography (tuh-MOG-ruh-fee) (CT) scan and magnetic resonance imaging (MRI).
How will my stroke be treated?
This depends upon the type of stroke you have had and how quickly you receive medical care.
If you have the most common type of stroke (ischemic), you might get a clot-busting drug called t-PA. It is injected into one of your veins. This drug travels in the blood to your brain and breaks up the clot. To work properly and safely, t-PA must be given within three hours from the time your stroke started. In fact the sooner t-PA is given, the better it works.
A new therapy for ischemic strokes is the Mechanical Embolus Removal for Cerebral Ischemia (MERCI) system. A thin wire is guided into the blood vessels and to the blocked artery in the brain. The doctors use the wire to pull the clot out. The MERCI system can be used for up to eight hours after stroke onset.
If you've had the kind of stroke that involves bleeding into the brain, there are fewer treatment options. Usually, little can be done to stop the bleeding. But treatment usually involves trying to reduce pressure with drugs or surgery.
Once your condition is stable, your doctor will talk to you about next steps. This might involve therapy, such as physical therapy or speech therapy, medicines, or surgery.
Source: Office on Women's Health, HHS
What Is Angina?
Angina (an-JI-nuh or AN-juh-nuh) is chest pain or discomfort that occurs if an area of your heart muscle doesn't get enough oxygen-rich blood.
Angina may feel like pressure or squeezing in your chest. The pain also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion.
Angina isn't a disease; it's a symptom of an underlying heart problem. Angina usually is a symptom of coronary heart disease (CHD).
CHD is the most common type of heart disease in adults. It occurs if a waxy substance called plaque (plak) builds up on the inner walls of your coronary arteries. These arteries carry oxygen-rich blood to your heart.


Plaque narrows and stiffens the coronary arteries. This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain. Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow, which can cause a heart attack.
Angina also can be a symptom of coronary microvascular disease (MVD). This is heart disease that affects the heart’s smallest coronary arteries. In coronary MVD, plaque doesn't create blockages in the arteries like it does in CHD.
Studies have shown that coronary MVD is more likely to affect women than men. Coronary MVD also is called cardiac syndrome X and nonobstructive CHD.
The major types of angina are stable, unstable, variant (Prinzmetal's), and microvascular. Knowing how the types differ is important. This is because they have different symptoms and require different treatments.
Stable angina is the most common type of angina. It occurs when the heart is working harder than usual. Stable angina has a regular pattern. (“Pattern” refers to how often the angina occurs, how severe it is, and what factors trigger it.)
If you have stable angina, you can learn its pattern and predict when the pain will occur. The pain usually goes away a few minutes after you rest or take your angina medicine.
Stable angina isn't a heart attack, but it suggests that a heart attack is more likely to happen in the future.
Unstable angina doesn't follow a pattern. It may occur more often and be more severe than stable angina. Unstable angina also can occur with or without physical exertion, and rest or medicine may not relieve the pain.
Unstable angina is very dangerous and requires emergency treatment. This type of angina is a sign that a heart attack may happen soon.
Variant angina is rare. A spasm in a coronary artery causes this type of angina. Variant angina usually occurs while you're at rest, and the pain can be severe. It usually happens between midnight and early morning. Medicine can relieve this type of angina.
Microvascular angina can be more severe and last longer than other types of angina. Medicine may not relieve this type of angina.
Experts believe that nearly 7 million people in the United States suffer from angina. The condition occurs equally among men and women.
Angina can be a sign of CHD, even if initial tests don't point to the disease. However, not all chest pain or discomfort is a sign of CHD.
Other conditions also can cause chest pain, such as:
All chest pain should be checked by a doctor.
Angina usually is a symptom of coronary heart disease (CHD). This means that the underlying causes of angina generally are the same as the underlying causes of CHD.
Research suggests that CHD starts when certain factors damage the inner layers of the coronary arteries. These factors include:
Plaque may begin to build up where the arteries are damaged. When plaque builds up in the arteries, the condition is called atherosclerosis (ath-er-o-skler-O-sis).
Plaque narrows or blocks the arteries, reducing blood flow to the heart muscle. Some plaque is hard and stable and causes the arteries to become narrow and stiff. This can greatly reduce blood flow to the heart and cause angina.
Other plaque is soft and more likely to rupture (break open) and cause blood clots. Blood clots can partially or totally block the coronary arteries and cause angina or a heart attack.
Many factors can trigger angina pain, depending on the type of angina you have.
Physical exertion is the most common trigger of stable angina. Severely narrowed arteries may allow enough blood to reach the heart when the demand for oxygen is low, such as when you're sitting.
However, with physical exertion—like walking up a hill or climbing stairs—the heart works harder and needs more oxygen.
Other triggers of stable angina include:
Blood clots that partially or totally block an artery cause unstable angina.
If plaque in an artery ruptures, blood clots may form. This creates a blockage. A clot may grow large enough to completely block the artery and cause a heart attack. For more information, go to the animation in "What Causes a Heart Attack?"
Blood clots may form, partially dissolve, and later form again. Angina can occur each time a clot blocks an artery.
A spasm in a coronary artery causes variant angina. The spasm causes the walls of the artery to tighten and narrow. Blood flow to the heart slows or stops. Variant angina can occur in people who have CHD and in those who don’t.
The coronary arteries can spasm as a result of:
This type of angina may be a symptom of coronary microvascular disease (MVD). Coronary MVD is heart disease that affects the heart’s smallest coronary arteries.
Reduced blood flow in the small coronary arteries may cause microvascular angina. Plaque in the arteries, artery spasms, or damaged or diseased artery walls can reduce blood flow through the small coronary arteries.
Angina is a symptom of an underlying heart problem. It’s usually a symptom of coronary heart disease (CHD), but it also can be a symptom of coronary microvascular disease (MVD). So, if you’re at risk for CHD or coronary MVD, you’re also at risk for angina.
The major risk factors for CHD and coronary MVD include:
For more detailed information about CHD and coronary MVD risk factors, visit the Diseases and Conditions Index Coronary Heart Disease, Coronary Heart Disease Risk Factors, and Coronary Microvascular Disease articles.
People sometimes think that because men have more heart attacks than women, men also suffer from angina more often. In fact, overall, angina occurs equally among men and women.
Microvascular angina, however, occurs more often in women. About 70 percent of the cases of microvascular angina occur in women around the time of menopause.
Unstable angina occurs more often in older adults. Variant angina is rare; it accounts for only about 2 out of 100 cases of angina. People who have variant angina often are younger than those who have other forms of angina.
Pain and discomfort are the main symptoms of angina. Angina often is described as pressure, squeezing, burning, or tightness in the chest. The pain or discomfort usually starts behind the breastbone.
Pain from angina also can occur in the arms, shoulders, neck, jaw, throat, or back. The pain may feel like indigestion. Some people say that angina pain is hard to describe or that they can't tell exactly where the pain is coming from.
Signs and symptoms such as nausea (feeling sick to your stomach), fatigue (tiredness), shortness of breath, sweating, light-headedness, and weakness also may occur.
Women are more likely to feel discomfort in the neck, jaw, throat, abdomen, or back. Shortness of breath is more common in older people and those who have diabetes. Weakness, dizziness, and confusion can mask the signs and symptoms of angina in elderly people.
Symptoms also vary based on the type of angina you have.
Because angina has so many possible symptoms and causes, all chest pain should be checked by a doctor. Chest pain that lasts longer than a few minutes and isn't relieved by rest or angina medicine may be a sign of a heart attack. Call 9–1–1 right away.
The pain or discomfort:
The pain or discomfort:
The pain or discomfort:
The pain or discomfort:
The most important issues to address when you go to the doctor with chest pain are:
Angina is a symptom of an underlying heart problem, usually coronary heart disease (CHD). The type of angina pain you have can be a sign of how severe the CHD is and whether it's likely to cause a heart attack.
If you have chest pain, your doctor will want to find out whether it's angina. He or she also will want to know whether the angina is stable or unstable. If it's unstable, you may need emergency medical treatment to try to prevent a heart attack.
To diagnose chest pain as stable or unstable angina, your doctor will do a physical exam, ask about your symptoms, and ask about your risk factors for and your family history of CHD or other heart diseases.
Your doctor also may ask questions about your symptoms, such as:
If your doctor thinks that you have unstable angina or that your angina is related to a serious heart condition, he or she may recommend one or more tests.
An EKG is a simple, painless test that detects and records the heart’s electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage due to CHD and signs of a previous or current heart attack. However, some people who have angina have normal EKGs.
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can’t exercise, you may be given medicine to make your heart work hard and beat fast.
When your heart is working hard and beating fast, it needs more blood and oxygen. Plaque-narrowed arteries can't supply enough oxygen-rich blood to meet your heart's needs.
A stress test can show possible signs and symptoms of CHD, such as:
As part of some stress tests, pictures are taken of your heart while you exercise and while you rest. These imaging stress tests can show how well blood is flowing in various parts of your heart. They also can show how well your heart pumps blood when it beats.
A chest x ray takes pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels.
A chest x ray can reveal signs of heart failure. It also can show signs of lung disorders and other causes of symptoms not related to CHD. However, a chest x ray alone is not enough to diagnose angina or CHD.
Your doctor may recommend coronary angiography (an-jee-OG-ra-fee) if he or she suspects you have CHD. This test uses dye and special x rays to show the inside of your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-e-ter-ih-ZA-shun).
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through your coronary arteries. The dye lets your doctor study the flow of blood through your heart and blood vessels.
Cardiac catheterization usually is done in a hospital. You're awake during the procedure. It usually causes little or no pain, although you may feel some soreness in the blood vessel where your doctor inserts the catheter.
Computed tomography (to-MOG-rah-fee) angiography (CTA) uses dye and special x rays to show blood flow through the coronary arteries. This test is less invasive than coronary angiography with cardiac catheterization.
For CTA, a needle connected to an intravenous (IV) line is put into a vein in your hand or arm. Dye is injected through the IV line during the scan. You may have a warm feeling when this happens. The dye highlights your blood vessels on the CT scan pictures.
Sticky patches called electrodes are put on your chest. The patches are attached to an EKG machine to record your heart's electrical activity during the scan.
The CT scanner is a large machine that has a hollow, circular tube in the middle. You lie on your back on a sliding table. The table slowly slides into the opening of the machine.
Inside the scanner, an x-ray tube moves around your body to take pictures of different parts of your heart. A computer puts the pictures together to make a three-dimensional (3D) picture of the whole heart.
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may show that you have risk factors for CHD.
Your doctor may recommend a blood test to check the level of a protein called C-reactive protein (CRP) in your blood. Some studies suggest that high levels of CRP in the blood may increase the risk for CHD and heart attack.
Your doctor also may recommend a blood test to check for low levels of hemoglobin (HEE-muh-glow-bin) in your blood. Hemoglobin is an iron-rich protein in red blood cells. It helps the blood cells carry oxygen from the lungs to all parts of your body. If your hemoglobin level is low, you may have a condition called anemia (uh-NEE-me-uh).
Treatments for angina include lifestyle changes, medicines, medical procedures, cardiac rehabilitation (rehab), and other therapies. The main goals of treatment are to:
Lifestyle changes and medicines may be the only treatments needed if your symptoms are mild and aren't getting worse. If lifestyle changes and medicines don't control angina, you may need medical procedures or cardiac rehab.
Unstable angina is an emergency condition that requires treatment in a hospital.
Making lifestyle changes can help prevent episodes of angina. You can:
You also can make lifestyle changes that help lower your risk for coronary heart disease. One of the most important changes is to quit smoking. Smoking can damage and tighten blood vessels and raise your risk for CHD. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
For more information about how to quit smoking, go to the Diseases and Conditions Index (DCI) Smoking and Your Heart article and the National Heart, Lung, and Blood Institute’s (NHLBI’s) "Your Guide to a Healthy Heart."
Following a healthy diet is another important lifestyle change. A healthy diet can prevent or reduce high blood pressure and high blood cholesterol and help you maintain a healthy weight.
A healthy diet includes a variety of fruits and vegetables (including beans and peas). It also includes whole grains, lean meats, poultry without skin, seafood, and fat-free or low-fat milk and dairy products. A healthy diet also is low in sodium (salt), added sugars, solid fats, and refined grains.
For more information about following a healthy diet, go to the NHLBI’s “Your Guide to Lowering Your Blood Pressure With DASH” and the U.S. Department of Agriculture’s ChooseMyPlate.gov Web site. Both resources provide general information about healthy eating.
Other important lifestyle changes include:
Nitrates are the medicines most commonly used to treat angina. They relax and widen blood vessels. This allows more blood to flow to the heart, while reducing the heart’s workload.
Nitroglycerin (NI-tro-GLIS-er-in) is the most commonly used nitrate for angina. Nitroglycerin that dissolves under your tongue or between your cheek and gum is used to relieve angina episodes.
Nitroglycerin pills and skin patches are used to prevent angina episodes. However, pills and skin patches act too slowly to relieve pain during an angina attack.
Other medicines also are used to treat angina, such as beta blockers, calcium channel blockers, ACE inhibitors, oral antiplatelet medicines, or anticoagulants (blood thinners). These medicines can help:
People who have stable angina may be advised to get annual flu shots.
If lifestyle changes and medicines don't control angina, you may need a medical procedure to treat the underlying heart disease. Both angioplasty (AN-jee-oh-plas-tee) and coronary artery bypass grafting (CABG) are commonly used to treat heart disease.
Angioplasty opens blocked or narrowed coronary arteries. During angioplasty, a thin tube with a balloon or other device on the end is threaded through a blood vessel to the narrowed or blocked coronary artery.
Once in place, the balloon is inflated to push the plaque outward against the wall of the artery. This widens the artery and restores blood flow.
Angioplasty can improve blood flow to your heart and relieve chest pain. A small mesh tube called a stent usually is placed in the artery to help keep it open after the procedure.
During CABG, healthy arteries or veins taken from other areas in your body are used to bypass (that is, go around) your narrowed coronary arteries. Bypass surgery can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
You will work with your doctor to decide which treatment is better for you.
Your doctor may recommend cardiac rehab for angina or after angioplasty, CABG, or a heart attack. Cardiac rehab is a medically supervised program that can help improve the health and well-being of people who have heart problems.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians or nutritionists, and psychologists or other mental health specialists.
Rehab has two parts:
For more information about cardiac rehab, go to the DCI Cardiac Rehabilitation article.
Enhanced external counterpulsation (EECP) therapy is helpful for some people who have angina. Large cuffs, similar to blood pressure cuffs, are put on your legs. The cuffs are inflated and deflated in sync with your heartbeat.
EECP therapy improves the flow of oxygen-rich blood to your heart muscle and helps relieve angina. You typically get 35 1-hour treatments over 7 weeks.
You can prevent or lower your risk for angina and heart disease by making lifestyle changes and treating related conditions.
Healthy lifestyle choices can help prevent or delay angina and heart disease. To adopt a healthy lifestyle, you can:
For more information about these lifestyle changes, go to “How Is Angina Treated?” For more information about preventing and controlling heart disease risk factors, visit the Diseases and Conditions Index Coronary Heart Disease, Coronary Heart Disease Risk Factors, and Coronary Microvascular Disease articles.
You also can help prevent or delay angina and heart disease by treating related conditions, such as high blood cholesterol, high blood pressure, diabetes, and overweight or obesity.
If you have one or more of these conditions, talk with your doctor about how to control them. Follow your treatment plan and take all of your medicines as your doctor prescribes.
Angina isn't a heart attack, but it does increase your risk of having a heart attack. The risk is even higher if you have unstable angina. For these reasons, it's important that you know:
Stable angina usually occurs in a pattern. You should know:
After several episodes, you’ll learn the pattern of your angina. You’ll want to pay attention to whether the pattern changes. Pattern changes may include angina that occurs more often, lasts longer, is more severe, occurs without physical exertion, or doesn't go away with rest or medicines.
These changes may be a sign that your symptoms are getting worse or becoming unstable. You should seek medical help. Unstable angina suggests that you're at high risk for a heart attack very soon.
You should know what medicines you're taking, the purpose of each, how and when to take them, and possible side effects. Know exactly when and how to take fast-acting nitroglycerin or other nitrates to relieve chest pain.
Correctly storing your angina medicines and knowing when to replace them also is important. Your doctor can advise you about this.
If you have side effects from your medicines, let your doctor know. You should never stop taking your medicines without your doctor's approval.
Talk with your doctor if you have any questions or concerns about taking your angina medicines. Tell him or her about any other medicines you’re taking. Some medicines can cause serious problems if they're taken with nitrates or other angina medicines.
After several angina episodes, you’ll know the level of activity, stress, and other factors that trigger your angina. By knowing this, you can take steps to prevent or lessen the severity of episodes.
Know what level of physical exertion triggers your angina and try to stop and rest before chest pain starts. For example, if walking up a flight of stairs leads to chest pain, stop halfway and rest before continuing.
If chest pain occurs during physical exertion, stop and rest or take your angina medicine. The pain should go away in a few minutes. If the pain doesn't go away or lasts longer than usual, call 9–1–1 for emergency care.
Anger, arguing, and worrying are examples of emotional stress that can trigger angina. Try to avoid or limit situations that cause these emotions.
Exercise and relaxation can help relieve stress. Alcohol and drug use play a part in causing stress and don't relieve it. If stress is a problem for you, talk with your doctor about getting help for it.
If large meals lead to chest pain, eat smaller meals. Also, avoid eating rich foods.
Most people who have stable angina can continue their normal activities. This includes work, hobbies, and sexual relations. However, if you do very strenuous activities or have a stressful job, talk with your doctor.
Angina increases your risk for a heart attack. It’s important that you and your family know how and when to seek medical attention.
Talk with your doctor about making an emergency action plan. The plan should include making sure you and your family members know:
Discuss your emergency plan with your family members. Take action quickly if your chest pain becomes severe, lasts longer than a few minutes, or isn't relieved by rest or medicine.
Sometimes it’s hard to tell the difference between unstable angina and a heart attack. Both are emergencies, so you should call 9–1–1 right away.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. However, many questions remain about various diseases and conditions, including angina.
The NHLBI continues to support research aimed at learning more about angina. For example, the NHLBI currently is sponsoring a study called PROMISE.
This study compares computed tomography angiography (CTA) with stress testing in patients who have suspected coronary heart disease (CHD). The goal of this study is to show whether initial screening with CTA can improve the outcomes for patients who have CHD.
Research often depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they’re widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don’t directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You’ll learn about treatments and tests you may receive, and the benefits and risks they may pose. You’ll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you’ll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to angina, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
Source: NHLBI, NIH
Atrial fibrillation (A-tre-al fi-bri-LA-shun), or AF, is the most common type of arrhythmia (ah-RITH-me-ah). An arrhythmia is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
AF occurs if rapid, disorganized electrical signals cause the heart's two upper chambers—called the atria (AY-tree-uh)—to fibrillate. The term "fibrillate" means to contract very fast and irregularly.
In AF, blood pools in the atria. It isn't pumped completely into the heart's two lower chambers, called the ventricles (VEN-trih-kuls). As a result, the heart's upper and lower chambers don't work together as they should.
People who have AF may not feel symptoms. However, even when AF isn't noticed, it can increase the risk of stroke. In some people, AF can cause chest pain or heart failure, especially if the heart rhythm is very rapid.
AF may happen rarely or every now and then, or it may become an ongoing or long-term heart problem that lasts for years.
To understand AF, it helps to understand the heart's internal electrical system. The heart's electrical system controls the rate and rhythm of the heartbeat.
With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As the signal travels, it causes the heart to contract and pump blood.
Each electrical signal begins in a group of cells called the sinus node or sinoatrial (SA) node. The SA node is located in the right atrium. In a healthy adult heart at rest, the SA node sends an electrical signal to begin a new heartbeat 60 to 100 times a minute. (This rate may be slower in very fit athletes.)
From the SA node, the electrical signal travels through the right and left atria. It causes the atria to contract and pump blood into the ventricles.
The electrical signal then moves down to a group of cells called the atrioventricular (AV) node, located between the atria and the ventricles. Here, the signal slows down slightly, allowing the ventricles time to finish filling with blood.
The electrical signal then leaves the AV node and travels to the ventricles. It causes the ventricles to contract and pump blood to the lungs and the rest of the body. The ventricles then relax, and the heartbeat process starts all over again in the SA node.
For more information about the heart's electrical system and detailed animations, go to the Diseases and Conditions Index How the Heart Works article.
In AF, the heart's electrical signals don't begin in the SA node. Instead, they begin in another part of the atria or in the nearby pulmonary veins. The signals don't travel normally. They may spread throughout the atria in a rapid, disorganized way. This can cause the atria to fibrillate.
The faulty signals flood the AV node with electrical impulses. As a result, the ventricles also begin to beat very fast. However, the AV node can't send the signals to the ventricles as fast as they arrive. So, even though the ventricles are beating faster than normal, they aren't beating as fast as the atria.
Thus, the atria and ventricles no longer beat in a coordinated way. This creates a fast and irregular heart rhythm. In AF, the ventricles may beat 100 to 175 times a minute, in contrast to the normal rate of 60 to 100 beats a minute.
If this happens, blood isn't pumped into the ventricles as well as it should be. Also, the amount of blood pumped out of the ventricles to the body is based on the random atrial beats.
The body may get rapid, small amounts of blood and occasional larger amounts of blood. The amount will depend on how much blood has flowed from the atria to the ventricles with each beat.
Most of the symptoms of AF are related to how fast the heart is beating. If medicines or age slow the heart rate, the symptoms are minimized.
AF may be brief, with symptoms that come and go and end on their own. Or, the condition may be ongoing and require treatment. Sometimes AF is permanent, and medicines or other treatments can't restore a normal heart rhythm.
The animation below shows atrial fibrillation. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
The animation shows how the heart's electrical signal can begin somewhere other than the sinoatrial node. This causes the atria to beat very fast and irregularly.
People who have AF can live normal, active lives. For some people, treatment can restore normal heart rhythms.
For people who have permanent AF, treatment can help control symptoms and prevent complications. Treatment may include medicines, medical procedures, and lifestyle changes.
In paroxysmal (par-ok-SIZ-mal) atrial fibrillation (AF), the faulty electrical signals and rapid heart rate begin suddenly and then stop on their own. Symptoms can be mild or severe. They stop within about a week, but usually in less than 24 hours.
Persistent AF is a condition in which the abnormal heart rhythm continues for more than a week. It may stop on its own, or it can be stopped with treatment.
Permanent AF is a condition in which a normal heart rhythm can't be restored with treatment. Both paroxysmal and persistent AF may become more frequent and, over time, result in permanent AF.
Atrial fibrillation (AF) occurs if the heart's electrical signals don't travel through the heart in a normal way. Instead, they become very rapid and disorganized.
Damage to the heart's electrical system causes AF. The damage most often is the result of other conditions that affect the health of the heart, such as high blood pressure and coronary heart disease.
The risk of AF increases as you age. Inflammation also is thought to play a role in causing AF.
Sometimes, the cause of AF is unknown.
Atrial fibrillation (AF) affects millions of people, and the number is rising. Men are more likely than women to have the condition. In the United States, AF is more common among Whites than African Americans or Hispanic Americans.
The risk of AF increases as you age. This is mostly because your risk for heart disease and other conditions that can cause AF also increases as you age. However, about half of the people who have AF are younger than 75.
AF is uncommon in children.
AF is more common in people who have:
AF also is more common in people who are having heart attacks or who have just had surgery.
Other conditions that raise your risk for AF include hyperthyroidism (too much thyroid hormone), obesity, diabetes, and lung disease.
Certain factors also can raise your risk for AF. For example, drinking large amounts of alcohol, especially binge drinking, raises your risk. Even modest amounts of alcohol can trigger AF in some people. Caffeine or psychological stress also may trigger AF in some people.
Some data suggest that people who have sleep apnea are at greater risk for AF. Sleep apnea is a common disorder that causes one or more pauses in breathing or shallow breaths while you sleep.
Metabolic syndrome also raises your risk for AF. Metabolic syndrome is the name for a group of risk factors that raises your risk for CHD and other health problems, such as diabetes and stroke.
Research suggests that people who receive high-dose steroid therapy are at increased risk for AF. This therapy is used for asthma and some inflammatory conditions. It may act as a trigger in people who have other AF risk factors.
Genetic factors also may play a role in causing AF. However, their role isn't fully known.
Atrial fibrillation (AF) usually causes the heart's lower chambers, the ventricles, to contract faster than normal.
When this happens, the ventricles can't completely fill with blood. Thus, they may not be able to pump enough blood to the lungs and body. This can lead to signs and symptoms, such as:
AF has two major complications—stroke and heart failure.
During AF, the heart's upper chambers, the atria, don't pump all of their blood to the ventricles. Some blood pools in the atria. When this happens, a blood clot (also called a thrombus) can form.
If the clot breaks off and travels to the brain, it can cause a stroke. (A clot that forms in one part of the body and travels in the bloodstream to another part of the body is called an embolus.)
Blood-thinning medicines that reduce the risk of stroke are an important part of treatment for people who have AF.
Heart failure occurs if the heart can't pump enough blood to meet the body's needs. AF can lead to heart failure because the ventricles are beating very fast and can't completely fill with blood. Thus, they may not be able to pump enough blood to the lungs and body.
Fatigue and shortness of breath are common symptoms of heart failure. A buildup of fluid in the lungs causes these symptoms. Fluid also can build up in the feet, ankles, and legs, causing weight gain.
Lifestyle changes, medicines, and procedures or surgery (rarely, a mechanical heart pump or heart transplant) are the main treatments for heart failure.
Atrial fibrillation (AF) is diagnosed based on your medical and family histories, a physical exam, and the results from tests and procedures.
Sometimes AF doesn't cause signs or symptoms. Thus, it may be found during a physical exam or EKG (electrocardiogram) test done for another purpose.
If you have AF, your doctor will want to find out what is causing it. This will help him or her plan the best way to treat the condition.
Primary care doctors often are involved in the diagnosis and treatment of AF. These doctors include family practitioners and internists.
Doctors who specialize in the diagnosis and treatment of heart disease also may be involved, such as:
Your doctor will likely ask questions about your:
Your doctor will do a complete cardiac exam. He or she will listen to the rate and rhythm of your heartbeat and take your pulse and blood pressure reading. Your doctor will likely check for any signs of heart muscle or heart valve problems. He or she will listen to your lungs to check for signs of heart failure.
Your doctor also will check for swelling in your legs or feet and look for an enlarged thyroid gland or other signs of hyperthyroidism (too much thyroid hormone).
An EKG is a simple, painless test that records the heart's electrical activity. It's the most useful test for diagnosing AF.
An EKG shows how fast your heart is beating and its rhythm (steady or irregular). It also records the strength and timing of electrical signals as they pass through your heart.
A standard EKG only records the heartbeat for a few seconds. It won't detect AF that doesn't happen during the test. To diagnose paroxysmal AF, your doctor may ask you to wear a portable EKG monitor that can record your heartbeat for longer periods.
The two most common types of portable EKGs are Holter and event monitors.
A Holter monitor records the heart's electrical activity for a full 24- or 48-hour period. You wear small patches called electrodes on your chest. Wires connect these patches to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
You wear the Holter monitor while you do your normal daily activities. This allows the monitor to record your heart for a longer time than a standard EKG.
An event monitor is similar to a Holter monitor. You wear an event monitor while doing your normal activities. However, an event monitor only records your heart's electrical activity at certain times while you're wearing it.
For many event monitors, you push a button to start the monitor when you feel symptoms. Other event monitors start automatically when they sense abnormal heart rhythms.
You can wear an event monitor for weeks or until symptoms occur.
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can't exercise, you may be given medicine to make your heart work hard and beat fast.
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
This test sometimes is called transthoracic (trans-thor-AS-ik) echocardiography. It's painless and noninvasive (no instruments are inserted into the body). For the test, a device called a transducer is moved back and forth over your chest. The device sends special sound waves through your chest wall to your heart.
The sound waves bounce off the structures of your heart, and a computer converts them into pictures on a screen.
Transesophageal (trans-e-SOF-ah-ge-al) echo, or TEE, uses sound waves to take pictures of your heart through the esophagus. The esophagus is the passage leading from your mouth to your stomach.
Your heart's upper chambers, the atria, are deep in your chest. They often can't be seen very well using transthoracic echo. Your doctor can see the atria much better using TEE.
During this test, the transducer is attached to the end of a flexible tube. The tube is guided down your throat and into your esophagus. You'll likely be given medicine to help you relax during the procedure.
TEE is used to detect blood clots that may be forming in the atria because of AF.
A chest x ray is a painless test that creates pictures of the structures in your chest, such as your heart and lungs. This test can show fluid buildup in the lungs and signs of other AF complications.
Blood tests check the level of thyroid hormone in your body and the balance of your body's electrolytes. Electrolytes are minerals that help maintain fluid levels and acid-base balance in the body. They're essential for normal health and functioning of your body's cells and organs.
Treatment for atrial fibrillation (AF) depends on how often you have symptoms, how severe they are, and whether you already have heart disease. General treatment options include medicines, medical procedures, and lifestyle changes.
The goals of treating AF include:
People who have AF but don't have symptoms or related heart problems may not need treatment. AF may even go back to a normal heart rhythm on its own. (This also can occur in people who have AF with symptoms.)
In some people who have AF for the first time, doctors may choose to use an electrical procedure or medicine to restore a normal heart rhythm.
Repeat episodes of AF tend to cause changes to the heart's electrical system, leading to persistent or permanent AF. Most people who have persistent or permanent AF need treatment to control their heart rate and prevent complications.
People who have AF are at increased risk for stroke. This is because blood can pool in the heart's upper chambers (the atria), causing a blood clot to form. If the clot breaks off and travels to the brain, it can cause a stroke.
Preventing blood clots from forming is probably the most important part of treating AF. The benefits of this type of treatment have been proven in multiple studies.
Doctors prescribe blood-thinning medicines to prevent blood clots. These medicines include warfarin (Coumadin®), dabigatran, heparin, and aspirin.
People taking blood-thinning medicines need regular blood tests to check how well the medicines are working.
Doctors can prescribe medicines to slow down the rate at which the ventricles are beating. These medicines help bring the heart rate to a normal level.
Rate control is the recommended treatment for most patients who have AF, even though an abnormal heart rhythm continues and the heart doesn't work as well as it should. Most people feel better and can function well if their heart rates are well-controlled.
Medicines used to control the heart rate include beta blockers (for example, metoprolol and atenolol), calcium channel blockers (diltiazem and verapamil), and digitalis (digoxin). Several other medicines also are available.
Restoring and maintaining a normal heart rhythm is a treatment approach recommended for people who aren't doing well with rate control treatment. This treatment also may be used for people who have only recently started having AF. The long-term benefits of rhythm control have not been proven conclusively yet.
Doctors use medicines or procedures to control the heart's rhythm. Patients often begin rhythm control treatment in a hospital so that their hearts can be closely watched.
The longer you have AF, the less likely it is that doctors can restore a normal heart rhythm. This is especially true for people who have had AF for 6 months or more.
Restoring a normal rhythm also becomes less likely if the atria are enlarged or if any underlying heart disease worsens. In these cases, the chance that AF will recur is high, even if you're taking medicine to help convert AF to a normal rhythm.
Medicines. Medicines used to control the heart rhythm include amiodarone, sotalol, flecainide, propafenone, dofetilide, and ibutilide. Sometimes older medicines—such as quinidine, procainamide, and disopyramide—are used.
Your doctor will carefully tailor the dose and type of medicines he or she prescribes to treat your AF. This is because medicines used to treat AF can cause a different kind of arrhythmia.
These medicines also can harm people who have underlying diseases of the heart or other organs. This is especially true for patients who have an unusual heart rhythm problem called Wolff-Parkinson-White syndrome.
Your doctor may start you on a small dose of medicine and then gradually increase the dose until your symptoms are controlled. Medicines used for rhythm control can be given regularly by injection at a doctor's office, clinic, or hospital. Or, you may routinely take pills to try to control AF or prevent repeat episodes.
If your doctor knows how you'll react to a medicine, a specific dose may be prescribed for you to take on an as-needed basis if you have an episode of AF.
Procedures. Doctors use several procedures to restore a normal heart rhythm. For example, they may use electrical cardioversion to treat a fast or irregular heartbeat. For this procedure, low-energy shocks are given to your heart to trigger a normal rhythm. You're temporarily put to sleep before you receive the shocks.
Electrical cardioversion isn't the same as the emergency heart shocking procedure often seen on TV programs. It's planned in advance and done under carefully controlled conditions.
Before doing electrical cardioversion, your doctor may recommend transesophageal echocardiography (TEE). This test can rule out the presence of blood clots in the atria. If clots are present, you may need to take blood-thinning medicines before the procedure. These medicines can help get rid of the clots.
Catheter ablation (ab-LA-shun) may be used to restore a normal heart rhythm if medicines or electrical cardioversion don't work. For this procedure, a wire is inserted through a vein in the leg or arm and threaded to the heart.
Radio wave energy is sent through the wire to destroy abnormal tissue that may be disrupting the normal flow of electrical signals. An electrophysiologist usually does this procedure in a hospital. Your doctor may recommend a TEE before catheter ablation to check for blood clots in the atria.
Sometimes doctors use catheter ablation to destroy the atrioventricular (AV) node. The AV node is where the heart's electrical signals pass from the atria to the ventricles (the heart's lower chambers). This procedure requires your doctor to surgically implant a device called a pacemaker, which helps maintain a normal heart rhythm.
Research on the benefits of catheter ablation as a treatment for AF is still ongoing. (For more information, go to the "Clinical Trials" section of this article.)
Another procedure to restore a normal heart rhythm is called maze surgery. For this procedure, the surgeon makes small cuts or burns in the atria. These cuts or burns prevent the spread of disorganized electrical signals.
This procedure requires open-heart surgery, so it's usually done when a person requires heart surgery for other reasons, such as for heart valve disease (which can increase the risk of AF).
Your doctor may recommend treatments for an underlying cause of AF or to reduce AF risk factors. For example, he or she may prescribe medicines to treat an overactive thyroid, lower high blood pressure, or manage high blood cholesterol.
Your doctor also may recommend lifestyle changes, such as following a healthy diet, cutting back on salt intake (to help lower blood pressure), quitting smoking, and reducing stress.
Limiting or avoiding alcohol, caffeine, or other stimulants that may increase your heart rate also can help reduce your risk for AF.
Following a healthy lifestyle and taking steps to lower your risk for heart disease may help you prevent atrial fibrillation (AF). These steps include:
If you already have heart disease or other AF risk factors, work with your doctor to manage your condition. In addition to adopting the healthy habits above, which can help control heart disease, your doctor may advise you to:
For more information about following a healthy lifestyle, visit the National Heart, Lung, and Blood Institute's Aim for a Healthy Weight Web site, "Your Guide to a Healthy Heart," "Your Guide to Lowering Your Blood Pressure With DASH," and "Your Guide to Physical Activity and Your Heart."
People who have atrial fibrillation (AF)—even permanent AF—can live normal, active lives. If you have AF, ongoing medical care is important.
Keep all your medical appointments. Bring a list of all the medicines you're taking to every doctor and emergency room visit. This will help your doctor know exactly what medicines you're taking.
Follow your doctor's instructions for taking medicines. Be careful about taking over-the-counter medicines, nutritional supplements, and cold and allergy medicines. Some of these products contain stimulants that can trigger rapid heart rhythms. Also, some over-the-counter medicines can have harmful interactions with heart rhythm medicines.
Tell your doctor if your medicines are causing side effects, if your symptoms are getting worse, or if you have new symptoms.
If you're taking blood-thinning medicines, you'll need to be carefully monitored. For example, you may need routine blood tests to check how the medicines are working. Also, talk with your doctor about your diet. Some foods, such as leafy green vegetables, may interfere with warfarin, a blood-thinning medicine.
Ask your doctor about physical activity, weight control, and alcohol use. Find out what steps you can take to manage your condition.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. However, many questions remain about various diseases and conditions, including atrial fibrillation (AF).
The NHLBI continues to support research aimed at learning more about AF. For example, NHLBI-supported research on AF includes studies that explore:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
Some clinical trials compare two current treatments. For example, the NHLBI is supporting a trial that compares catheter ablation with rate control or rhythm control medicines in people who have AF.
The study results will help researchers understand which of these treatments is best, and whether one is better than another in certain situations. For more information about this study, go to https://www.cabanatrial.org.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to AF, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
Source: NHLBI, NIH
Hypertension (High Blood Pressure)
High blood pressure (HBP) is a serious condition that can lead to coronary heart disease, heart failure, stroke, kidney failure, and other health problems.
"Blood pressure" is the force of blood pushing against the walls of the arteries as the heart pumps blood. If this pressure rises and stays high over time, it can damage the body in many ways.
About 1 in 3 adults in the United States has HBP. The condition itself usually has no signs or symptoms. You can have it for years without knowing it. During this time, though, HBP can damage your heart, blood vessels, kidneys, and other parts of your body.
Knowing your blood pressure numbers is important, even when you're feeling fine. If your blood pressure is normal, you can work with your health care team to keep it that way. If your blood pressure is too high, treatment may help prevent damage to your body's organs.
Blood pressure is measured as systolic (sis-TOL-ik) and diastolic (di-ah-STOL-ik) pressures. "Systolic" refers to blood pressure when the heart beats while pumping blood. "Diastolic" refers to blood pressure when the heart is at rest between beats.
You most often will see blood pressure numbers written with the systolic number above or before the diastolic number, such as 120/80 mmHg. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
The table below shows normal blood pressure numbers for adults. It also shows which numbers put you at greater risk for health problems.
| Category | Systolic (top number) |
Diastolic (bottom number) |
|
|---|---|---|---|
| Normal | Less than 120 | And | Less than 80 |
| Prehypertension | 120–139 | Or | 80–89 |
| High blood pressure | |||
| Stage 1 | 140–159 | Or | 90–99 |
| Stage 2 | 160 or higher | Or | 100 or higher |
The ranges in the table apply to most adults (aged 18 and older) who don't have short-term serious illnesses.
Blood pressure doesn't stay the same all the time. It lowers as you sleep and rises when you wake up. Blood pressure also rises when you're excited, nervous, or active. If your numbers stay above normal most of the time, you're at risk for health problems. The risk grows as blood pressure numbers rise. "Prehypertension" means you may end up with HBP, unless you take steps to prevent it.
If you're being treated for HBP and have repeat readings in the normal range, your blood pressure is under control. However, you still have the condition. You should see your doctor and follow your treatment plan to keep your blood pressure under control.
Your systolic and diastolic numbers may not be in the same blood pressure category. In this case, the more severe category is the one you're in. For example, if your systolic number is 160 and your diastolic number is 80, you have stage 2 HBP. If your systolic number is 120 and your diastolic number is 95, you have stage 1 HBP.
If you have diabetes or chronic kidney disease, HBP is defined as 130/80 mmHg or higher. HBP numbers also differ for children and teens. (For more information, go to "How Is High Blood Pressure Diagnosed?")
Blood pressure tends to rise with age. Following a healthy lifestyle helps some people delay or prevent this rise in blood pressure.
People who have HBP can take steps to control it and reduce their risk for related health problems. Key steps include following a healthy lifestyle, having ongoing medical care, and following your treatment plan.
Sources: National Center for Health Statistics. (2007–2010). National Health and Nutrition Examination Survey; Centers for Disease Control and Prevention. (2011). Vital signs: prevalence, treatment, and control of hypertension, 1999–2002 and 2005–2008. MMWR: Morbidity & Mortality Weekly Report, 60(4), 103–108; National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program. (2004). The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
High blood pressure (HBP) also is called hypertension (HI-per-TEN-shun).
When HBP has no known cause, it might be called essential hypertension, primary hypertension, or idiopathic (id-ee-o-PATH-ick) hypertension.
When another condition causes HBP, it's sometimes called secondary hypertension.
Some people only have high systolic blood pressure. This condition is called isolated systolic hypertension (ISH). Many older adults have this condition. ISH can cause as much harm as HBP in which both numbers are too high.
Blood pressure tends to rise with age, unless you take steps to prevent or control it.
Some medical problems—such as chronic kidney disease, thyroid disease, and sleep apnea—may cause blood pressure to rise. Some medicines also may raise your blood pressure. Examples include asthma medicines (for example, corticosteroids) and cold-relief products.
Other medicines also can cause high blood pressure (HBP). If you have HBP, let your doctor know about all of the medicines you take, including over-the-counter products.
In some women, birth control pills, pregnancy, or hormone therapy (HT) may cause blood pressure to rise.
Women taking birth control pills usually have a small rise in both systolic and diastolic blood pressures. If you already have HBP and want to use birth control pills, make sure your doctor knows about your HBP. Talk with him or her about how often you should have your blood pressure checked and how to control it while taking the pill.
Taking HT to reduce the symptoms of menopause can cause a small rise in systolic blood pressure. If you already have HBP and want to start using HT, talk with your doctor about the risks and benefits. If you decide to take hormones, find out how to control your blood pressure and how often you should have it checked.
Children younger than 10 years old who have HBP often have another condition that's causing it (such as kidney disease). Treating the underlying condition may resolve the HBP.
The older a child is when HBP is diagnosed, the more likely he or she is to have essential hypertension. This means that doctors don't know what's causing the HBP.
High blood pressure (HBP) is a common condition. In the United States, about 1 in 3 adults has HBP.
Certain traits, conditions, and habits can raise your risk for HBP. The major risk factors for HBP are described below.
Blood pressure tends to rise with age. About 65 percent of Americans aged 60 or older have HBP.
Isolated systolic hypertension (ISH) is the most common form of HBP in older adults. ISH occurs when only systolic blood pressure (the top number) is high. About 2 out of 3 people over age 60 with HBP have ISH.
HBP doesn't have to be a routine part of aging. You can take steps to keep your blood pressure at a normal level. (For more information, go to "How Is High Blood Pressure Treated?")
HBP can affect anyone. However, it's more common in African American adults than in Caucasian or Hispanic American adults. In relation to these groups, African Americans:
HBP risks vary among different groups of Hispanic American adults. For instance, Puerto Rican American adults have higher rates of HBP-related death than all other Hispanic groups and Caucasians. However, Cuban Americans have lower rates of HBP-related death than Caucasians.
You're more likely to develop prehypertension or HBP if you're overweight or obese. The terms "overweight" and "obesity" refer to body weight that's greater than what is considered healthy for a certain height.
Men and women are equally likely to develop HBP during their lifetimes. However, before age 45, men are more likely to have HBP than women. After age 65, the condition is more likely to affect women than men.
Also, men younger than 55 are more likely to have uncontrolled HBP than women. However, after age 65, women are more likely to have uncontrolled HBP.
Many unhealthy lifestyle habits can raise your risk for HBP, including:
A family history of HBP raises your risk for the condition. Long-lasting stress also can put you at risk for HBP.
You're also more likely to develop HBP if you have prehypertension. Prehypertension means that your blood pressure is in the 120–139/80–89 mmHg range.
Prehypertension and HBP are becoming more common in children and teens. This is due in part to a rise in overweight and obesity among children and teens.
African American and Mexican American youth are more likely to have HBP and prehypertension than Caucasian youth. Also, boys are at higher risk for HBP than girls.
Like adults, children and teens need to have routine blood pressure checks, especially if they're overweight.
High blood pressure (HBP) itself usually has no signs or symptoms. Rarely, headaches may occur.
You can have HBP for years without knowing it. During this time, the condition can damage your heart, blood vessels, kidneys, and other parts of your body.
Some people only learn that they have HBP after the damage has caused problems, such as coronary heart disease, stroke, or kidney failure.
Knowing your blood pressure numbers is important, even when you're feeling fine. If your blood pressure is normal, you can work with your health care team to keep it that way. If your blood pressure is too high, you can take steps to lower it. Lowering your blood pressure will help reduce your risk for related health problems.
When blood pressure stays high over time, it can damage the body. HBP can cause:
High blood pressure (HBP) is diagnosed using a blood pressure test. This test will be done several times to make sure the results are correct. If your numbers are high, your doctor may have you return for repeat tests to check your blood pressure over time.
If your blood pressure is 140/90 mmHg or higher over time, your doctor will likely diagnose you with HBP. If you have diabetes or chronic kidney disease, a blood pressure of 130/80 mmHg or higher is considered HBP.
The ranges for HBP in children are different, as discussed below.
A blood pressure test is easy and painless. This test is done at a doctor's office or clinic.
To prepare for the test:
To measure your blood pressure, your doctor or nurse will use some type of a gauge, a stethoscope (or electronic sensor), and a blood pressure cuff.
Most often, you will sit or lie down with the cuff around your arm as your doctor or nurse checks your blood pressure. If he or she doesn't tell you what your blood pressure numbers are, you should ask.
Doctors measure blood pressure in children and teens the same way they do in adults. Your child should have routine blood pressure checks starting at 3 years of age.
Blood pressure normally rises with age and body size. Newborn babies often have very low blood pressure numbers, while older teens have numbers similar to adults.
The ranges for normal blood pressure and HBP generally are lower for youth than for adults. To find out whether a child has HBP, a doctor will compare the child's blood pressure numbers to average numbers for his or her age, gender, and height.
For more information, go to the National Heart, Lung, and Blood Institute's "A Pocket Guide to Blood Pressure Measurement in Children."
If you're diagnosed with HBP, your doctor will prescribe treatment. Your blood pressure will be tested again to see how the treatment affects it.
Once your blood pressure is under control, you'll still need treatment. "Under control" means that your blood pressure numbers are in the normal range. Your doctor will likely recommend routine blood pressure tests. He or she can tell you how often you should be tested.
The sooner you find out about HBP and treat it, the better. Early treatment may help you avoid problems such as heart attack, stroke, and kidney failure.
High blood pressure (HBP) is treated with lifestyle changes and medicines.
Most people who have HBP will need lifelong treatment. Sticking to your treatment plan is important. It can help prevent or delay problems related to HBP and help you live and stay active longer.
For more tips on controlling your blood pressure, go to the National Heart, Lung, and Blood Institute's (NHLBI's) "Your Guide to Lowering Blood Pressure."
The treatment goal for most adults is to get and keep blood pressure below 140/90 mmHg. For adults who have diabetes or chronic kidney disease, the goal is to get and keep blood pressure below 130/80 mmHg.
Healthy lifestyle habits can help you control HBP. These habits include:
If you combine healthy lifestyle habits, you can achieve even better results than taking single steps.
You may find it hard to make lifestyle changes. Start by making one healthy lifestyle change and then adopt others.
Some people can control their blood pressure with lifestyle changes alone, but many people can't. Keep in mind that the main goal is blood pressure control.
If your doctor prescribes medicines as a part of your treatment plan, keep up your healthy lifestyle habits. They will help you better control your blood pressure.
Your doctor may recommend the DASH (Dietary Approaches to Stop Hypertension) eating plan if you have HBP. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart healthy and low in fat, cholesterol, and sodium (salt).
DASH also focuses on fat-free or low-fat dairy products, fish, poultry, and nuts. The DASH eating plan is reduced in red meats (including lean red meats), sweets, added sugars, and sugar-containing beverages. It's rich in nutrients, protein, and fiber.
To help control HBP, you should limit the amount of salt that you eat. This means choosing low-sodium and no added salt foods and seasonings at the table and while cooking. The Nutrition Facts label on food packaging shows the amount of sodium in an item. You should eat no more than about 1 teaspoon of salt a day.
Also, try to limit alcoholic drinks. Too much alcohol will raise your blood pressure. Men should have no more than two alcoholic drinks a day. Women should have no more than one alcoholic drink a day. One drink is a glass of wine, beer, or a small amount of hard liquor.
For more information, go to the NHLBI's "Your Guide to Lowering Your Blood Pressure With DASH."
Routine physical activity can lower HBP and reduce your risk for other health problems. Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. The more active you are, the more you will benefit.
For more information about physical activity, go to the U.S. Department of Health and Human Services' "2008 Physical Activity Guidelines for Americans," the Health Topics Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Maintaining a healthy weight can help you control HBP and reduce your risk for other health problems.
If you're overweight or obese, aim to reduce your weight by 5 to 10 percent during your first year of treatment. This amount of weight loss can lower your risk for health problems related to HBP.
To lose weight, cut back your calorie intake and do more physical activity. Eat smaller portions and choose lower calorie foods. Don't feel that you have to finish the entrees served at restaurants. Many restaurant portions are oversized and have too many calories for the average person.
After your first year of treatment, you may have to continue to lose weight so you can lower your body mass index (BMI) to less than 25. BMI measures your weight in relation to your height and gives an estimate of your total body fat.
A BMI between 25 and 29.9 is considered overweight. A BMI of 30 or more is considered obese. A BMI of less than 25 is the goal for controlling blood pressure.
You can use the NHLBI's online BMI calculator to figure out your BMI, or your doctor can help you.
For more information about losing weight and keeping it off, go to the Health Topics Overweight and Obesity article.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health.
Physical activity helps some people cope with stress. Other people listen to music or focus on something calm or peaceful to reduce stress. Some people learn yoga, tai chi, or how to meditate.
Today's blood pressure medicines can safely help most people control their blood pressure. These medicines are easy to take. The side effects, if any, tend to be minor.
If you have side effects from your medicines, talk with your doctor. He or she might adjust the doses or prescribe other medicines. You shouldn't decide on your own to stop taking your medicines.
Blood pressure medicines work in different ways to lower blood pressure. Some remove extra fluid and salt from the body to lower blood pressure. Others slow down the heartbeat or relax and widen blood vessels. Often, two or more medicines work better than one.
Diuretics sometimes are called water pills. They help your kidneys flush excess water and salt from your body. This reduces the amount of fluid in your blood, and your blood pressure goes down.
Diuretics often are used with other HBP medicines and sometimes combined into one pill.
Beta blockers help your heart beat slower and with less force. As a result, your heart pumps less blood through your blood vessels. This causes your blood pressure to go down.
ACE inhibitors keep your body from making a hormone called angiotensin II. This hormone normally causes blood vessels to narrow. ACE inhibitors prevent this, so your blood pressure goes down.
Angiotensin II receptor blockers are newer blood pressure medicines that protect your blood vessels from the angiotensin II hormone. As a result, blood vessels relax and widen, and your blood pressure goes down.
Calcium channel blockers keep calcium from entering the muscle cells of your heart and blood vessels. This allows blood vessels to relax, and your blood pressure goes down.
Alpha blockers reduce nerve impulses that tighten blood vessels. This allows blood to flow more freely, causing blood pressure to go down.
Alpha-beta blockers reduce nerve impulses the same way alpha blockers do. However, they also slow the heartbeat like beta blockers. As a result, blood pressure goes down.
Nervous system inhibitors increase nerve impulses from the brain to relax and widen blood vessels. This causes blood pressure to go down.
Vasodilators relax the muscles in blood vessel walls. This causes blood pressure to go down.
If another condition is causing your child's HBP, treating it often resolves the HBP. When the cause of a child or teen's HBP isn't known, the first line of treatment is lifestyle changes (as it is for adults).
If lifestyle changes don't control blood pressure, children and teens also may need to take medicines. Most of the medicines listed above for adults have special doses for children.
If you don't have high blood pressure (HBP), you can take steps to prevent it. Healthy lifestyle habits can help you maintain normal blood pressure.
Many people who adopt these healthy lifestyle habits are able to prevent or delay HBP. The more lifestyle changes you make, the more likely you are to lower your blood pressure and avoid related health problems.
For more information about healthy lifestyle habits, go to "How Is High Blood Pressure Treated?"
If you have HBP, you can still take steps to prevent the long-term problems it can cause. Healthy lifestyle habits (listed above) and medicines can help you live a longer, more active life.
Follow the treatment plan your doctor prescribes to control your blood pressure. Treatment can help you prevent or delay coronary heart disease, stroke, kidney disease, and other health problems.
A healthy lifestyle also can help prevent HBP in children and teens. Key steps include having a child:
Make these healthy habits part of a family health plan to help your child adopt and maintain a healthy lifestyle.
If you have high blood pressure (HBP), you'll need to treat and control it for life. This means making lifestyle changes, taking prescribed medicines, and getting ongoing medical care.
Treatment can help control blood pressure, but it will not cure HBP. If you stop treatment, your blood pressure and risk for related health problems will rise.
For a healthy future, follow your treatment plan closely. Work with your health care team for lifelong blood pressure control.
Making healthy lifestyle changes can help control HBP. A healthy lifestyle includes following a healthy diet, being physically active, and maintaining a healthy weight. (For more information, go to "How Is High Blood Pressure Treated?")
Take all blood pressure medicines that your doctor prescribes. Know the names and doses of your medicines and how to take them. If you have questions about your medicines, talk with your doctor or pharmacist.
Make sure you refill your medicines before they run out. Take your medicines exactly as your doctor directs—don't skip days or cut pills in half.
If you're having side effects from your medicines, talk with your doctor. He or she may need to adjust the doses or prescribe other medicines. You shouldn't decide on your own to stop taking your medicines.
If you have HBP, have medical checkups or tests as your doctor advises. Your doctor may need to change or add medicines to your treatment plan over time. Routine checkups allow your doctor to change your treatment right away if your blood pressure goes up again.
Keeping track of your blood pressure is important. Have your blood pressure checked on the schedule your doctor advises.
You may want to learn how to check your blood pressure at home. Your doctor can help you learn how to do this. Each time you check your own blood pressure, you should write down your numbers and the date.
The National Heart, Lung, and Blood Institute's (NHLBI's) "My Blood Pressure Wallet Card" can help you track your blood pressure. You also can write down the names and doses of your medicines and keep track of your lifestyle changes with this handy card.
During checkups, you can ask your doctor or health care team any questions you have about your treatments. For possible questions you may want to ask your doctor, go to the NHLBI's Questions to Ask Your Doctor If You Have High Blood Pressure Web page.
Many pregnant women who have HBP have healthy babies. However, HBP can cause problems for both the mother and the fetus. HBP can harm the mother's kidneys and other organs. It also can cause the baby to be born early and with a low birth weight.
If you're thinking about having a baby and you have HBP, talk with your health care team. You can take steps to control your blood pressure before and while you're pregnant.
Some women get HBP for the first time while they're pregnant. In the most serious cases, the mother has a condition called preeclampsia (pre-eh-KLAMP-se-ah).
This condition can threaten the lives of both the mother and the unborn child. You'll need special care to reduce your risk. With such care, most women and babies have good outcomes.
Go to the NHLBI's Your Guide to Lowering High Blood Pressure Web site for more information about HBP and pregnancy.
Source: NHLBI, NIH
High Blood Pressure in the Elderly

Blood pressure is the force of blood pushing against the walls of the blood vessels as the heart pumps blood. If your blood pressure rises and stays high over time, it’s called high blood pressure. High blood pressure is dangerous because it makes the heart work too hard, and the high force of the blood flow can harm arteries and organs such as the heart, kidneys, brain, and eyes.
The pressure of blood against the artery walls when your heart beats is called systolic pressure. The pressure between beats when your heart relaxes is called diastolic pressure.
Blood pressure is always given as two numbers, the systolic and diastolic pressures. Both are important. Usually they are written one above or before the other -- for example, 120/80 mmHg. The top, or first, number is the systolic and the bottom, or second number, is the diastolic. If your blood pressure is 120/80, you say that it is "120 over 80."
Your blood pressure changes throughout the day. It is usually lowest when you're asleep, and it rises when you awaken. It also can rise when you are excited, nervous, or active. So it varies throughout the day.
Systolic blood pressure of 140 mmHg or higher, or a diastolic blood pressure of 90 mmHg or higher, is considered high blood pressure, or hypertension. Hypertension is the medical term for high blood pressure.
If you have diabetes or chronic kidney disease, your recommended blood pressure levels are a systolic blood pressure of 130 mmHg or lower, and a diastolic blood pressure of 80 mmHg or lower.
High blood pressure currently affects nearly 1 in every 3 American adults.
High blood pressure is often called "the silent killer" because it usually has no symptoms. Occasionally, headaches may occur. Some people may not find out they have high blood pressure until they have trouble with their heart, kidneys, or eyes. When high blood pressure is not diagnosed and treated, it can lead to other life-threatening conditions, including heart attack, heart failure, stroke, and kidney failure. It can also lead to vision changes or blindness.
Over time, high blood pressure can cause
A blood pressure reading of 120/80 mmHg or less is considered normal. Usually, the lower, the better, although very low blood pressure can sometimes be a cause for concern and should be checked out by your doctor.

If either your systolic or diastolic blood pressure is higher than normal (120/80) but not high enough to be considered high blood pressure (140/90), you have pre-hypertension. Pre-hypertension is a top number between 120 and 139 or a bottom number between 80 and 89 mmHg. For example, blood pressure readings of 138/82, 128/70, or 115/86 are all in the "pre-hypertension" range. (See the chart on the right for more information.)
If you have pre-hypertension, your chances of developing high blood pressure are greater than average unless you take action to prevent it. In fact, having pre-hypertension doubles a woman's chances of having heart disease or a stroke. That's a 100 percent increase. For men, the increase is 45 percent. Talk to your health care provider about lifestyle changes you can make to lower your blood pressure and prevent hypertension.
About two out of every three people over the age of 60 who have high blood pressure have isolated systolic hypertension. This means that only the top number, the systolic pressure, is high (140 mmHg or higher). Isolated systolic hypertension can be as harmful as when both numbers are high.
You may have isolated systolic hypertension and feel fine. As with other types of high blood pressure, it often causes no symptoms.
When your systolic and diastolic pressures fall into different categories, the more severe category is used to classify your blood pressure level. For example, 160/80 mmHg is considered stage 2 high blood pressure even though a diastolic pressure of 80 mmHg is in the pre-hypertension range.
Nearly 1 in 3 American adults have high blood pressure. Many people get high blood pressure as they get older. In fact, about two thirds of Americans age 60 and older have high blood pressure. However, getting high blood pressure is not a normal part of aging. There are things you can do to help keep your blood pressure normal, such as eating a healthy diet and getting more exercise.
Anyone can develop high blood pressure. But your chances of getting high blood pressure are higher if you

Other things that increase your chances of developing high blood pressure are

In the U.S., high blood pressure occurs more often in African Americans. Compared to other groups, blacks
You can take steps to prevent high blood pressure by adopting these healthy lifestyle habits.

More than 2 out of 3 Americans ages 20-74 are either overweight or obese. Overweight and obesity increase your chances of developing high blood pressure and diabetes, which, in turn, increase your chances of developing heart disease. Blood pressure rises as body weight increases. Losing even 10 pounds can lower blood pressure -- and it has the greatest effect for those who are overweight and already have hypertension.
Talk to your health care provider about lifestyle changes that can lower your blood pressure and prevent hypertension. If you are overweight or obese, work with your health care provider to develop a plan to help you reduce your weight and maintain a healthy weight. Aim to reduce your weight by 7 to 10 percent over six months, which can lower your risk for health problems. For example, if you are overweight at 200 pounds, try to lose 14 to 20 pounds over six months. After that, you may have to continue to lose weight to get to a healthy weight.
How do you know if you’re overweight? Two key measures are used to determine if someone is overweight or obese. These are body mass index, or BMI, and waist circumference.
Body mass index (BMI) is a measure of weight in relation to height, and provides an estimate of your total body fat. It applies to both men and women, but it does have some limits.
That’s why waist measurement is often checked as well. Another reason is that too much body fat in the stomach area also increases disease risk. A waist measurement of more than 35 inches in women and more than 40 inches in men is considered high.
Overweight is defined as a BMI of 25 to 29.9; obesity is defined as a BMI greater than or equal to 30. As your BMI goes up, so do your chances of getting high blood pressure, heart disease, and other health problems.

A portion of a body mass index chart is on the right. The full chart is available from NHLBI (National Heart, Lung, and Blood Institute).
If you need to lose weight, it’s important to do so slowly. Lose no more than 1/2 pound to 2 pounds a week. Begin with a goal of losing 10 percent of your current weight. This is the healthiest way to lose weight and offers the best chance of long-term success.
There’s no magic formula for weight loss. You have to eat fewer calories than you use up in daily activities. Just how many calories you burn daily depends on factors such as your body size and how physically active you are.
One pound equals 3,500 calories. So, to lose 1 pound a week, you need to eat 500 calories a day less or burn 500 calories a day more than you usually do. It’s best to work out some combination of both eating less and being more physically active.
And remember to be aware of serving sizes. It’s not only what you eat that adds calories, but also how much. As you lose weight, be sure to follow a healthy eating plan that includes a variety of foods.
Following an eating plan that emphasizes fruits, vegetables, fat-free or low-fat milk and milk products, and whole grains, and that is low in saturated fat, cholesterol, and total fat is even more effective when you also reduce your sodium (salt) intake and calories.

One such eating plan is called DASH. DASH stands for Dietary Approaches to Stop Hypertension. This is the name of a study sponsored by the National Institutes of Health that showed that this kind of eating plan can help you prevent and control high blood pressure. The study also showed that combining this kind of eating plan with cutting back on salt in your diet is even more effective at lowering your blood pressure.
To learn more about DASH, see Lowering Your Blood Pressure with DASH.

In general, the lower your salt intake, the lower your blood pressure. Older adults should limit their sodium intake to 1,500 milligrams (mg) daily (about 2/3 of a teaspoon of salt). The key to reducing the amount of salt we eat is making wise food choices. Only a small amount of the salt that we eat comes from the salt shaker, and only small amounts occur naturally in food. Most of the salt that we eat comes from processed foods -- for example, canned or processed meat, baked goods, certain cereals, soy sauce, and foods that contain seasoned salts, monosodium glutamate (MSG), and baking soda. Food from fast food restaurants, frozen foods, and canned foods also tend to be higher in sodium.
See tips to reduce salt in your diet.

Be sure to read food labels to choose products lower in salt. Look for foods and seasonings that are labeled as low-salt or "no added salt." Look for the sodium content in milligrams and the Percent Daily Value. Aim for foods that are less than 5 percent of the Daily Value of sodium. Foods with 20 percent or more Daily Value of sodium are considered high. You should eat no more than about 1 teaspoon, or 2300 mg, of salt a day.
To learn more about reading nutrition labels, see Reading the Label.

Being physically active is one of the most important steps you can take to prevent or control high blood pressure. It also helps reduce your risk of heart disease. Getting at least 2 and one-half hours of moderate exercise, or one hour and 15 minutes of vigorous activity, each week, preferably spread out across the week in at least 10-minute intervals, can help maintain or improve your cardiovascular health.
Most people don’t need to see a doctor before they start a moderate-level physical activity. You should check first with your doctor if you
See examples of exercises for older adults at Exercises to Try.
For more on exercise and physical activity for older adults, visit Go4Life®, the exercise and physical activity campaign from the National Institute on Aging.
If you drink alcoholic beverages, do so in moderation. Drinking too much alcohol can raise your blood pressure. Men should limit their intake to 2 drinks per day, and women should limit their intake to one drink per day.
See how drinking alcohol can affect you as you age.
2. Why are older people more sensitive to alcohol's effects than younger people?
One reason that older adults are more sensitive to alcohol's effects is that they metabolize, or break down, alcohol more slowly than younger people. So, alcohol stays in their bodies longer. Also, the amount of water in the body goes down with age. As a result, older adults will have a higher percentage of alcohol in their blood than younger people after drinking the same amount of alcohol.
Watch a video on how to cut back on drinking alcohol.
Smoking injures blood vessel walls and speeds up the process of hardening of the arteries. It increases your chances of stroke, heart disease, peripheral arterial disease, and several forms of cancer. If you smoke, quit. If you don't smoke, don't start. Once you quit, your risk of having a heart attack is reduced after the first year. So you have a lot to gain by quitting.
See how to start a smoking quit plan geared to older adults.
Now that you understand how your addiction affects your health and your loved ones, you have probably decided that now is the best time to quit. Creating your own Quit Plan is a good way to proceed. A Quit Plan can help you stay focused and motivated and can improve your chances of quitting for good.
Below are 8 Quit Plan Steps and 8 Quit Smoking Worksheets. Each worksheet corresponds to a step in the Quit Plan. The worksheets can help you get started and will guide you through the quit process. They will also provide you with a written record of your Quit Plan.
First, read the list of steps to see what a Quit Plan involves. Also watch the video above, "What's Involved in a Smoking Quit Plan?" Then download and complete the worksheet for the first step, "Pick A Quit Date." Proceed through the rest of the steps of the Quit Plan, using the appropriate worksheets, until you have completed the quit process. Keep your worksheets where you will see them often. Referring to them can help you through the hard times.
You have the option of completing the worksheets online and printing them out when you are done or printing out the worksheets first and then completing them by hand. When you exit a worksheet, you can choose to save the information to your computer or you can exit without saving it. The information you fill in on a worksheet will only be available to you. No other record of the information will be kept.
Select the eight worksheets in PDF or HTML formats:
High blood pressure is often called the "silent killer" because you can have it for years without knowing it. The only way to find out if you have high blood pressure is to have your blood pressure measured.

Most doctors will check your blood pressure several times on different days before making a diagnosis. Only if you have several readings of 140/90 mmHg or higher (or 130/80 mmHg or higher if you have diabetes or chronic kidney disease), will your doctor diagnose you with high blood pressure
Having your blood pressure measured is quick and easy. Your doctor or nurse will use some type of gauge, a stethoscope or electronic sensor, and a blood pressure cuff.

You should be sitting down and relaxed when your blood pressure is taken. There are other things you can do to prepare for the test.

Ask the doctor or nurse to tell you your blood pressure reading in numbers and to explain what the numbers mean. Write down your numbers or ask the doctor or nurse to write them down for you. (The wallet card on the right can be printed out and used to record your blood pressure numbers.)

You can also check your blood pressure at home with a home blood pressure measurement device or monitor. It is important that the blood pressure cuff fits you properly and that you understand how to use the monitor. A cuff that is too small, for example, can give you a reading that is higher than your actual blood pressure. Your doctor, nurse, or pharmacist can help you check the cuff size and teach you how to use it correctly. You may also ask for their help in choosing the right blood pressure monitor for you. Blood pressure monitors can be bought at discount chain stores and drug stores.
When you are taking your blood pressure at home, sit with your back supported and your feet flat on the floor. Rest your arm on a table at the level of your heart.
If you're diagnosed with high blood pressure, your doctor will prescribe treatment. Your blood pressure will be tested again to see how the treatment affects it.
Once your blood pressure is under control, you'll still need treatment. "Under control" means that your blood pressure numbers are in the normal range. Your doctor will likely recommend routine blood pressure tests. He or she can tell you how often you should be tested.
The sooner you find out about high blood pressure and treat it, the better. Early treatment may help you avoid problems such as heart attack, stroke and kidney failure.
See tips for talking with your doctor after you receive a medical diagnosis.
18. What questions should I ask my doctor once I am given a diagnosis?
A diagnosis identifies your disease or physical problem.
The doctor makes a diagnosis based on the symptoms you are experiencing and the results of the physical exam, laboratory work, and other tests.
Understanding your diagnosis, or health problem, can help you make decisions about what you would like to do about it. Also, if you know how the health problem may affect your life and activities and what may happen if the condition gets worse, you may be better prepared to deal with the problem.
Here are some questions you may want to ask your doctor about your health problem.
If you have high blood pressure, you will need to treat it and control it for life. This means making lifestyle changes, and, in some cases, taking prescribed medicines, and getting ongoing medical care.
In most cases, your goal is probably to keep your blood pressure below 140/90 mmHg (130/80 if you have diabetes or chronic kidney disease). Normal blood pressure is less than 120/80. Ask your doctor what your blood pressure goal should be.
Treatment can help control blood pressure, but it will not cure high blood pressure, even if your blood pressure readings appear normal. If you stop treatment, your blood pressure and risk for related health problems will rise. For a healthy future, follow your treatment plan closely. Work with your health care team for lifelong blood pressure control.

Some people can prevent or control high blood pressure with these healthy lifestyle habits.
If you combine healthy lifestyle habits, you can achieve even better results than taking single steps.
Although some people can control their high blood pressure with lifestyle changes alone, many people can't. Keep in mind that the main goal is blood pressure control. If your doctor prescribes medicines as a part of your treatment plan, keep up your healthy lifestyle habits. They will help you better control your blood pressure.

Blood pressure medicines work in different ways to lower blood pressure. Some drugs lower blood pressure by removing extra fluid and salt from your body. Others affect blood pressure by slowing down the heartbeat, or by relaxing and widening blood vessels. Often, two or more drugs work better than one.
Here are the types of medicines used to treat high blood pressure.
Check and record your blood pressure often to see if the medicine is working for you. If your blood pressure continues to measure 140/90 mmHg or higher (130/80 or higher if you have diabetes or chronic kidney disease) after you start taking medicine, your doctor may need to add a second drug or try you on different medicines until you find one that helps you reach your goal.
Don’t stop taking your medicine if your blood pressure is normal. That means the medicine is working.
Be sure to talk with your doctor or health care provider about side effects from your medications, and don't make any changes to your medications without talking with your doctor first.

It is important that you take your blood pressure medication the same time each day. There are a few tips to make this easier to remember.
Source: NIHSeniorHealth, NIH
Atherosclerosis (ath-er-o-skler-O-sis) is a disease in which plaque (plak) builds up inside your arteries. Arteries are blood vessels that carry oxygen-rich blood to your heart and other parts of your body.
Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows your arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body.
Atherosclerosis can lead to serious problems, including heart attack, stroke, or even death.
Atherosclerosis can affect any artery in the body, including arteries in the heart, brain, arms, legs, pelvis, and kidneys. As a result, different diseases may develop based on which arteries are affected.
Coronary heart disease (CHD), also called coronary artery disease, is the #1 killer of both men and women in the United States. CHD occurs if plaque builds up in the coronary arteries. These arteries supply oxygen-rich blood to your heart.
Plaque narrows the coronary arteries and reduces blood flow to your heart muscle. Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow.
If blood flow to your heart muscle is reduced or blocked, you may have angina (chest pain or discomfort) or a heart attack.
Plaque also can form in the heart's smallest arteries. This disease is called coronary microvascular disease (MVD). In coronary MVD, plaque doesn't cause blockages in the arteries as it does in CHD.
Carotid (ka-ROT-id) artery disease occurs if plaque builds up in the arteries on each side of your neck (the carotid arteries). These arteries supply oxygen-rich blood to your brain. If blood flow to your brain is reduced or blocked, you may have a stroke.
Peripheral arterial disease (P.A.D.) occurs if plaque builds up in the major arteries that supply oxygen-rich blood to your legs, arms, and pelvis.
If blood flow to these parts of your body is reduced or blocked, you may have numbness, pain, and, sometimes, dangerous infections.
Chronic kidney disease can occur if plaque builds up in the renal arteries. These arteries supply oxygen-rich blood to your kidneys.
Over time, chronic kidney disease causes a slow loss of kidney function. The main function of the kidneys is to remove waste and extra water from the body.
The cause of atherosclerosis isn't known. However, certain traits, conditions, or habits may raise your risk for the disease. These conditions are known as risk factors.
You can control some risk factors, such as lack of physical activity, smoking, and an unhealthy diet. Others you can't control, such as age and a family history of heart disease.
Some people who have atherosclerosis have no signs or symptoms. They may not be diagnosed until after a heart attack or stroke.
The main treatment for atherosclerosis is lifestyle changes. You also may need medicines and medical procedures. These treatments, along with ongoing medical care, can help you live a healthier life.
Improved treatments have reduced the number of deaths from atherosclerosis-related diseases. These treatments also have improved the quality of life for people who have these diseases. However, atherosclerosis remains a common health problem.
You may be able to prevent or delay atherosclerosis and the diseases it can cause. Making lifestyle changes and getting ongoing care can help you avoid the problems of atherosclerosis and live a long, healthy life.
The exact cause of atherosclerosis isn't known. However, studies show that atherosclerosis is a slow, complex disease that may start in childhood. It develops faster as you age.
Atherosclerosis may start when certain factors damage the inner layers of the arteries. These factors include:
Plaque may begin to build up where the arteries are damaged. Over time, plaque hardens and narrows the arteries. Eventually, an area of plaque can rupture (break open).
When this happens, blood cell fragments called platelets (PLATE-lets) stick to the site of the injury. They may clump together to form blood clots. Clots narrow the arteries even more, limiting the flow of oxygen-rich blood to your body.
Depending on which arteries are affected, blood clots can worsen angina (chest pain) or cause a heart attack or stroke.
Researchers continue to look for the causes of atherosclerosis. They hope to find answers to questions such as:
Coronary heart disease (atherosclerosis of the coronary arteries) is the #1 killer of both men and women in the United States.
The exact cause of atherosclerosis isn't known. However, certain traits, conditions, or habits may raise your risk for the disease. These conditions are known as risk factors. The more risk factors you have, the more likely it is that you'll develop atherosclerosis.
You can control most risk factors and help prevent or delay atherosclerosis. Other risk factors can't be controlled.
Although age and a family history of early heart disease are risk factors, it doesn't mean that you'll develop atherosclerosis if you have one or both. Controlling other risk factors often can lessen genetic influences and prevent atherosclerosis, even in older adults.
Studies show that an increasing number of children and youth are at risk for atherosclerosis. This is due to a number of causes, including rising childhood obesity rates.
Scientists continue to study other possible risk factors for atherosclerosis.
High levels of a protein called C-reactive protein (CRP) in the blood may raise the risk for atherosclerosis and heart attack. High levels of CRP are a sign of inflammation in the body.
Inflammation is the body's response to injury or infection. Damage to the arteries' inner walls seems to trigger inflammation and help plaque grow.
People who have low CRP levels may develop atherosclerosis at a slower rate than people who have high CRP levels. Research is under way to find out whether reducing inflammation and lowering CRP levels also can reduce the risk for atherosclerosis.
High levels of triglycerides (tri-GLIH-seh-rides) in the blood also may raise the risk for atherosclerosis, especially in women. Triglycerides are a type of fat.
Studies are under way to find out whether genetics may play a role in atherosclerosis risk.
Other factors also may raise your risk for atherosclerosis, such as:
Atherosclerosis usually doesn't cause signs and symptoms until it severely narrows or totally blocks an artery. Many people don't know they have the disease until they have a medical emergency, such as a heart attack or stroke.
Some people may have signs and symptoms of the disease. Signs and symptoms will depend on which arteries are affected.
The coronary arteries supply oxygen-rich blood to your heart. If plaque narrows or blocks these arteries (a disease called coronary heart disease, or CHD), a common symptom is angina. Angina is chest pain or discomfort that occurs when your heart muscle doesn't get enough oxygen-rich blood.
Angina may feel like pressure or squeezing in your chest. You also may feel it in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion. The pain tends to get worse with activity and go away with rest. Emotional stress also can trigger the pain.
Other symptoms of CHD are shortness of breath and arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat.
Plaque also can form in the heart's smallest arteries. This disease is called coronary microvascular disease (MVD). Symptoms of coronary MVD include angina, shortness of breath, sleep problems, fatigue (tiredness), and lack of energy.
The carotid arteries supply oxygen-rich blood to your brain. If plaque narrows or blocks these arteries (a disease called carotid artery disease), you may have symptoms of a stroke. These symptoms may include:
Plaque also can build up in the major arteries that supply oxygen-rich blood to the legs, arms, and pelvis (a disease called peripheral arterial disease).
If these major arteries are narrowed or blocked, you may have numbness, pain, and, sometimes, dangerous infections.
The renal arteries supply oxygen-rich blood to your kidneys. If plaque builds up in these arteries, you may develop chronic kidney disease. Over time, chronic kidney disease causes a slow loss of kidney function.
Early kidney disease often has no signs or symptoms. As the disease gets worse it can cause tiredness, changes in how you urinate (more often or less often), loss of appetite, nausea (feeling sick to the stomach), swelling in the hands or feet, itchiness or numbness, and trouble concentrating.
Your doctor will diagnose atherosclerosis based on your medical and family histories, a physical exam, and test results.
If you have atherosclerosis, a primary care doctor, such as an internist or family practitioner, may handle your care. Your doctor may recommend other health care specialists if you need expert care, such as:
During the physical exam, your doctor may listen to your arteries for an abnormal whooshing sound called a bruit (broo-E). Your doctor can hear a bruit when placing a stethoscope over an affected artery. A bruit may indicate poor blood flow due to plaque buildup.
Your doctor also may check to see whether any of your pulses (for example, in the leg or foot) are weak or absent. A weak or absent pulse can be a sign of a blocked artery.
Your doctor may recommend one or more tests to diagnose atherosclerosis. These tests also can help your doctor learn the extent of your disease and plan the best treatment.
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may be a sign that you're at risk for atherosclerosis.
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage caused by CHD. The test also can show signs of a previous or current heart attack.
A chest x ray takes pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels. A chest x ray can reveal signs of heart failure.
This test compares the blood pressure in your ankle with the blood pressure in your arm to see how well your blood is flowing. This test can help diagnose P.A.D.
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test provides information about the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
A computed tomography (CT) scan creates computer-generated pictures of the heart, brain, or other areas of the body. The test can show hardening and narrowing of large arteries.
A cardiac CT scan also can show whether calcium has built up in the walls of the coronary (heart) arteries. This may be an early sign of CHD.
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can't exercise, you may be given medicine to make your heart work hard and beat fast.
When your heart is working hard, it needs more blood and oxygen. Plaque-narrowed arteries can't supply enough oxygen-rich blood to meet your heart's needs.
A stress test can show possible signs and symptoms of CHD, such as:
As part of some stress tests, pictures are taken of your heart while you exercise and while you rest. These imaging stress tests can show how well blood is flowing in various parts of your heart. They also can show how well your heart pumps blood when it beats.
Angiography (an-jee-OG-ra-fee) is a test that uses dye and special x rays to show the inside of your arteries. This test can show whether plaque is blocking your arteries and how severe the blockage is.
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. Dye that can be seen on an x-ray picture is injected through the catheter into the arteries. By looking at the x-ray picture, your doctor can see the flow of blood through your arteries.
Other tests are being studied to see whether they can give a better view of plaque buildup in the arteries. Examples of these tests include magnetic resonance imaging (MRI) and positron emission tomography (PET).
Treatments for atherosclerosis may include lifestyle changes, medicines, and medical procedures or surgery.
The goals of treatment include:
Making lifestyle changes often can help prevent or treat atherosclerosis. For some people, these changes may be the only treatment needed.
A healthy diet is an important part of a healthy lifestyle. Following a healthy diet can prevent or reduce high blood pressure and high blood cholesterol and help you maintain a healthy weight.
For information about healthy eating, go to the National Heart, Lung, and Blood Institute's (NHLBI's) Aim for a Healthy Weight Web site. This site provides practical tips on healthy eating, physical activity, and weight control.
Therapeutic Lifestyle Changes (TLC). Your doctor may recommend TLC if you have high blood cholesterol. TLC is a three-part program that includes a healthy diet, physical activity, and weight management.
With the TLC diet, less than 7 percent of your daily calories should come from saturated fat. This kind of fat is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods.
No more than 25 to 35 percent of your daily calories should come from all fats, including saturated, trans, monounsaturated, and polyunsaturated fats.
You also should have less than 200 mg a day of cholesterol. The amounts of cholesterol and the types of fat in prepared foods can be found on the foods' Nutrition Facts labels.
Foods high in soluble fiber also are part of a healthy diet. They help prevent the digestive tract from absorbing cholesterol. These foods include:
A diet rich in fruits and vegetables can increase important cholesterol-lowering compounds in your diet. These compounds, called plant stanols or sterols, work like soluble fiber.
A healthy diet also includes some types of fish, such as salmon, tuna (canned or fresh), and mackerel. These fish are a good source of omega-3 fatty acids. These acids may help protect the heart from blood clots and inflammation and reduce the risk for heart attack. Try to have about two fish meals every week.
You should try to limit the amount of sodium (salt) that you eat. This means choosing low-salt and "no added salt" foods and seasonings at the table or while cooking. The Nutrition Facts label on food packaging shows the amount of sodium in the item.
Try to limit drinks with alcohol. Too much alcohol will raise your blood pressure and triglyceride level. (Triglycerides are a type of fat found in the blood.) Alcohol also adds extra calories, which will cause weight gain.
Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. One drink is a glass of wine, beer, or a small amount of hard liquor.
For more information about TLC, go to the NHLBI's "Your Guide to Lowering Your Cholesterol With TLC."
Dietary Approaches to Stop Hypertension (DASH). Your doctor may recommend the DASH eating plan if you have high blood pressure. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart healthy and low in fat, cholesterol, and salt.
DASH also focuses on fat-free or low-fat milk and dairy products, fish, poultry, and nuts. The DASH eating plan is reduced in red meats (including lean red meats), sweets, added sugars, and sugar-containing beverages. The plan is rich in nutrients, protein, and fiber.
The DASH eating plan is a good heart healthy eating plan, even for those who don't have high blood pressure. For more information, go to the NHLBI's "Your Guide to Lowering Your Blood Pressure With DASH."
Regular physical activity can lower many atherosclerosis risk factors, including LDL ("bad") cholesterol, high blood pressure, and excess weight.
Physical activity also can lower your risk for diabetes and raise your HDL cholesterol level. HDL is the "good" cholesterol that helps prevent atherosclerosis.
Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. For major health benefits, do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity or 75 minutes (1 hour and 15 minutes) of vigorous-intensity aerobic activity each week. The more active you are, the more you will benefit.
For more information about physical activity, go to the U.S. Department of Health and Human Services' "2008 Physical Activity Guidelines for Americans," the Diseases and Conditions Index (DCI) Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Maintaining a healthy weight can lower your risk for atherosclerosis. A general goal to aim for is a body mass index (BMI) of less than 25.
BMI measures your weight in relation to your height and gives an estimate of your total body fat. You can use the NHLBI's online BMI calculator to figure out your BMI, or your doctor can help you.
A BMI between 25 and 29.9 is considered overweight. A BMI of 30 or more is considered obese. A BMI of less than 25 is the goal for preventing and treating atherosclerosis. Your doctor or health care provider can help you set an appropriate BMI goal.
For more information about losing weight or maintaining your weight, go to the DCI Overweight and Obesity article.
If you smoke or use tobacco, quit. Smoking can damage and tighten blood vessels and raise your risk for atherosclerosis. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
For more information about how to quit smoking, go to the DCI Smoking and Your Heart article and the NHLBI's "Your Guide to a Healthy Heart."
Research shows that the most commonly reported "trigger" for a heart attack is an emotionally upsetting event—particularly one involving anger. Also, some of the ways people cope with stress—such as drinking, smoking, or overeating—aren't healthy.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress.
Physical activity, medicine, and relaxation therapy also can help relieve stress. You may want to consider taking part in a stress management program.
To slow the progress of plaque buildup, your doctor may prescribe medicines to help lower your cholesterol level or blood pressure. He or she also may prescribe medicines to prevent blood clots from forming.
For successful treatment, take all medicines as your doctor prescribes.
If you have severe atherosclerosis, your doctor may recommend a medical procedure or surgery.
Angioplasty (AN-jee-oh-plas-tee) is a procedure that's used to open blocked or narrowed coronary (heart) arteries. Angioplasty can improve blood flow to the heart and relieve chest pain. Sometimes a small mesh tube called a stent is placed in the artery to keep it open after the procedure.
Coronary artery bypass grafting (CABG) is a type of surgery. In CABG, arteries or veins from other areas in your body are used to bypass (that is, go around) your narrowed coronary arteries. CABG can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
Bypass grafting also can be used for leg arteries. For this surgery, a healthy blood vessel is used to bypass a narrowed or blocked artery in one of the legs. The healthy blood vessel redirects blood around the blocked artery, improving blood flow to the leg.
Carotid endarterectomy (END-ar-ter-EK-to-me) is surgery to remove plaque buildup from the carotid arteries in the neck. This procedure restores blood flow to the brain, which can help prevent a stroke.
Taking action to control your risk factors can help prevent or delay atherosclerosis and its related diseases. Your risk for atherosclerosis increases with the number of risk factors you have.
One step you can take is to adopt a healthy lifestyle. Following a healthy diet is an important part of a healthy lifestyle.
A healthy diet includes a variety of fruits and vegetables (including beans and peas). It also includes whole grains, lean meats, poultry without skin, seafood, and fat-free or low-fat milk and dairy products. A healthy diet is low in sodium (salt), added sugar, solid fats, and refined grains.
The National Heart, Lung, and Blood Institute's (NHLBI's) Therapeutic Lifestyle Changes (TLC) and Dietary Approaches to Stop Hypertension (DASH) are two programs that promote healthy eating.
If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan. Controlling your weight helps you control atherosclerosis risk factors.
Be as physically active as you can. Physical activity can improve your fitness level and your health. Ask your doctor what types and amounts of activity are safe for you.
For more information about physical activity, go to the Diseases and Conditions Index (DCI) Physical Activity and Your Heart article and the NHLBI's "Your Guide to Physical Activity and Your Heart."
If you smoke, quit. Smoking can damage and tighten blood vessels and raise your risk for atherosclerosis. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
For more information about quitting smoking, go to the DCI Smoking and Your Heart article and the NHLBI's "Your Guide to a Healthy Heart."
Know your family history of atherosclerosis. If you or someone in your family has an atherosclerosis-related disease, be sure to tell your doctor.
If lifestyle changes aren't enough, your doctor may prescribe medicines to control your atherosclerosis risk factors. Take all of your medicines as your doctor advises.
For more information about lifestyle changes and medicines, go to "How Is Atherosclerosis Treated?"
Improved treatments have reduced the number of deaths from atherosclerosis-related diseases. These treatments also have improved the quality of life for people who have these diseases.
Adopting a healthy lifestyle may help you prevent or delay atherosclerosis and the problems it can cause. This, along with ongoing medical care, can help you avoid the problems of atherosclerosis and live a long, healthy life.
Researchers continue to look for ways to improve the health of people who have atherosclerosis or may develop it.
If you have atherosclerosis, work closely with your doctor and other health care providers to avoid serious problems, such as heart attack and stroke.
Follow your treatment plan and take all of your medicines as your doctor prescribes. Your doctor will let you know how often you should schedule office visits or blood tests. Be sure to let your doctor know if you have new or worsening symptoms.
Having an atherosclerosis-related disease may cause fear, anxiety, depression, and stress. Talk about how you feel with your doctor. Talking to a professional counselor also can help. If you're very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Community resources are available to help you learn more about atherosclerosis. Contact your local public health departments, hospitals, and local chapters of national health organizations to learn more about available resources in your area.
Talk about your lifestyle changes with your family and friends—whoever can provide support or needs to understand why you're changing your habits.
Family and friends may be able to help you make lifestyle changes. For example, they can help you plan healthier meals. Because atherosclerosis tends to run in families, your lifestyle changes may help many of your family members too.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. However, many questions remain about various diseases and conditions, including atherosclerosis.
The NHLBI continues to support research aimed at learning more about atherosclerosis and its related diseases. For example, NHLBI-supported research includes studies that:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to atherosclerosis and its related diseases, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Source: NHLBI, NIH
Chronic Obstructive Pulmonary Disease (COPD)
What Is COPD?
COPD, or chronic obstructive pulmonary (PULL-mun-ary) disease, is a progressive disease that makes it hard to breathe. "Progressive" means the disease gets worse over time.
COPD can cause coughing that produces large amounts of mucus (a slimy substance), wheezing, shortness of breath, chest tightness, and other symptoms.
Cigarette smoking is the leading cause of COPD. Most people who have COPD smoke or used to smoke. Long-term exposure to other lung irritants—such as air pollution, chemical fumes, or dust—also may contribute to COPD.
To understand COPD, it helps to understand how the lungs work. The air that you breathe goes down your windpipe into tubes in your lungs called bronchial (BRONG-ke-al) tubes or airways.
Within the lungs, your bronchial tubes branch into thousands of smaller, thinner tubes called bronchioles (BRONG-ke-ols). These tubes end in bunches of tiny round air sacs called alveoli (al-VEE-uhl-eye).
Small blood vessels called capillaries (KAP-ih-lare-ees) run through the walls of the air sacs. When air reaches the air sacs, oxygen passes through the air sac walls into the blood in the capillaries. At the same time, carbon dioxide (a waste gas) moves from the capillaries into the air sacs. This process is called gas exchange.
The airways and air sacs are elastic (stretchy). When you breathe in, each air sac fills up with air like a small balloon. When you breathe out, the air sacs deflate and the air goes out.
In COPD, less air flows in and out of the airways because of one or more of the following:
Figure A shows the location of the lungs and airways in the body. The inset image shows a detailed cross-section of the bronchioles and alveoli. Figure B shows lungs damaged by COPD. The inset image shows a detailed cross-section of the damaged bronchioles and alveolar walls.
In the United States, the term "COPD" includes two main conditions—emphysema (em-fih-SE-ma) and chronic bronchitis (bron-KI-tis). (Note: The Health Topics article about bronchitis discusses both acute and chronic bronchitis.)
In emphysema, the walls between many of the air sacs are damaged. As a result, the air sacs lose their shape and become floppy. This damage also can destroy the walls of the air sacs, leading to fewer and larger air sacs instead of many tiny ones. If this happens, the amount of gas exchange in the lungs is reduced.
In chronic bronchitis, the lining of the airways is constantly irritated and inflamed. This causes the lining to thicken. Lots of thick mucus forms in the airways, making it hard to breathe.
Most people who have COPD have both emphysema and chronic bronchitis. Thus, the general term "COPD" is more accurate.
COPD is a major cause of disability, and it's the third leading cause of death in the United States. Currently, millions of people are diagnosed with COPD. Many more people may have the disease and not even know it.
COPD develops slowly. Symptoms often worsen over time and can limit your ability to do routine activities. Severe COPD may prevent you from doing even basic activities like walking, cooking, or taking care of yourself.
Most of the time, COPD is diagnosed in middle-aged or older adults. The disease isn't passed from person to person—you can't catch it from someone else.
COPD has no cure yet, and doctors don't know how to reverse the damage to the airways and lungs. However, treatments and lifestyle changes can help you feel better, stay more active, and slow the progress of the disease.
Long-term exposure to lung irritants that damage the lungs and the airways usually is the cause of COPD.
In the United States, the most common irritant that causes COPD is cigarette smoke. Pipe, cigar, and other types of tobacco smoke also can cause COPD, especially if the smoke is inhaled.
Breathing in secondhand smoke, air pollution, or chemical fumes or dust from the environment or workplace also can contribute to COPD. (Secondhand smoke is smoke in the air from other people smoking.)
Rarely, a genetic condition called alpha-1 antitrypsin deficiency may play a role in causing COPD. People who have this condition have low levels of alpha-1 antitrypsin (AAT)—a protein made in the liver.
Having a low level of the AAT protein can lead to lung damage and COPD if you're exposed to smoke or other lung irritants. If you have this condition and smoke, COPD can worsen very quickly.
Although uncommon, some people who have asthma can develop COPD. Asthma is a chronic (long-term) lung disease that inflames and narrows the airways. Treatment usually can reverse the inflammation and narrowing. However, if not, COPD can develop.
The main risk factor for COPD is smoking. Most people who have COPD smoke or used to smoke. People who have a family history of COPD are more likely to develop the disease if they smoke.
Long-term exposure to other lung irritants also is a risk factor for COPD. Examples of other lung irritants include secondhand smoke, air pollution, and chemical fumes and dust from the environment or workplace. (Secondhand smoke is smoke in the air from other people smoking.)
Most people who have COPD are at least 40 years old when symptoms begin. Although uncommon, people younger than 40 can have COPD. For example, this may happen if a person has alpha-1 antitrypsin deficiency, a genetic condition.
At first, COPD may cause no symptoms or only mild symptoms. As the disease gets worse, symptoms usually become more severe. Common signs and symptoms of COPD include:
If you have COPD, you also may have colds or the flu (influenza) often.
Not everyone who has the symptoms above has COPD. Likewise, not everyone who has COPD has these symptoms. Some of the symptoms of COPD are similar to the symptoms of other diseases and conditions. Your doctor can find out whether you have COPD.
If your symptoms are mild, you may not notice them, or you may adjust your lifestyle to make breathing easier. For example, you may take the elevator instead of the stairs.
Over time, symptoms may become severe enough to see a doctor. For example, you may get short of breath during physical exertion.
The severity of your symptoms will depend on how much lung damage you have. If you keep smoking, the damage will occur faster than if you stop smoking.
Severe COPD can cause other symptoms, such as swelling in your ankles, feet, or legs; weight loss; and lower muscle endurance.
Some severe symptoms may require treatment in a hospital. You—with the help of family members or friends, if you're unable—should seek emergency care if:
Your doctor will diagnose COPD based on your signs and symptoms, your medical and family histories, and test results.
Your doctor may ask whether you smoke or have had contact with lung irritants, such as secondhand smoke, air pollution, chemical fumes, or dust.
If you have an ongoing cough, let your doctor know how long you've had it, how much you cough, and how much mucus comes up when you cough. Also, let your doctor know whether you have a family history of COPD.
Your doctor will examine you and use a stethoscope to listen for wheezing or other abnormal chest sounds. He or she also may recommend one or more tests to diagnose COPD.
Lung function tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood.
The main test for COPD is spirometry (spi-ROM-eh-tre). Other lung function tests, such as a lung diffusion capacity test, also might be used. (For more information, go to the Health Topics Lung Function Tests article.)
During this painless test, a technician will ask you to take a deep breath in. Then, you'll blow as hard as you can into a tube connected to a small machine. The machine is called a spirometer.
The machine measures how much air you breathe out. It also measures how fast you can blow air out.
The image shows how spirometry is done. The patient takes a deep breath and then blows hard into a tube connected to a spirometer. The spirometer measures the amount of air breathed out. It also measures how fast the air is blown out.
Your doctor may have you inhale medicine that helps open your airways and then blow into the tube again. He or she can then compare your test results before and after taking the medicine.
Spirometry can detect COPD before symptoms develop. Your doctor also might use the test results to find out how severe your COPD is and to help set your treatment goals.
The test results also may help find out whether another condition, such as asthma or heart failure, is causing your symptoms.
Your doctor may recommend other tests, such as:
COPD has no cure yet. However, lifestyle changes and treatments can help you feel better, stay more active, and slow the progress of the disease.
The goals of COPD treatment include:
To assist with your treatment, your family doctor may advise you to see a pulmonologist. This is a doctor who specializes in treating lung disorders.
Quitting smoking is the most important step you can take to treat COPD. Talk with your doctor about programs and products that can help you quit.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking. Ask your family members and friends to support you in your efforts to quit.
Also, try to avoid secondhand smoke and places with dust, fumes, or other toxic substances that you may inhale.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's "Your Guide to a Healthy Heart." Although these resources focus on heart health, they include basic information about how to quit smoking.
If you have COPD, you may have trouble eating enough because of your symptoms, such as shortness of breath and fatigue. (This issue is more common with severe disease.)
As a result, you may not get all of the calories and nutrients you need, which can worsen your symptoms and raise your risk for infections.
Talk with your doctor about following an eating plan that will meet your nutritional needs. Your doctor may suggest eating smaller, more frequent meals; resting before eating; and taking vitamins or nutritional supplements.
Also, talk with your doctor about what types of activity are safe for you. You may find it hard to be active with your symptoms. However, physical activity can strengthen the muscles that help you breathe and improve your overall wellness.
Bronchodilators relax the muscles around your airways. This helps open your airways and makes breathing easier.
Depending on the severity of your COPD, your doctor may prescribe short-acting or long-acting bronchodilators. Short-acting bronchodilators last about 4–6 hours and should be used only when needed. Long-acting bronchodilators last about 12 hours or more and are used every day.
Most bronchodilators are taken using a device called an inhaler. This device allows the medicine to go straight to your lungs. Not all inhalers are used the same way. Ask your health care team to show you the correct way to use your inhaler.
If your COPD is mild, your doctor may only prescribe a short-acting inhaled bronchodilator. In this case, you may use the medicine only when symptoms occur.
If your COPD is moderate or severe, your doctor may prescribe regular treatment with short- and long-acting bronchodilators.
If your COPD is more severe, or if your symptoms flare up often, your doctor may prescribe a combination of medicines that includes a bronchodilator and an inhaled steroid. Steroids help reduce airway inflammation.
In general, using inhaled steroids alone is not a preferred treatment.
Your doctor may ask you to try inhaled steroids with the bronchodilator for a trial period of 6 weeks to 3 months to see whether the addition of the steroid helps relieve your breathing problems.
The flu (influenza) can cause serious problems for people who have COPD. Flu shots can reduce your risk of getting the flu. Talk with your doctor about getting a yearly flu shot.
This vaccine lowers your risk for pneumococcal pneumonia (NU-mo-KOK-al nu-MO-ne-ah) and its complications. People who have COPD are at higher risk for pneumonia than people who don't have COPD. Talk with your doctor about whether you should get this vaccine.
Pulmonary rehabilitation (rehab) is a broad program that helps improve the well-being of people who have chronic (ongoing) breathing problems.
Rehab may include an exercise program, disease management training, and nutritional and psychological counseling. The program's goal is to help you stay active and carry out your daily activities.
Your rehab team may include doctors, nurses, physical therapists, respiratory therapists, exercise specialists, and dietitians. These health professionals will create a program that meets your needs.
If you have severe COPD and low levels of oxygen in your blood, oxygen therapy can help you breathe better. For this treatment, you're given oxygen through nasal prongs or a mask.
You may need extra oxygen all the time or only at certain times. For some people who have severe COPD, using extra oxygen for most of the day can help them:
Surgery may benefit some people who have COPD. Surgery usually is a last resort for people who have severe symptoms that have not improved from taking medicines.
Surgeries for people who have COPD that's mainly related to emphysema include bullectomy (bul-EK-toe-me) and lung volume reduction surgery (LVRS). A lung transplant might be an option for people who have very severe COPD.
When the walls of the air sacs are destroyed, larger air spaces called bullae (BUL-e) form. These air spaces can become so large that they interfere with breathing. In a bullectomy, doctors remove one or more very large bullae from the lungs.
In LVRS, surgeons remove damaged tissue from the lungs. This helps the lungs work better. In carefully selected patients, LVRS can improve breathing and quality of life.
During a lung transplant, your damaged lung is removed and replaced with a healthy lung from a deceased donor.
A lung transplant can improve your lung function and quality of life. However, lung transplants have many risks, such as infections. The surgery can cause death if the body rejects the transplanted lung.
If you have very severe COPD, talk with your doctor about whether a lung transplant is an option. Ask your doctor about the benefits and risks of this type of surgery.
COPD symptoms usually worsen slowly over time. However, they can worsen suddenly. For instance, a cold, the flu, or a lung infection may cause your symptoms to quickly worsen. You may have a much harder time catching your breath. You also may have chest tightness, more coughing, changes in the color or amount of your sputum (spit), and a fever.
Call your doctor right away if your symptoms worsen suddenly. He or she may prescribe antibiotics to treat the infection and other medicines, such as bronchodilators and inhaled steroids, to help you breathe.
Some severe symptoms may require treatment in a hospital. For more information, go to "What Are the Signs and Symptoms of COPD?"
You can take steps to prevent COPD before it starts. If you already have COPD, you can take steps to prevent complications and slow the progress of the disease.
The best way to prevent COPD is to not start smoking or to quit smoking. Smoking is the leading cause of COPD. If you smoke, talk with your doctor about programs and products that can help you quit.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking. Ask your family members and friends to support you in your efforts to quit.
Also, try to avoid lung irritants that can contribute to COPD. Examples include secondhand smoke, air pollution, chemical fumes, and dust. (Secondhand smoke is smoke in the air from other people smoking.)
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's "Your Guide to a Healthy Heart." Although these resources focus on heart health, they include basic information about how to quit smoking.
If you have COPD, the most important step you can take is to quit smoking. Quitting can help prevent complications and slow the progress of the disease. You also should avoid exposure to the lung irritants mentioned above.
Follow your treatments for COPD exactly as your doctor prescribes. They can help you breathe easier, stay more active, and avoid or manage severe symptoms.
Talk with your doctor about whether and when you should get flu (influenza) and pneumonia vaccines. These vaccines can lower your chances of getting these illnesses, which are major health risks for people who have COPD.
COPD has no cure yet. However, you can take steps to manage your symptoms and slow the progress of the disease. You can:
If you smoke, quit. Smoking is the leading cause of COPD. Talk with your doctor about programs and products that can help you quit.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking. Ask your family members and friends to support you in your efforts to quit.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute's "Your Guide to a Healthy Heart." Although these resources focus on heart health, they include basic information about how to quit smoking.
Also, try to avoid lung irritants that can contribute to COPD. Examples include secondhand smoke, air pollution, chemical fumes, and dust. (Secondhand smoke is smoke in the air from other people smoking.)
Keep these irritants out of your home. If your home is painted or sprayed for insects, have it done when you can stay away for a while.
Keep your windows closed and stay at home (if possible) when there's a lot of air pollution or dust outside.
If you have COPD, it's important to get ongoing medical care. Take all of your medicines as your doctor prescribes. Make sure to refill your prescriptions before they run out. Bring a list of all the medicines you're taking when you have medical checkups.
Talk with your doctor about whether and when you should get flu (influenza) and pneumonia vaccines. Also, ask him or her about other diseases for which COPD may increase your risk, such as heart disease, lung cancer, and pneumonia.
You can do things to help manage COPD and its symptoms. For example:
Depending on how severe your disease is, you may want to ask your family and friends for help with daily tasks.
If you have COPD, know when and where to seek help for your symptoms. You should get emergency care if you have severe symptoms, such as trouble catching your breath or talking. (For more information on severe symptoms, go to "What Are the Signs and Symptoms of COPD?")
Call your doctor if you notice that your symptoms are worsening or if you have signs of an infection, such as a fever. Your doctor may change or adjust your treatments to relieve and treat symptoms.
Keep phone numbers handy for your doctor, hospital, and someone who can take you for medical care. You also should have on hand directions to the doctor's office and hospital and a list of all the medicines you're taking.
Living with COPD may cause fear, anxiety, depression, and stress. Talk about how you feel with your health care team. Talking to a professional counselor also might help. If you're very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to living with COPD. You can see how other people who have the same symptoms have coped with them. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has uncovered some of the causes of chronic lung diseases, as well as ways to prevent and treat these diseases.
Many more questions remain about chronic lung diseases, including COPD. The NHLBI continues to support research aimed at learning more about these diseases. For example, NHLBI-supported research on COPD includes studies that explore:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you may gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to COPD, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
A heart attack happens when the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can't get oxygen. If blood flow isn't restored quickly, the section of heart muscle begins to die.
Heart attacks are a leading killer of both men and women in the United States. The good news is that excellent treatments are available for heart attacks. These treatments can save lives and prevent disabilities.
Heart attack treatment works best when it's given right after symptoms occur. If you think you or someone else is having a heart attack (even if you're not fully sure), call9–1–1 right away.
Heart attacks most often occur as a result of coronary heart disease (CHD), also called coronary artery disease. CHD is a condition in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart.
When plaque builds up in the arteries, the condition is called atherosclerosis (ath-er-o-skler-O-sis). The buildup of plaque occurs over many years.
Eventually, an area of plaque can rupture (break open) inside of an artery. This causes a blood clot to form on the plaque's surface. If the clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn't treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
Figure A shows a heart with dead heart muscle caused by a heart attack. Figure B is a cross-section of a coronary artery with plaque buildup and a blood clot.
A less common cause of heart attack is a severe spasm (tightening) of a coronary artery. The spasm cuts off blood flow through the artery. Spasms can occur in coronary arteries that aren't affected by atherosclerosis.
Heart attacks can be associated with or lead to severe health problems, such as heart failure and life-threatening arrhythmias (ah-RITH-me-ahs).
Heart failure is a condition in which the heart can't pump enough blood to meet the body's needs. Arrhythmias are irregular heartbeats. Ventricular fibrillation is a life-threatening arrhythmia that can cause death if not treated right away.
Acting fast at the first sign of heart attack symptoms can save your life and limit damage to your heart. Treatment works best when it's given right after symptoms occur.
Many people aren't sure what's wrong when they are having symptoms of a heart attack. Some of the most common warning symptoms of a heart attack for both men and women are:
Other possible symptoms of a heart attack include:
Not all heart attacks begin with the sudden, crushing chest pain that often is shown on TV or in the movies, or other common symptoms such as chest discomfort. The symptoms of a heart attack can vary from person to person. Some people can have few symptoms and are surprised to learn they've had a heart attack. If you've already had a heart attack, your symptoms may not be the same for another one.
Quick Action Can Save Your Life: Call 9–1–1
If you think you or someone else may be having heart attack symptoms or a heart attack, don't ignore it or feel embarrassed to call for help. Call 9–1–1 for emergency medical care. Acting fast can save your life.
Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
Each year, close to 1 million people in the United States have heart attacks, and many of them die. CHD, which often results in heart attacks, is the leading killer of both men and women in the United States.
Many more people could survive or recover better from heart attacks if they got help faster. Of the people who die from heart attacks, about half die within an hour of the first symptoms and before they reach the hospital.
A heart attack happens if the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can't get oxygen. Most heart attacks occur as a result of coronary heart disease (CHD).
CHD is a condition in which a waxy substance called plaque builds up inside of the coronary arteries. These arteries supply oxygen-rich blood to your heart.
When plaque builds up in the arteries, the condition is called atherosclerosis. The buildup of plaque occurs over many years.
Eventually, an area of plaque can rupture (break open) inside of an artery. This causes a blood clot to form on the plaque's surface. If the clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn't treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
A less common cause of heart attack is a severe spasm (tightening) of a coronary artery. The spasm cuts off blood flow through the artery. Spasms can occur in coronary arteries that aren't affected by atherosclerosis.
What causes a coronary artery to spasm isn't always clear. A spasm may be related to:
The animation below shows how plaque buildup or a coronary artery spasm can lead to a heart attack. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
Certain risk factors make it more likely that you'll develop coronary heart disease (CHD) and have a heart attack. You can control many of these risk factors.
The major risk factors for a heart attack that you can control include:
Some of these risk factors—such as obesity, high blood pressure, and high blood sugar—tend to occur together. When they do, it's called metabolic syndrome.
In general, a person who has metabolic syndrome is twice as likely to develop heart disease and five times as likely to develop diabetes as someone who doesn't have metabolic syndrome.
For more information about the risk factors that are part of metabolic syndrome, go to the Health Topics Metabolic Syndrome article.
Risk factors that you can't control include:
Not all heart attacks begin with the sudden, crushing chest pain that often is shown on TV or in the movies. In one study, for example, one-third of the patients who had heart attacks had no chest pain. These patients were more likely to be older, female, or diabetic.
The symptoms of a heart attack can vary from person to person. Some people can have few symptoms and are surprised to learn they've had a heart attack. If you've already had a heart attack, your symptoms may not be the same for another one. It is important for you to know the most common symptoms of a heart attack and also remember these facts:
Some people don't have symptoms at all. Heart attacks that occur without any symptoms or with very mild symptoms are called silent heart attacks.
The most common warning symptoms of a heart attack for both men and women are:
The symptoms of angina (an-JI-nuh or AN-juh-nuh) can be similar to the symptoms of a heart attack. Angina is chest pain that occurs in people who have coronary heart disease, usually when they're active. Angina pain usually lasts for only a few minutes and goes away with rest.
Chest pain or discomfort that doesn't go away or changes from its usual pattern (for example, occurs more often or while you're resting) can be a sign of a heart attack.
All chest pain should be checked by a doctor.
Pay attention to these other possible symptoms of a heart attack:
Not everyone having a heart attack has typical symptoms. If you've already had a heart attack, your symptoms may not be the same for another one. However, some people may have a pattern of symptoms that recur.
The more signs and symptoms you have, the more likely it is that you're having a heart attack.
The signs and symptoms of a heart attack can develop suddenly. However, they also can develop slowly—sometimes within hours, days, or weeks of a heart attack.
Any time you think you might be having heart attack symptoms or a heart attack, don't ignore it or feel embarrassed to call for help. Call 9–1–1 for emergency medical care, even if you are not sure whether you're having a heart attack. Here's why:
Every minute matters. Never delay calling 9–1–1 to take aspirin or do anything else you think might help.
Your doctor will diagnose a heart attack based on your signs and symptoms, your medical and family histories, and test results.
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can show signs of heart damage due to coronary heart disease (CHD) and signs of a previous or current heart attack.
During a heart attack, heart muscle cells die and release proteins into the bloodstream. Blood tests can measure the amount of these proteins in the bloodstream. Higher than normal levels of these proteins suggest a heart attack.
Commonly used blood tests include troponin tests, CK or CK–MB tests, and serum myoglobin tests. Blood tests often are repeated to check for changes over time.
Coronary angiography (an-jee-OG-ra-fee) is a test that uses dye and special x rays to show the insides of your coronary arteries. This test often is done during a heart attack to help find blockages in the coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-e-ter-ih-ZA-shun).
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through the coronary arteries. The dye lets your doctor study the flow of blood through the heart and blood vessels.
If your doctor finds a blockage, he or she may recommend a procedure calledpercutaneous (per-ku-TA-ne-us) coronary intervention (PCI), sometimes referred to as coronary angioplasty (AN-jee-oh-plas-tee). This procedure can help restore blood flow through a blocked artery. Sometimes a small mesh tube called a stent is placed in the artery to help prevent blockages after the procedure.
Early treatment for a heart attack can prevent or limit damage to the heart muscle. Acting fast, at the first symptoms of a heart attack, can save your life. Medical personnel can begin diagnosis and treatment even before you get to the hospital.
Certain treatments usually are started right away if a heart attack is suspected, even before the diagnosis is confirmed. These include:
Once the diagnosis of a heart attack is confirmed or strongly suspected, doctors start treatments to try to promptly restore blood flow to the heart. The two main treatments are "clot-busting" medicines and percutaneous coronary intervention (PCI), sometimes referred to as coronary angioplasty, a procedure used to open blocked coronary arteries.
Clot-Busting Medicines
Thrombolytic medicines, also called "clot busters," are used to dissolve blood clots that are blocking the coronary arteries. To work best, these medicines must be given within several hours of the start of heart attack symptoms. Ideally, the medicine should be given as soon as possible.
Percutaneous Coronary Intervention
Percutaneous (per-ku-TA-ne-us) coronary intervention (PCI) is a nonsurgical procedure that opens blocked or narrowed coronary arteries. This procedure also is called coronary angioplasty.
A thin, flexible tube with a balloon or other device on the end is threaded through a blood vessel, usually in the groin (upper thigh), to the narrowed or blocked coronary artery.
Once in place, the balloon is inflated to compress the plaque against the wall of the artery. This restores blood flow through the artery.
During the procedure, the doctor may put a small mesh tube called a stent in the artery. The stent helps prevent blockages in the artery in the months or years after the procedure.
For more information, go to the Health Topics PCI article.
Other Treatments for Heart Attack
Medicines
You also may be given medicines to relieve pain and anxiety, treat arrhythmias (which often occur during a heart attack), or lower your cholesterol (these medicines are called statins).
Medical Procedures
Coronary artery bypass grafting (CABG) also may be used to treat a heart attack. During CABG, a surgeon removes a healthy artery or vein from your body. The artery or vein is then connected, or grafted, to the blocked coronary artery.
The grafted artery or vein bypasses (that is, goes around) the blocked portion of the coronary artery. This provides a new route for blood to flow to the heart muscle.
For more information, go to the Health Topics Coronary Artery Bypass Graftingarticle.
Treatment After You Leave the Hospital
Most people spend several days in the hospital after a heart attack. When you leave the hospital, treatment doesn't stop. At home, your treatment may include daily medicines and cardiac rehabilitation (rehab). Your doctor may want you to have a flu shot and pneumococcal vaccine each year.
Your doctor also may recommend lifestyle changes, including following a heart healthy diet, being physically active, maintaining a healthy weight, and quitting smoking. Taking these steps can lower your chances of having another heart attack.
Cardiac Rehabilitation
Your doctor may recommend cardiac rehab to help you recover from a heart attack and to help prevent another heart attack. Almost everyone who has had a heart attack can benefit from rehab.
Cardiac rehab is a medically supervised program that may help improve the health and well-being of people who have heart problems.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians or nutritionists, and psychologists or other mental health specialists.
Rehab has two parts:
Lowering your risk factors for coronary heart disease (CHD) can help you prevent a heart attack. (For more information about risk factors, go to "Who Is at Risk for a Heart Attack?")
Even if you already have CHD, you can still take steps to lower your risk for a heart attack. These steps involve following a heart healthy lifestyle and getting ongoing care.
Following a healthy diet is an important part of a heart healthy lifestyle. A healthy diet includes a variety of fruits, vegetables, and whole grains. It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugars.
For more information about following a healthy diet, go to the National Heart, Lung, and Blood Institute's (NHLBI's) Aim for a Healthy Weight Web site, "Your Guide to a Healthy Heart," and "Your Guide to Lowering Your Blood Pressure With DASH." All of these resources provide general information about healthy eating.
If you're overweight or obese, work with your doctor to create a reasonable weight-loss plan that involves diet and physical activity. Controlling your weight helps you control risk factors for CHD and heart attack.
Be as physically active as you can. Physical activity can improve your fitness level and your health. Talk with your doctor about what types of activity are safe for you.
For more information about physical activity, go to the Health Topics Physical Activity and Your Heart article and the NHLBI's "Your Guide to Physical Activity and Your Heart."
If you smoke, quit. Smoking can raise your risk of CHD and heart attack. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke. For more information about quitting smoking, go to the Health Topics Smoking and Your Heart article.
Treating conditions that make a heart attack more likely also can help lower your risk for a heart attack. These conditions may include:
Make sure that you have an emergency action plan in case you or someone in your family has a heart attack. This is very important if you're at high risk for a heart attack or have already had a heart attack.
Write down a list of medicines you are taking, medicines you are allergic to, your health care provider's phone numbers (both during and after office hours), and contact information for a friend or relative. Keep the list in a handy place to share in a medical emergency (for example, fill out this wallet card).
Talk with your doctor about the signs and symptoms of a heart attack, when you should call 9–1–1, and steps you can take while waiting for medical help to arrive.
Many people survive heart attacks and live active, full lives. If you get help quickly, treatment can limit damage to your heart muscle. Less heart damage improves your chances for a better quality of life after a heart attack.
After a heart attack, you'll need treatment for coronary heart disease (CHD). This will help prevent another heart attack. Your doctor may recommend:
If you find it hard to get your medicines or take them, talk with your doctor. Don't stop taking medicines that can help you prevent another heart attack.
After a heart attack, most people who don't have chest pain or discomfort or other problems can safely return to most of their normal activities within a few weeks. Most can begin walking right away.
Sexual activity also can begin within a few weeks for most patients. Talk with your doctor about a safe schedule for returning to your normal routine.
If allowed by State law, driving usually can begin within a week for most patients who don't have chest pain or discomfort or other problems. Each State has rules about driving a motor vehicle following a serious illness. People who have complications shouldn't drive until their symptoms have been stable for a few weeks.
After a heart attack, many people worry about having another heart attack. Sometimes they feel depressed and have trouble adjusting to new lifestyle changes.
Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you're very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to life after a heart attack. You can see how other people who have the same symptoms have coped with them. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Once you've had a heart attack, you're at higher risk for another one. Knowing the difference between angina and a heart attack is important. Angina is chest pain that occurs in people who have CHD.
The pain from angina usually occurs after physical exertion and goes away in a few minutes when you rest or take medicine as directed.
The pain from a heart attack usually is more severe than the pain from angina. Heart attack pain doesn't go away when you rest or take medicine.
If you don't know whether your chest pain is angina or a heart attack, call 9–1–1.
The symptoms of a second heart attack may not be the same as those of a first heart attack. Don't take a chance if you're in doubt. Always call 9–1–1 right away if you or someone else has heart attack symptoms.
Unfortunately, most heart attack victims wait 2 hours or more after their symptoms start before they seek medical help. This delay can result in lasting heart damage or death.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has uncovered some of the causes of heart diseases and conditions, as well as ways to prevent or treat them.
Many more questions remain about heart diseases and conditions, including heart attacks. The NHLBI continues to support research aimed at learning more about heart attacks. For example, NHLBI-supported research includes studies that explore:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart attacks, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
Source: NHLBI, NIH
Sudden cardiac arrest (SCA) is a condition in which the heart suddenly and unexpectedly stops beating. If this happens, blood stops flowing to the brain and other vital organs.
SCA usually causes death if it's not treated within minutes.
To understand SCA, it helps to understand how the heart works. The heart has an electrical system that controls the rate and rhythm of the heartbeat. Problems with the heart's electrical system can cause irregular heartbeats called arrhythmias.
There are many types of arrhythmias. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. Some arrhythmias can cause the heart to stop pumping blood to the body—these arrhythmias cause SCA.
SCA is not the same as a heart attack. A heart attack occurs if blood flow to part of the heart muscle is blocked. During a heart attack, the heart usually doesn't suddenly stop beating. SCA, however, may happen after or during recovery from a heart attack.
People who have heart disease are at higher risk for SCA. However, SCA can happen in people who appear healthy and have no known heart disease or other risk factors for SCA.
Most people who have SCA die from it—often within minutes. Rapid treatment of SCA with a defibrillator can be lifesaving. A defibrillator is a device that sends an electric shock to the heart to try to restore its normal rhythm.
Automated external defibrillators (AEDs) can be used by bystanders to save the lives of people who are having SCA. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
Ventricular fibrillation (v-fib) causes most sudden cardiac arrests (SCAs). V-fib is a type of arrhythmia.
During v-fib, the ventricles (the heart's lower chambers) don't beat normally. Instead, they quiver very rapidly and irregularly. When this happens, the heart pumps little or no blood to the body. V-fib is fatal if not treated within a few minutes.
Other problems with the heart's electrical system also can cause SCA. For example, SCA can occur if the rate of the heart's electrical signals becomes very slow and stops. SCA also can occur if the heart muscle doesn't respond to the heart's electrical signals.
Certain diseases and conditions can cause the electrical problems that lead to SCA. Examples include coronary heart disease(CHD), also called coronary artery disease; severe physical stress; certain inherited disorders; and structural changes in the heart.
Several research studies are under way to try to find the exact causes of SCA and how to prevent them.
CHD is a disease in which a waxy substance called plaque (plak) builds up in the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
Plaque narrows the arteries and reduces blood flow to your heart muscle. Eventually, an area of plaque can rupture (break open). This may cause a blood clot to form on the plaque's surface.
A blood clot can partly or fully block the flow of oxygen-rich blood to the portion of heart muscle fed by the artery. This causes a heart attack.
During a heart attack, some heart muscle cells die and are replaced with scar tissue. The scar tissue damages the heart's electrical system. As a result, electrical signals may spread abnormally throughout the heart. These changes to the heart increase the risk of dangerous arrhythmias and SCA.
CHD seems to cause most cases of SCA in adults. Many of these adults, however, have no signs or symptoms of CHD before having SCA.
Certain types of physical stress can cause your heart's electrical system to fail. Examples include:
A tendency to have arrhythmias runs in some families. This tendency is inherited, which means it's passed from parents to children through the genes. Members of these families may be at higher risk for SCA.
An example of an inherited disorder that makes you more likely to have arrhythmias is long QT syndrome (LQTS). LQTS is a disorder of the heart's electrical activity. Problems with tiny pores on the surface of heart muscle cells cause the disorder. LQTS can cause sudden, uncontrollable, dangerous heart rhythms.
People who inherit structural heart problems also may be at higher risk for SCA. These types of problems often are the cause of SCA in children.
Changes in the heart's normal size or structure may affect its electrical system. Examples of such changes include an enlarged heart due to high blood pressure or advanced heart disease. Heart infections also may cause structural changes in the heart.
The risk of sudden cardiac arrest (SCA) increases:
The major risk factor for SCA is coronary heart disease. Most people who have SCA have some degree of coronary heart disease; however, many people may not know that they have coronary heart disease until SCA occurs. Usually their coronary heart disease is “silent”—that is, it has no signs or symptoms. Because of this, doctors and nurses have not detected it.
Many people who have SCA also have silent, or undiagnosed, heart attacks before sudden cardiac arrest happens. These people have no clear signs of heart attack, and they don’t even realize that they’ve had one. Read more about coronary heart disease risk factors.
Other risk factors for SCA include:
Usually, the first sign of sudden cardiac arrest (SCA) is loss of consciousness (fainting). At the same time, no heartbeat (or pulse) can be felt.
Some people may have a racing heartbeat or feel dizzy or light-headed just before they faint. Within an hour before SCA, some people have chest pain, shortness of breath, nausea (feeling sick to the stomach), or vomiting.
Sudden cardiac arrest (SCA) happens without warning and requires emergency treatment. Doctors rarely diagnose SCA with medical tests as it's happening. Instead, SCA often is diagnosed after it happens. Doctors do this by ruling out other causes of a person's sudden collapse.
If you're at high risk for SCA, your doctor may refer you to a cardiologist. This is a doctor who specializes in diagnosing and treating heart diseases and conditions. Your cardiologist will work with you to decide whether you need treatment to prevent SCA.
Some cardiologists specialize in problems with the heart's electrical system. These specialists are called cardiac electrophysiologists.
Doctors use several tests to help detect the factors that put people at risk for SCA.
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can show evidence of heart damage due to coronary heart disease (CHD). The test also can show signs of a previous or current heart attack.
Echocardiography, or echo, is a painless test that uses sound waves to create pictures of your heart. The test shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
There are several types of echo, including stress echo. This test is done both before and after a cardiac stress test. During this test, you exercise (or are given medicine if you're unable to exercise) to make your heart work hard and beat fast.
Stress echo shows whether you have decreased blood flow to your heart (a sign of CHD).
A MUGA (multiple gated acquisition) test shows how well your heart is pumping blood. For this test, a small amount of radioactive substance is injected into a vein and travels to your heart.
The substance releases energy, which special cameras outside of your body can detect. The cameras use the energy to create pictures of many parts of your heart.
Cardiac MRI (magnetic resonance imaging) is a safe procedure that uses radio waves and magnets to create detailed pictures of your heart. The test creates still and moving pictures of your heart and major blood vessels.
Doctors use cardiac MRI to get pictures of the beating heart and to look at the structure and function of the heart.
Cardiac catheterization is a procedure used to diagnose and treat certain heart conditions. A long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. Through the catheter, your doctor can do diagnostic tests and treatments on your heart.
Sometimes dye is put into the catheter. The dye will flow through your bloodstream to your heart. The dye makes your coronary (heart) arteries visible on x-ray pictures. The dye can show whether plaque has narrowed or blocked any of your coronary arteries.
For an electrophysiology study, doctors use cardiac catheterization to record how your heart's electrical system responds to certain medicines and electrical stimulation. This helps your doctor find where the heart's electrical system is damaged.
Your doctor may recommend blood tests to check the levels of potassium, magnesium, and other chemicals in your blood. These chemicals play an important role in your heart's electrical signaling.
Sudden cardiac arrest (SCA) is an emergency. A person having SCA needs to be treated with a defibrillator right away. This device sends an electric shock to the heart. The electric shock can restore a normal rhythm to a heart that's stopped beating.
To work well, defibrillation must be done within minutes of SCA. With every minute that passes, the chances of surviving SCA drop rapidly.
Police, emergency medical technicians, and other first responders usually are trained and equipped to use a defibrillator. Call 9–1–1 right away if someone has signs or symptoms of SCA. The sooner you call for help, the sooner lifesaving treatment can begin.
Automated external defibrillators (AEDs) are special defibrillators that untrained bystanders can use. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
AEDs are programmed to give an electric shock if they detect a dangerous arrhythmia, such as ventricular fibrillation. This prevents giving a shock to someone who may have fainted but isn't having SCA.
You should give cardiopulmonary resuscitation (CPR) to a person having SCA until defibrillation can be done.
People who are at risk for SCA may want to consider having an AED at home. A 2008 study by the National Heart, Lung, and Blood Institute and the National Institutes of Health found that AEDs in the home are safe and effective.
Some people feel that placing these devices in homes will save many lives because many SCAs occur at home. Others note that no evidence supports the idea that home-use AEDs save more lives. These people fear that people who have AEDs in their homes will delay calling for help during an emergency. They're also concerned that people who have home-use AEDs will not properly maintain the devices or forget where they are.
When considering a home-use AED, talk with your doctor. He or she can help you decide whether having an AED in your home will benefit you.
If you survive SCA, you'll likely be admitted to a hospital for ongoing care and treatment. In the hospital, your medical team will closely watch your heart. They may give you medicines to try to reduce the risk of another SCA.
While in the hospital, your medical team will try to find out what caused your SCA. If you're diagnosed with coronary heart disease, you may have percutaneous coronary intervention, also known as coronary angioplasty, or coronary artery bypass grafting. These procedures help restore blood flow through narrowed or blocked coronary arteries.
Often, people who have SCA get a device called an implantable cardioverter defibrillator (ICD). This small device is surgically placed under the skin in your chest or abdomen. An ICD uses electric pulses or shocks to help control dangerous arrhythmias. (For more information, go to "How Can Death Due to Sudden Cardiac Arrest Be Prevented?")
Ways to prevent death due to sudden cardiac arrest (SCA) differ depending on whether:
If you've already had SCA, you're at high risk of having it again. Research shows that an implantable cardioverter defibrillator (ICD) reduces the chances of dying from a second SCA. An ICD is surgically placed under the skin in your chest or abdomen. The device has wires with electrodes on the ends that connect to your heart's chambers. The ICD monitors your heartbeat.
If the ICD detects a dangerous heart rhythm, it gives an electric shock to restore the heart's normal rhythm. Your doctor may give you medicine to limit irregular heartbeats that can trigger the ICD.
An ICD isn't the same as a pacemaker. The devices are similar, but they have some differences. Pacemakers give off low-energy electrical pulses. They're often used to treat less dangerous heart rhythms, such as those that occur in the upper chambers of the heart. Most new ICDs work as both pacemakers and ICDs.
If you have severe coronary heart disease (CHD), you're at increased risk for SCA. This is especially true if you've recently had a heart attack.
Your doctor may prescribe a type of medicine called a beta blocker to help lower your risk for SCA. Your doctor also may discuss beginning statin treatment if you have an elevated risk for developing heart disease or having a stroke. Doctors usually prescribe statins for people who have:
Your doctor also may prescribe other medications to:
Take all medicines regularly, as your doctor prescribes. Don’t change the amount of your medicine or skip a dose unless your doctor tells you to. You should still follow a heart-healthy lifestyle, even if you take medicines to treat your coronary heart disease.
Other treatments for coronary heart disease—such as percutaneous coronary intervention, also known as coronary angioplasty, or coronary artery bypass grafting—also may lower your risk for SCA. Your doctor also may recommend an ICD if you’re at high risk for SCA.
CHD seems to be the cause of most SCAs in adults. CHD also is a major risk factor for angina (chest pain or discomfort) and heart attack, and it contributes to other heart problems.
Following a healthy lifestyle can help you lower your risk for CHD, SCA, and other heart problems. A heart-healthy lifestyle includes:
Heart-healthy eating is an important part of a heart-healthy lifestyle. Your doctor may recommend heart-healthy eating, which should include:
When following a heart-healthy diet, you should avoid eating:
Two nutrients in your diet make blood cholesterol levels rise:
Saturated fat raises your blood cholesterol more than anything else in your diet. When you follow a heart-healthy eating plan, only 5 percent to 6 percent of your daily calories should come from saturated fat. Food labels list the amounts of saturated fat. To help you stay on track, here are some examples:
|
If you eat: |
Try to eat no more than: |
|
1,200 calories a day |
8 grams of saturated fat a day |
|
1,500 calories a day |
10 grams of saturated fat a day |
|
1,800 calories a day |
12 grams of saturated fat a day |
|
2,000 calories a day |
13 grams of saturated fat a day |
|
2,500 calories a day |
17 grams of saturated fat a day |
Not all fats are bad. Monounsaturated and polyunsaturated fats actually help lower blood cholesterol levels. Some sources of monounsaturated and polyunsaturated fats are:
You should try to limit the amount of sodium that you eat. This means choosing and preparing foods that are lower in salt and sodium. Try to use low-sodium and “no added salt” foods and seasonings at the table or while cooking. Food labels tell you what you need to know about choosing foods that are lower in sodium. Try to eat no more than 2,300 milligrams of sodium a day. If you have high blood pressure, you may need to restrict your sodium intake even more.
Your doctor may recommend the Dietary Approaches to Stop Hypertension (DASH) eating plan if you have high blood pressure. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart healthy and low in fat, cholesterol, and sodium and salt.
The DASH eating plan is a good heart-healthy eating plan, even for those who don’t have high blood pressure. Read more about DASH.
Try to limit alcohol intake. Too much alcohol can raise your blood pressure and triglyceride levels, a type of fat found in the blood. Alcohol also adds extra calories, which may cause weight gain.
Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. One drink is:
Maintaining a healthy weight is important for overall health and can lower your risk for sudden cardiac arrest. Aim for a Healthy Weight by following a heart-healthy eating plan and keeping physically active.
Knowing your body mass index (BMI) helps you find out if you’re a healthy weight in relation to your height and gives an estimate of your total body fat. To figure out your BMI, check out the National Heart, Lung, and Blood Institute’s online BMI calculator or talk to your doctor. A BMI:
A general goal to aim for is a BMI of less than 25. Your doctor or health care provider can help you set an appropriate BMI goal.
Measuring waist circumference helps screen for possible health risks. If most of your fat is around your waist rather than at your hips, you’re at a higher risk for heart disease and type 2 diabetes. This risk may be higher with a waist size that is greater than 35 inches for women or greater than 40 inches for men. To learn how to measure your waist, visit Assessing Your Weight and Health Risk.
If you’re overweight or obese, try to lose weight. A loss of just 3 percent to 5 percent of your current weight can lower your triglycerides, blood glucose, and the risk of developing type 2 diabetes. Greater amounts of weight loss can improve blood pressure readings, lower LDL cholesterol, and increase HDL cholesterol.
Managing and coping with stress. Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Consider healthy stress-reducing activities, such as:
Regular physical activity can lower your risk for coronary heart disease, sudden cardiac arrest, and other health problems. Everyone should try to participate in moderate-intensity aerobic exercise at least 2 hours and 30 minutes per week or vigorous aerobic exercise for 1 hour and 15 minutes per week. Aerobic exercise, such as brisk walking, is any exercise in which your heart beats faster and you use more oxygen than usual. The more active you are, the more you will benefit. Participate in aerobic exercise for at least 10 minutes at a time spread throughout the week.
Talk with your doctor before you start a new exercise plan. Ask your doctor how much and what kinds of physical activity are safe for you.
Read more about physical activity at:
People who smoke are more likely to have a heart attack than are people who don’t smoke. The risk of having a heart attack increases with the number of cigarettes smoked each day. Smoking also raises your risk for stroke and lung diseases, such as chronic obstructive pulmonary disease (COPD) and lung cancer.
Quitting smoking can greatly reduce your risk for heart and lung diseases. Ask your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke. If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking. Read more about how to quit smoking.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. Often, these advances depend on the willingness of volunteers to take part in clinical trials.
Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions. For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to sudden cardiac arrest, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Sudden Cardiac Arrest Clinical Trials
Learn more about other sudden cardiac arrest trials and how to participate in a clinical trial.
Source: NHLBI, NIH
Heart failure is a condition in which the heart can't pump enough blood to meet the body's needs. In some cases, the heart can't fill with enough blood. In other cases, the heart can't pump blood to the rest of the body with enough force. Some people have both problems.
The term "heart failure" doesn't mean that your heart has stopped or is about to stop working. However, heart failure is a serious condition that requires medical care.
Heart failure develops over time as the heart's pumping action grows weaker. The condition can affect the right side of the heart only, or it can affect both sides of the heart. Most cases involve both sides of the heart.
Right-side heart failure occurs if the heart can't pump enough blood to the lungs to pick up oxygen. Left-side heart failure occurs if the heart can't pump enough oxygen-rich blood to the rest of the body.
Right-side heart failure may cause fluid to build up in the feet, ankles, legs, liver, abdomen, and the veins in the neck. Right-side and left-side heart failure also may cause shortness of breath and fatigue (tiredness).
The leading causes of heart failure are diseases that damage the heart. Examples include coronary heart disease (CHD), high blood pressure, and diabetes.
Heart failure is a very common condition. About 5.1 million people in the United States have heart failure.
Both children and adults can have the condition, although the symptoms and treatments differ. This article focuses on heart failure in adults.
Currently, heart failure has no cure. However, treatments—such as medicines and lifestyle changes—can help people who have the condition live longer and more active lives. Researchers continue to study new ways to treat heart failure and its complications.
Conditions that damage or overwork the heart muscle can cause heart failure. Over time, the heart weakens. It isn't able to fill with and/or pump blood as well as it should.
As the heart weakens, certain proteins and substances might be released into the blood. These substances have a toxic effect on the heart and blood flow, and they worsen heart failure.
The most common causes of heart failure are coronary heart disease (CHD), high blood pressure, and diabetes. Treating these problems can prevent or improve heart failure.
CHD is a condition in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
Plaque narrows the arteries and reduces blood flow to your heart muscle. The buildup of plaque also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow.
CHD can lead to chest pain or discomfort called angina (an-JI-nuh or AN-juh-nuh), a heart attack, heart damage, or even death.
Blood pressure is the force of blood pushing against the walls of the arteries. If this pressure rises and stays high over time, it can weaken your heart and lead to plaque buildup.
Blood pressure is considered high if it stays at or above 140/90 mmHg over time. (The mmHg is millimeters of mercury—the units used to measure blood pressure.) If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher.
Diabetes is a disease in which the body's blood glucose (sugar) level is too high. The body normally breaks down food into glucose and then carries it to cells throughout the body. The cells use a hormone called insulin to turn the glucose into energy.
In diabetes, the body doesn't make enough insulin or doesn't use its insulin properly. Over time, high blood sugar levels can damage and weaken the heart muscle and the blood vessels around the heart, leading to heart failure.
Other diseases and conditions also can lead to heart failure, such as:
Other factors also can injure the heart muscle and lead to heart failure. Examples include:
Heart damage from obstructive sleep apnea may worsen heart failure. Sleep apnea is a common disorder in which you have one or more pauses in breathing or shallow breaths while you sleep.
Sleep apnea can deprive your heart of oxygen and increase its workload. Treating this sleep disorder might improve heart failure.
About 5.8 million people in the United States have heart failure. The number of people who have this condition is growing.
Heart failure is more common in:
Children who have congenital heart defects also can develop heart failure. These defects occur if the heart, heart valves, or blood vessels near the heart don't form correctly while a baby is in the womb.
Congenital heart defects can make the heart work harder. This weakens the heart muscle, which can lead to heart failure.
Children don't have the same symptoms of heart failure or get the same treatments as adults. This article focuses on heart failure in adults.
The most common signs and symptoms of heart failure are:
All of these symptoms are the result of fluid buildup in your body. When symptoms start, you may feel tired and short of breath after routine physical effort, like climbing stairs.
As your heart grows weaker, symptoms get worse. You may begin to feel tired and short of breath after getting dressed or walking across the room. Some people have shortness of breath while lying flat.
Fluid buildup from heart failure also causes weight gain, frequent urination, and a cough that's worse at night and when you're lying down. This cough may be a sign of acute pulmonary edema (e-DE-ma). This is a condition in which too much fluid builds up in your lungs. The condition requires emergency treatment.
The image shows the major signs and symptoms of heart failure.
Your doctor will diagnose heart failure based on your medical and family histories, a physical exam, and test results. The signs and symptoms of heart failure also are common in other conditions. Thus, your doctor will:
Early diagnosis and treatment can help people who have heart failure live longer, more active lives.
Your doctor will ask whether you or others in your family have or have had a disease or condition that can cause heart failure.
Your doctor also will ask about your symptoms. He or she will want to know which symptoms you have, when they occur, how long you've had them, and how severe they are. Your answers will help show whether and how much your symptoms limit your daily routine.
During the physical exam, your doctor will:
No single test can diagnose heart failure. If you have signs and symptoms of heart failure, your doctor may recommend one or more tests.
Your doctor also may refer you to a cardiologist. A cardiologist is a doctor who specializes in diagnosing and treating heart diseases and conditions.
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast your heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through your heart.
An EKG may show whether the walls in your heart's pumping chambers are thicker than normal. Thicker walls can make it harder for your heart to pump blood. An EKG also can show signs of a previous or current heart attack.
A chest x ray takes pictures of the structures inside your chest, such as your heart, lungs, and blood vessels. This test can show whether your heart is enlarged, you have fluid in your lungs, or you have lung disease.
This test checks the level of a hormone in your blood called BNP. The level of this hormone rises during heart failure.
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test shows the size and shape of your heart and how well your heart chambers and valves work.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and heart muscle damage caused by lack of blood flow.
Echo might be done before and after a stress test (see below). A stress echo can show how well blood is flowing through your heart. The test also can show how well your heart pumps blood when it beats.
A Doppler ultrasound uses sound waves to measure the speed and direction of blood flow. This test often is done with echo to give a more complete picture of blood flow to the heart and lungs.
Doctors often use Doppler ultrasound to help diagnose right-side heart failure.
A Holter monitor records your heart's electrical activity for a full 24- or 48-hour period, while you go about your normal daily routine.
You wear small patches called electrodes on your chest. Wires connect the patches to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
A nuclear heart scan shows how well blood is flowing through your heart and how much blood is reaching your heart muscle.
During a nuclear heart scan, a safe, radioactive substance called a tracer is injected into your bloodstream through a vein. The tracer travels to your heart and releases energy. Special cameras outside of your body detect the energy and use it to create pictures of your heart.
A nuclear heart scan can show where the heart muscle is healthy and where it's damaged.
A positron emission tomography (PET) scan is a type of nuclear heart scan. It shows the level of chemical activity in areas of your heart. This test can help your doctor see whether enough blood is flowing to these areas. A PET scan can show blood flow problems that other tests might not detect.
During cardiac catheterization (KATH-eh-ter-ih-ZA-shun), a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. This allows your doctor to look inside your coronary (heart) arteries.
During this procedure, your doctor can check the pressure and blood flow in your heart chambers, collect blood samples, and use x rays to look at your coronary arteries.
Coronary angiography (an-jee-OG-rah-fee) usually is done with cardiac catheterization. A dye that can be seen on x ray is injected into your bloodstream through the tip of the catheter.
The dye allows your doctor to see the flow of blood to your heart muscle. Angiography also shows how well your heart is pumping.
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise to make your heart work hard and beat fast.
You may walk or run on a treadmill or pedal a bicycle. If you can't exercise, you may be given medicine to raise your heart rate.
Heart tests, such as nuclear heart scanning and echo, often are done during stress testing.
Cardiac MRI (magnetic resonance imaging) uses radio waves, magnets, and a computer to create pictures of your heart as it's beating. The test produces both still and moving pictures of your heart and major blood vessels.
A cardiac MRI can show whether parts of your heart are damaged. Doctors also have used MRI in research studies to find early signs of heart failure, even before symptoms appear.
Thyroid function tests show how well your thyroid gland is working. These tests include blood tests, imaging tests, and tests to stimulate the thyroid. Having too much or too little thyroid hormone in the blood can lead to heart failure.
Early diagnosis and treatment can help people who have heart failure live longer, more active lives. Treatment for heart failure will depend on the type and stage of heart failure (the severity of the condition).
The goals of treatment for all stages of heart failure include:
Treatments usually include lifestyle changes, medicines, and ongoing care. If you have severe heart failure, you also may need medical procedures or surgery.
Simple changes can help you feel better and control heart failure. The sooner you make these changes, the better off you'll likely be.
Following a heart healthy diet is an important part of managing heart failure. In fact, not having a proper diet can make heart failure worse. Ask your doctor and health care team to create an eating plan that works for you.
A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, eggs, poultry without skin, seafood, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt) and solid fats (saturated fat and trans fatty acids). Too much salt can cause extra fluid to build up in your body, making heart failure worse. Saturated fat and trans fatty acids can cause unhealthy blood cholesterol levels, which are a risk factor for heart disease.
A healthy diet also is low in added sugars and refined grains. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber). Examples of refined grains include white rice and white bread.
A balanced, nutrient-rich diet can help your heart work better. Getting enough potassium is important for people who have heart failure. Some heart failure medicines deplete the potassium in your body. Lack of potassium can cause very rapid heart rhythms that can lead to sudden death.
Potassium is found in foods like white potatoes and sweet potatoes, greens (such as spinach), bananas, many dried fruits, and white beans and soybeans.
Talk with your health care team about getting the correct amount of potassium. Too much potassium also can be harmful.
For more information about following a healthy diet, go to the National Heart, Lung, and Blood Institute's "Your Guide to Lowering Your Blood Pressure With DASH" and the U.S. Department of Agriculture's ChooseMyPlate.gov Web site. Both resources provide general information about healthy eating.
It's important for people who have heart failure to drink the correct amounts and types of fluid. Drinking too much fluid can worsen heart failure. Also, if you have heart failure, you shouldn't drink alcohol.
Talk with your doctor about what amounts and types of fluid you should have each day.
Taking steps to control risk factors for CHD, high blood pressure, and diabetes will help control heart failure. For example:
Your doctor will prescribe medicines based on the type of heart failure you have, how severe it is, and your response to certain medicines. The following medicines are commonly used to treat heart failure:
You should watch for signs that heart failure is getting worse. For example, weight gain may mean that fluids are building up in your body. Ask your doctor how often you should check your weight and when to report weight changes.
Getting medical care for other related conditions is important. If you have diabetes or high blood pressure, work with your health care team to control these conditions. Have your blood sugar level and blood pressure checked. Talk with your doctor about when you should have tests and how often to take measurements at home.
Try to avoid respiratory infections like the flu and pneumonia. Talk with your doctor or nurse about getting flu and pneumonia vaccines.
Many people who have severe heart failure may need treatment in a hospital from time to time. Your doctor may recommend oxygen therapy (oxygen given through nasal prongs or a mask). Oxygen therapy can be given in a hospital or at home.
As heart failure worsens, lifestyle changes and medicines may no longer control your symptoms. You may need a medical procedure or surgery.
If you have heart damage and severe heart failure symptoms, your doctor might recommend a cardiac resynchronization therapy (CRT) device or an implantable cardioverter defibrillator (ICD).
In heart failure, the right and left sides of the heart may no longer contract at the same time. This disrupts the heart's pumping. To correct this problem, your doctor might implant a CRT device (a type of pacemaker) near your heart.
This device helps both sides of your heart contract at the same time, which can decrease heart failure symptoms.
Some people who have heart failure have very rapid, irregular heartbeats. Without treatment, these heartbeats can cause sudden cardiac arrest. Your doctor might implant an ICD near your heart to solve this problem. An ICD checks your heart rate and uses electrical pulses to correct irregular heart rhythms.
People who have severe heart failure symptoms at rest, despite other treatments, may need:
Researchers continue to learn more about heart failure and how to treat it. As a result, treatments are getting better.
If you have heart failure, you may want to consider taking part in research studies called clinical trials. These studies offer care from experts and the chance to help advance heart failure knowledge and treatment.
For more information about clinical trials, go to the "Clinical Trials" section of this article.
If you have heart failure, you may also want to take part in a heart failure registry. The registry tracks the course of disease and treatment in large numbers of people. These data help research move forward. You may help yourself and others by taking part. Talk with your health care team to learn more.
ou can take steps to prevent heart failure. The sooner you start, the better your chances of preventing or delaying the condition.
If you have a healthy heart, you can take action to prevent heart disease and heart failure. To reduce your risk of heart disease:
Even if you're at high risk for heart failure, you can take steps to reduce your risk. People at high risk include those who have coronary heart disease, high blood pressure, or diabetes.
If you have heart damage but no signs of heart failure, you can still reduce your risk of developing the condition. In addition to the steps above, take your medicines as prescribed to reduce your heart's workload.
Currently, heart failure has no cure. You'll likely have to take medicine and follow a treatment plan for the rest of your life.
Despite treatment, symptoms may get worse over time. You may not be able to do many of the things that you did before you had heart failure. However, if you take all the steps your doctor recommends, you can stay healthier longer.
Researchers also might find new treatments that can help you in the future.
Treatment can relieve your symptoms and make daily activities easier. It also can reduce the chance that you'll have to go to the hospital. Thus, it's important that you follow your treatment plan.
Certain actions can worsen your heart failure, such as:
These actions can lead to a hospital stay. If you have trouble following your diet, talk with your doctor. He or she can help arrange for a dietitian to work with you. Avoid drinking alcohol.
People who have heart failure often have other serious conditions that require ongoing treatment. If you have other serious conditions, you're likely taking medicines for them as well as for heart failure.
Taking more than one medicine raises the risk of side effects and other problems. Make sure your doctors and your pharmacist have a complete list of all of the medicines and over-the-counter products that you're taking.
Tell your doctor right away about any problems with your medicines. Also, talk with your doctor before taking any new medicine prescribed by another doctor or any new over-the-counter medicines or herbal supplements.
Try to avoid respiratory infections like the flu and pneumonia. Ask your doctor or nurse about getting flu and pneumonia vaccines.
If you have heart failure, it's important to know:
Living with heart failure may cause fear, anxiety, depression, and stress. Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you're very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to living with heart failure. You can see how other people who have the same symptoms have coped with them. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has uncovered some of the causes of heart diseases and conditions, as well as ways to prevent or treat these disorders.
Many more questions remain about heart diseases and conditions, including heart failure. The NHLBI continues to support research aimed at learning more about heart failure, including:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart failure, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Source: NHLBI, NIH
The words "heart failure" sound alarming, but they do not mean that the heart has suddenly stopped working. Instead, heart failure means that the heart is not pumping as well as it should to deliver oxygen-rich blood to the body. Congestive heart failure (CHF) happens when the heart's pumping action becomes so weak that fluid begins to accumulate in the lungs and other body tissues. This fluid buildup is the “congestion” part of congestive heart failure.
CHF usually develops slowly. Patients may be symptom-free for years, but the symptoms tend to get worse with time. This slow onset and progression of CHF is due to the heart's efforts to accommodate for its gradual weakening. The heart attempts to make up for its weakening by enlarging and by pumping faster.
Who is at risk for developing CHF, and what are its causes?
According to the American Heart Association, people 40 and older have a 1 in 5 chance of developing CHF during their lifetime. Nearly 5 million people in the United States—mostly older adults—already have CHF, and the number of people with CHF is rising. Approximately 400,000 people develop CHF each year. People are living longer and surviving heart attacks and other medical conditions that put them at risk for CHF. People who have other types of heart and vessel disease are also at risk for CHF.
Risk factors for CHF include:
• Previous heart attack
• Coronary artery disease
• High blood pressure (hypertension)
• Irregular heartbeat (arrhythmia)
• Heart valve disease (especially of the aortic and mitral valves)
• Cardiomyopathy (disease of the heart muscle)
• Congenital heart defects (inborn defects)
• Alcohol and drug abuse
Symptoms
Symptoms help doctors determine which side of the heart is not working properly.
If the left side of the heart is not working properly (left-sided heart failure), blood and fluid back up into the lungs. Patients feel short of breath, are very tired, and have a cough (especially at night). In some cases, patients may begin to cough up pinkish, blood-tinged sputum.
If the right side of the heart is not working properly (right-sided heart failure), the slowed blood flow causes a buildup of fluid in the veins. The patient’s feet, legs, and ankles begin to swell. This swelling is called edema. Sometimes edema spreads to the lungs, liver, and stomach. Because of the fluid buildup, patients may need to go to the bathroom more often, especially at night. Fluid buildup is also hard on the kidneys. It affects their ability to dispose of salt (sodium) and water, which can lead to kidney failure. After CHF is treated, the kidneys' function usually returns to normal.
As heart failure progresses, the heart becomes weaker and symptoms begin. In addition to those listed above, here are some other symptoms of CHF:
• Trouble breathing or lying flat due to shortness of breath
• Feeling tired, weak, and unable to exercise or perform physical activities
• Weight gain from excess fluid
• Chest pain
• Poor appetite or indigestion
• Swollen neck veins
• Cold and sweaty skin
• Fast or irregular pulse
• Feeling restless or confused
• Decreased attention span and memory
Diagnosis
Tests that doctors use to diagnose CHF include taking a history and physical examination, listening for the crackling sounds of fluid in the lungs, the distinct sound of faulty valves (heart murmur), or the presence of a very quick heartbeat, tapping on the chest to determine fluid buildup, ordering blood tests, taking a chest x-ray, performing electrocardiography (ECG) and exercise testing, and using echocardiography and other imaging techniques, such as nuclear ventriculography or multiple-gated acquisition scanning (MUGA), and angiography.
Treatment
The goals of treatment include reducing the heart's workload, controlling excess salt and water retention, and improving the heart's function. In some cases, heart failure can be treated by correcting the underlying cause. For example, controlling a fast heart rhythm may reverse structural heart abnormalities. In many cases structural abnormalities cannot be corrected, but treatment can usually markedly decrease symptoms and increase life expectancy and quality of life. Treatment may include lifestyle changes, medicines, transcatheter interventions, and surgery.
Lifestyle Changes
The best way to prevent heart failure from progressing is to practice healthy lifestyle habits. It is also important to address any risk factors that contribute to heart failure, such as high blood pressure or coronary artery disease. Lifestyle habits to implement include:
• Quitting smoking
• Maintaining a healthy weight
• Controlling high blood pressure, cholesterol levels, and diabetes
• Eating a sensible diet that is low in calories, saturated fat, and salt
• Limiting alcohol consumption
• Limiting liquid consumption and caffeine
• Weighing daily to monitor fluid buildup
• Participating a doctor-approved aerobic exercise program
• Reducing stress
Medicines
Studies show that medicines help improve heart function and make it easier to exercise or do physical activity. The following medicines are often given to patients with CHF: diuretics, inotropics, blood-thinning medicines, vasodilators, calcium channel blockers, beta blockers, ACE inhibitors, and angiotensin II receptor blockers.
Percutaneous Coronary Interventions
CHF may be improved with the use of angioplasty, a procedure to open arteries narrowed by fatty plaque buildup. It is performed in a cardiac catheterization laboratory. Stenting is sometimes used along with balloon angioplasty. It involves placing a mesh-like metal device into an artery at a site narrowed by plaque. Inotropic drug therapy is a percutaneous intervention that can increase the heart's ability to beat. This medicine is given through a small catheter placed directly into an artery.
Surgical Procedures
The conditions underlying CHF may be improved with surgery. Surgical procedures that are often considered, depending on the individual patient, may include heart valve repair or replacement, pacemaker or ICD implantation, correction of congenital heart defects, coronary artery bypass surgery, mechanical assist devices, myectomy, and heart transplantation.
Patients who carefully follow their doctors' advice continue to live full and productive lives.
Source: International Heart Institute of Montana
Resources
Texas Heart Institute www.texasheartinstitute.com/HIC/Topics/Cond/CHF.cfm
Mayo Clinic www.mayoclinic.org/congestive-heart-failure/index.html
American Heart Association www.americanheart.org/presenter.jhtml?identifier=4585
A heart murmur is an extra or unusual sound heard during a heartbeat. Murmurs range from very faint to very loud. Sometimes they sound like a whooshing or swishing noise.
Normal heartbeats make a "lub-DUPP" or "lub-DUB" sound. This is the sound of the heart valves closing as blood moves through the heart. Doctors can hear these sounds and heart murmurs using a stethoscope.
The two types of heart murmurs are innocent (harmless) and abnormal.
Innocent heart murmurs aren't caused by heart problems. These murmurs are common in healthy children. Many children will have heart murmurs heard by their doctors at some point in their lives.
People who have abnormal heart murmurs may have signs or symptoms of heart problems. Most abnormal murmurs in children are caused by congenital (kon-JEN-ih-tal) heart defects. These defects are problems with the heart's structure that are present at birth.
In adults, abnormal heart murmurs most often are caused by acquired heart valve disease. This is heart valve disease that develops as the result of another condition. Infections, diseases, and aging can cause heart valve disease.
A heart murmur isn't a disease, and most murmurs are harmless. Innocent murmurs don't cause symptoms. Having one doesn't require you to limit your physical activity or do anything else special. Although you may have an innocent murmur throughout your life, you won't need treatment for it.
The outlook and treatment for abnormal heart murmurs depend on the type and severity of the heart problem causing them.
The heart is a muscle about the size of your fist. It works like a pump and beats 100,000 times a day.
The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen-rich blood from the lungs and pumps it to the body.
The heart has four chambers and four valves and is connected to various blood vessels. Veins are blood vessels that carry blood from the body to the heart. Arteries are blood vessels that carry blood away from the heart to the body.
Figure 1 shows the location of the heart in the body. Figure B shows a cross-section of a healthy heart and its inside structures. The blue arrow shows the direction in which oxygen-poor blood flows through the heart to the lungs. The red arrow shows the direction in which oxygen-rich blood flows from the lungs into the heart and then out to the body.
The heart has four chambers or "rooms."
Four valves control the flow of blood from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart.
Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward.
When the heart's valves open and close, they make a "lub-DUB" sound that a doctor can hear using a stethoscope.
The arteries are major blood vessels connected to your heart.
The veins also are major blood vessels connected to your heart.
For more information about how a healthy heart works, go to the Health Topics How the Heart Works article. This article contains animations that show how your heart pumps blood and how your heart's electrical system works.
Why some people have innocent heart murmurs and others do not isn't known. Innocent murmurs are simply sounds made by blood flowing through the heart's chambers and valves, or through blood vessels near the heart.
Extra blood flow through the heart also may cause innocent heart murmurs. After childhood, the most common cause of extra blood flow through the heart is pregnancy. This is because during pregnancy, women's bodies make extra blood. Most heart murmurs that occur in pregnant women are innocent.
Congenital heart defects or acquired heart valve disease often are the cause of abnormal heart murmurs.
Congenital heart defects are the most common cause of abnormal heart murmurs in children. These defects are problems with the heart's structure that are present at birth. They change the normal flow of blood through the heart.
Congenital heart defects can involve the interior walls of the heart, the valves inside the heart, or the arteries and veins that carry blood to and from the heart. Some babies are born with more than one heart defect.
Heart valve problems, septal defects (also called holes in the heart), and diseases of the heart muscle such as hypertrophic cardiomyopathy are common heart defects that cause abnormal heart murmurs.
Examples of valve problems are narrow valves that limit blood flow or leaky valves that don't close properly. Septal defects are holes in the wall that separates the right and left sides of the heart. This wall is called the septum.
A hole in the septum between the heart's two upper chambers is called an atrial septal defect. A hole in the septum between the heart's two lower chambers is called a ventricular septal defect.
Hypertrophic (hi-per-TROF-ik) cardiomyopathy (kar-de-o-mi-OP-ah-thee) (HCM) occurs if heart muscle cells enlarge and cause the walls of the ventricles (usually the left ventricle) to thicken. The thickening may block blood flow out of the ventricle. If a blockage occurs, the ventricle must work hard to pump blood to the body. HCM also can affect the heart’s mitral valve, causing blood to leak backward through the valve.
Figure A shows the structure and blood flow inside a normal heart. Figure B shows a heart with leaking and narrowed valves. Figure C shows a heart with a ventricular septal defect.
For more information, go to the Health Topics Congenital Heart Defects article.
Acquired heart valve disease often is the cause of abnormal heart murmurs in adults. This is heart valve disease that develops as the result of another condition.
Many conditions can cause heart valve disease. Examples include heart conditions and other disorders, age-related changes, rheumatic (ru-MAT-ik) fever, and infections.
Heart conditions and other disorders. Certain conditions can stretch and distort the heart valves, such as:
Damage and scar tissue from a heart attack or injury to the heart.
Advanced high blood pressure and heart failure. These conditions can enlarge the heart or its main arteries.
Age-related changes. As you get older, calcium deposits or other deposits may form on your heart valves. These deposits stiffen and thicken the valve flaps and limit blood flow. This stiffening and thickening of the valve is called sclerosis (skle-RO-sis).
Rheumatic fever. The bacteria that cause strep throat, scarlet fever, and, in some cases, impetigo (im-peh-TI-go) also can cause rheumatic fever. This serious illness can develop if you have an untreated or not fully treated streptococcal (strep) infection.
Rheumatic fever can damage and scar the heart valves. The symptoms of this heart valve damage often don't occur until many years after recovery from rheumatic fever.
Today, most people who have strep infections are treated with antibiotics before rheumatic fever develops. It's very important to take all of the antibiotics your doctor prescribes for strep throat, even if you feel better before the medicine is gone.
Infections. Common germs that enter the bloodstream and get carried to the heart can sometimes infect the inner surface of the heart, including the heart valves. This rare but sometimes life-threatening infection is called infective endocarditis (EN-do-kar-DI-tis), or IE.
IE is more likely to develop in people who already have abnormal blood flow through a heart valve because of heart valve disease. The abnormal blood flow causes blood clots to form on the surface of the valve. The blood clots make it easier for germs to attach to and infect the valve.
IE can worsen existing heart valve disease.
Some heart murmurs occur because of an illness outside of the heart. The heart is normal, but an illness or condition can cause blood flow that's faster than normal. Examples of this type of illness include fever, anemia (uh-NEE-me-eh), and hyperthyroidism.
Anemia is a condition in which the body has a lower than normal number of red blood cells. Hyperthyroidism is a condition in which the body has too much thyroid hormone.
People who have innocent (harmless) heart murmurs don't have any signs or symptoms other than the murmur itself. This is because innocent heart murmurs aren't caused by heart problems.
People who have abnormal heart murmurs may have signs or symptoms of the heart problems causing the murmurs. These signs and symptoms may include:
Signs and symptoms depend on the problem causing the heart murmur and its severity.
Doctors use a stethoscope to listen to heart sounds and hear heart murmurs. They may detect heart murmurs during routine checkups or while checking for another condition.
If a congenital heart defect causes a murmur, it's often heard at birth or during infancy. Abnormal heart murmurs caused by other heart problems can be heard in patients of any age.
Primary care doctors usually refer people who have abnormal heart murmurs to cardiologists or pediatric cardiologists for further care and testing.
Cardiologists are doctors who specialize in diagnosing and treating heart problems in adults. Pediatric cardiologists specialize in diagnosing and treating heart problems in children.
Your doctor will carefully listen to your heart or your child's heart with a stethoscope to find out whether a murmur is innocent or abnormal. He or she will listen to the loudness, location, and timing of the murmur. This will help your doctor diagnose the cause of the murmur.
Your doctor also may:
When evaluating a heart murmur, your doctor will pay attention to many things, such as:
If your doctor thinks you or your child has an abnormal heart murmur, he or she may recommend one or more of the following tests.
A chest x ray is a painless test that creates pictures of the structures inside your chest, such as your heart, lungs, and blood vessels. This test is done to find the cause of symptoms, such as shortness of breath and chest pain.
An EKG (electrocardiogram) is a simple test that detects and records the heart's electrical activity. An EKG shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
This test is used to detect and locate the source of heart problems. The results from an EKG also may be used to rule out certain heart problems.
Echocardiography (EK-o-kar-de-OG-ra-fee), or echo, is a painless test that uses sound waves to create pictures of your heart. The test shows the size and shape of your heart and how well your heart's chambers and valves are working.
Echo also can show areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
There are several types of echo, including a stress echo. This test is done both before and after a stress test. During this test, you exercise to make your heart work hard and beat fast. If you can’t exercise, you may be given medicine to make your heart work hard and beat fast. Echo is used to take pictures of your heart before you exercise and as soon as you finish.
Stress echo shows whether you have decreased blood flow to your heart (a sign of coronary heart disease).
A heart murmur isn't a disease. It's an extra or unusual sound heard during the heartbeat. Thus, murmurs themselves don't require treatment. However, if an underlying condition is causing a heart murmur, your doctor may recommend treatment for that condition.
Healthy children who have innocent (harmless) heart murmurs don't need treatment. Their heart murmurs aren't caused by heart problems or other conditions.
Pregnant women who have innocent heart murmurs due to extra blood volume also don't need treatment. Their heart murmurs should go away after pregnancy.
If you or your child has an abnormal heart murmur, your doctor will recommend treatment for the disease or condition causing the murmur.
Some medical conditions, such as anemia or hyperthyroidism, can cause heart murmurs that aren't related to heart disease. Treating these conditions should make the heart murmur go away.
If a congenital heart defect is causing a heart murmur, treatment will depend on the type and severity of the defect. Treatment may include medicines or surgery. For more information about treatments for congenital heart defects, go to the Health Topics Congenital Heart Defects article.
If acquired heart valve disease is causing a heart murmur, treatment usually will depend on the type, amount, and severity of the disease.
Currently, no medicines can cure heart valve disease. However, lifestyle changes and medicines can treat symptoms and help delay complications. Eventually, though, you may need surgery to repair or replace a faulty heart valve.
For more information about treatments for heart valve disease, go to the Health Topics Heart Valve Disease article.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. Often, these advances depend on the willingness of volunteers to take part in clinical trials.
Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions. For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart murmurs or other heart diseases or conditions, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Source: NHLBI, NIH
Palpitations (pal-pi-TA-shuns) are feelings that your heart is skipping a beat, fluttering, or beating too hard or too fast. You may have these feelings in your chest, throat, or neck. They can occur during activity or even when you're sitting still or lying down.
Many things can trigger palpitations, including:
These factors can make the heart beat faster or stronger than usual, or they can cause premature (extra) heartbeats. In these situations, the heart is still working normally. Thus, these palpitations usually are harmless.
Some palpitations are symptoms of arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat.
Some arrhythmias are signs of heart conditions, such as heart attack, heart failure, heart valve disease, or heart muscle disease. However, less than half of the people who have palpitations have arrhythmias.
You can take steps to reduce or prevent palpitations. Try to avoid things that trigger them (such as stress and stimulants) and treat related medical conditions.
Palpitations are very common. They usually aren't serious or harmful, but they can be bothersome. If you have them, your doctor can decide whether you need treatment or ongoing care.
Many things can cause palpitations. You may have these feelings even when your heart is beating normally or somewhat faster than normal.
Most palpitations are harmless and often go away on their own. However, some palpitations are signs of a heart problem. Sometimes the cause of palpitations can't be found.
If you start having palpitations, see your doctor to have them checked.
You may feel your heart pounding or racing during anxiety, fear, or stress. You also may have these feelings if you're having a panic attack.
Intense activity can make your heart feel like it’s beating too hard or too fast, even though it's working normally. Intense activity also can cause occasional premature (extra) heartbeats.
Some medical conditions can cause palpitations. These conditions can make the heart beat faster or stronger than usual. They also can cause premature (extra) heartbeats.
Examples of these medical conditions include:
The hormonal changes that happen during pregnancy, menstruation, and the perimenopausal period may cause palpitations. The palpitations will likely improve or go away as these conditions go away or change.
Some palpitations that occur during pregnancy may be due to anemia.
Many medicines can trigger palpitations because they can make the heart beat faster or stronger than usual. Medicines also can cause premature (extra) heartbeats.
Examples of these medicines include:
Over-the-counter medicines that act as stimulants also may cause palpitations. These include decongestants (found in cough and cold medicines) and some herbal and nutritional supplements.
Caffeine, nicotine (found in tobacco), alcohol, and illegal drugs (such as cocaine and amphetamines) also can cause palpitations.
Some palpitations are symptoms of arrhythmias. Arrhythmias are problems with the rate or rhythm of the heartbeat. However, less than half of the people who have palpitations have arrhythmias.
During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. An arrhythmia happens if some part of the heart's electrical system doesn't work as it should.
Palpitations are more likely to be related to an arrhythmia if you:
Some people may be more likely than others to have palpitations. People at increased risk include those who:
Women who are pregnant, menstruating, or perimenopausal also may be at higher risk for palpitations because of hormonal changes. Some palpitations that occur during pregnancy may be due to anemia.
For more information about these risk factors, go to "What Causes Palpitations?"
Symptoms of palpitations include feelings that your heart is:
You may have these feelings in your chest, throat, or neck. They can occur during activity or even when you're sitting still or lying down.
Palpitations often are harmless, and your heart is working normally. However, these feelings can be a sign of a more serious problem if you also:
Your doctor may have already told you that your palpitations are harmless. Even so, see your doctor again if your palpitations:
Your doctor will want to check whether your palpitations are the symptom of a heart problem, such as an arrhythmia (irregular heartbeat).
First, your doctor will want to find out whether your palpitations are harmless or related to a heart problem. He or she will ask about your symptoms and medical history, do a physical exam, and recommend several basic tests.
This information may point to a heart problem as the cause of your palpitations. If so, your doctor may recommend more tests. These tests will help show what the problem is, so your doctor can decide how to treat it.
The cause of palpitations may be hard to diagnose, especially if symptoms don't occur regularly.
Several types of doctors may work with you to diagnose and treat your palpitations. These include a:
Your doctor will ask questions about your palpitations, such as:
Your doctor also may ask about your use of caffeine, alcohol, supplements, and illegal drugs.
Your doctor will take your pulse to find out how fast your heart is beating and whether its rhythm is normal. He or she also will use a stethoscope to listen to your heartbeat.
Your doctor may look for signs of conditions that can cause palpitations, such as an overactive thyroid.
Often, the first test that's done is an EKG (electrocardiogram). This simple test records your heart's electrical activity.
An EKG shows how fast your heart is beating and its rhythm (steady or irregular). It also records the strength and timing of electrical signals as they pass through your heart.
Even if your EKG results are normal, you may still have a medical condition that's causing palpitations. If your doctor suspects this is the case, you may have blood tests to gather more information about your heart's structure, function, and electrical system.
A standard EKG only records the heartbeat for a few seconds. It won't detect heart rhythm problems that don't happen during the test. To diagnose problems that come and go, your doctor may have you wear a Holter or event monitor.
A Holter monitor records the heart’s electrical activity for a full 24- or 48-hour period. You wear patches called electrodes on your chest. Wires connect the patches to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
During the 24- or 48-hour period, you do your usual daily activities. You use a notebook to record any symptoms you have and the time they occur. You then return both the recorder and the notebook to your doctor to read the results. Your doctor can see how your heart was beating at the time you had symptoms.
An event monitor is similar to a Holter monitor. You wear an event monitor while doing your normal activities. However, an event monitor only records your heart's electrical activity at certain times while you're wearing it.
For many event monitors, you push a button to start the monitor when you feel symptoms. Other event monitors start automatically when they sense abnormal heart rhythms.
You can wear an event monitor for weeks or until symptoms occur.
Figure A shows how a Holter or event monitor attaches to a patient. In this example, the monitor is clipped to the patient's belt and electrodes are attached to his chest. Figure B shows an electrocardiogram strip, which maps the data from the Holter or event monitor.
Echocardiography uses sound waves to create a moving picture of your heart. The picture shows the size and shape of your heart and how well your heart chambers and valves are working.
The test also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can’t exercise, you may be given medicine to make your heart work hard and beat fast.
Treatment for palpitations depends on their cause. Most palpitations are harmless and often go away on their own. In these cases, no treatment is needed.
Your palpitations may be harmless but bothersome. If so, your doctor may suggest avoiding things that trigger them. For examples, your doctor may advise you to:
Work with your doctor to control medical conditions that can cause palpitations, such as an overactive thyroid. If you're taking medicine that's causing palpitations, your doctor will try to find a different medicine for you.
If your palpitations are caused by an arrhythmia (irregular heartbeat), your doctor may recommend medicines or procedures to treat the problem. For more information, go to the Health Topics Arrhythmia article.
You can take steps to prevent palpitations. Try to avoid things that trigger them. For example:
Also, work with your doctor to treat medical conditions that can cause palpitations.
Most palpitations are harmless and often go away on their own. Treatment usually isn’t needed in these cases. Your doctor may advise you to avoid triggers for palpitations. (For more information, go to "How Are Palpitations Treated?")
Your doctor may have already told you that your palpitations are harmless. Even so, see your doctor again if they get worse, start to occur more often, become more noticeable or bothersome, or occur with other symptoms.
Your doctor will tell you about other signs and symptoms to be aware of and when to seek emergency care.
A medical condition or heart problem might be the cause of your palpitations. If so, your doctor will give you advice and treatment for your condition.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. Often, these advances depend on the willingness of volunteers to take part in clinical trials.
Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions. For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they’re widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don’t directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You’ll learn about treatments and tests you may receive, and the benefits and risks they may pose. You’ll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you’ll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to palpitations, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI’s Children and Clinical Studies Web page.
Source: NHLBI, NIH
Heart block is a problem that occurs with the heart's electrical system. This system controls the rate and rhythm of heartbeats. ("Rate" refers to the number of times your heart beats per minute. "Rhythm" refers to the pattern of regular or irregular pulses produced as the heart beats.)
With each heartbeat, an electrical signal spreads across the heart from the upper to the lower chambers. As it travels, the signal causes the heart to contract and pump blood.
Heart block occurs if the electrical signal is slowed or disrupted as it moves through the heart.
Heart block is a type of arrhythmia (ah-RITH-me-ah). An arrhythmia is any problem with the rate or rhythm of the heartbeat.
Some people are born with heart block, while others develop it during their lifetimes. If you're born with the condition, it's called congenital (kon-JEN-ih-tal) heart block. If the condition develops after birth, it's called acquired heart block.
Doctors might detect congenital heart block before or after a baby is born. Certain diseases that may occur during pregnancy can cause heart block in a baby. Some congenital heart defects also can cause heart block. Congenital heart defects are problems with the heart's structure that are present at birth. Often, doctors don't know what causes these defects.
Acquired heart block is more common than congenital heart block. Damage to the heart muscle or its electrical system causes acquired heart block. Diseases, surgery, or medicines can cause this damage.
The three types of heart block are first degree, second degree, and third degree. First degree is the least severe, and third degree is the most severe. This is true for both congenital and acquired heart block.
Doctors use a test called an EKG (electrocardiogram) to help diagnose heart block. This test detects and records the heart's electrical activity. It maps the data on a graph for the doctor to review.
The symptoms and severity of heart block depend on which type you have. First-degree heart block may not cause any severe symptoms.
Second-degree heart block may result in the heart skipping a beat or beats. This type of heart block also can make you feel dizzy or faint.
Third-degree heart block limits the heart's ability to pump blood to the rest of the body. This type of heart block may cause fatigue (tiredness), dizziness, and fainting. Third-degree heart block requires prompt treatment because it can be fatal.
A medical device called a pacemaker is used to treat third-degree heart block and some cases of second-degree heart block. This device uses electrical pulses to prompt the heart to beat at a normal rate. Pacemakers typically are not used to treat first-degree heart block.
All types of heart block may increase your risk for other arrhythmias, such as atrial fibrillation (A-tre-al fih-brih-LA-shun). Talk with your doctor to learn more about the signs and symptoms of arrhythmias.
Doctors use a test called an EKG (electrocardiogram) to help diagnose heart block. This test detects and records the heart's electrical activity. An EKG records the strength and timing of electrical signals as they pass through the heart.
The data are recorded on a graph so your doctor can study your heart's electrical activity. Different parts of the graph show each step of an electrical signal's journey through the heart.
Each electrical signal begins in a group of cells called the sinus node or sinoatrial (SA) node. The SA node is located in the right atrium (AY-tree-um), which is the upper right chamber of the heart. (Your heart has two upper chambers and two lower chambers.)
In a healthy adult heart at rest, the SA node sends an electrical signal to begin a new heartbeat 60 to 100 times a minute.
From the SA node, the signal travels through the right and left atria. This causes the atria to contract, which helps move blood into the heart's lower chambers, the ventricles (VEN-trih-kuls). The electrical signal moving through the atria is recorded as the P wave on the EKG.
The electrical signal passes between the atria and ventricles through a group of cells called the atrioventricular (AV) node. The signal slows down as it passes through the AV node. This slowing allows the ventricles enough time to finish filling with blood. On the EKG, this part of the process is the flat line between the end of the P wave and the beginning of the Q wave.
The electrical signal then leaves the AV node and travels along a pathway called the bundle of His. From there, the signal travels into the right and left bundle branches. The signal spreads quickly across your heart's ventricles, causing them to contract and pump blood to your lungs and the rest of your body. This process is recorded as the QRS waves on the EKG.
The ventricles then recover their normal electrical state (shown as the T wave on the EKG). The muscle stops contracting to allow the heart to refill with blood. This entire process continues over and over with each new heartbeat.
The animation below shows how your heart's electrical system works and how an EKG records your heart's electrical activity. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
The animation shows how an electrical signal moves through your heart and how an EKG records your heart's electrical activity.
For more information about the heart's electrical system, go to the Health Topics How the Heart Works article.
Some people are born with heart block (congenital), while others develop it during their lifetimes (acquired). Acquired heart block is more common than congenital heart block.
The three types of heart block are first degree, second degree, and third degree. First degree is the least severe, and third degree is the most severe. This is true for both congenital and acquired heart block.
In first-degree heart block, the heart's electrical signals are slowed as they move from the atria to the ventricles (the heart's upper and lower chambers, respectively). This results in a longer, flatter line between the P and the R waves on the EKG (electrocardiogram).
First-degree heart block may not cause any symptoms or require treatment.
In this type of heart block, electrical signals between the atria and ventricles are slowed to a large degree. Some signals don't reach the ventricles. On an EKG, the pattern of QRS waves doesn't follow each P wave as it normally would.
If an electrical signal is blocked before it reaches the ventricles, they won't contract and pump blood to the lungs and the rest of the body.
Second-degree heart block is divided into two types: Mobitz type I and Mobitz type II.
In this type (also known as Wenckebach's block), the electrical signals are delayed more and more with each heartbeat, until the heart skips a beat. On the EKG, the delay is shown as a line (called the PR interval) between the P and QRS waves. The line gets longer and longer until the QRS waves don't follow the next P wave.
Sometimes people who have Mobitz type I feel dizzy or have other symptoms. This type of second-degree heart block is less serious than Mobitz type II.
The animation below shows how your heart's electrical system works. It also shows what happens during second-degree Mobitz type I heart block. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
The first part of this animation is the same as the animation in the section on understanding the heart's electrical system and EKG results. If you want to skip directly to the frames on Mobitz type I heart block, click the "skip intro" link above the start, pause, and replay buttons.
The first part of the animation shows how an electrical signal moves through your heart and how an EKG records your heart's electrical activity. The second part of the animation shows how a pause in the heart's electrical signal can delay or block the contraction of the ventricles.
In second-degree Mobitz type II heart block, some of the electrical signals don't reach the ventricles. However, the pattern is less regular than it is in Mobitz type I. Some signals move between the atria and ventricles normally, while others are blocked.
On an EKG, the QRS wave follows the P wave at a normal speed. Sometimes, though, the QRS wave is missing (when a signal is blocked).
Mobitz type II is less common than type I, but it's usually more severe. Some people who have type II need medical devices called pacemakers to maintain their heart rates.
In this type of heart block, none of the electrical signals reach the ventricles. This type also is called complete heart block or complete AV block.
When complete heart block occurs, special areas in the ventricles may create electrical signals to cause the ventricles to contract. This natural backup system is slower than the normal heart rate and isn't coordinated with the contraction of the atria. On an EKG, the normal pattern is disrupted. The P waves occur at a faster rate, and it isn't coordinated with the QRS waves.
Complete heart block can result in sudden cardiac arrest and death. This type of heart block often requires emergency treatment. A temporary pacemaker might be used to keep the heart beating until you get a long-term pacemaker.
Heart block has many causes. Some people are born with the disorder (congenital), while others develop it during their lifetimes (acquired).
One form of congenital heart block occurs in babies whose mothers have autoimmune diseases, such as lupus. People who have these diseases make proteins called antibodies that attack and damage the body's tissues or cells.
In pregnant women, antibodies can cross the placenta. (The placenta is the organ that attaches the umbilical cord to the mother's womb.) These proteins can damage the baby's heart and lead to congenital heart block.
Congenital heart defects also may cause congenital heart block. These defects are problems with the heart's structure that are present at birth. Often, doctors don't know what causes these defects.
Many factors can cause acquired heart block. Examples include:
Other diseases may increase the risk of heart block. Examples include sarcoidosis (sar-koy-DOE-sis) and the degenerative muscle disorders Lev's disease and Lenegre's disease.
Certain types of surgery also may damage the heart's electrical system and lead to heart block.
Exposure to toxic substances and taking certain medicines—including digitalis, beta blockers, and calcium channel blockers—also may cause heart block. Doctors closely watch people who are taking these medicines for signs of problems.
Some types of heart block have been linked to genetic mutations (changes in the genes).
An overly active vagus nerve also can cause heart block. You have one vagus nerve on each side of your body. These nerves run from your brain stem all the way to your abdomen. Activity in the vagus nerve slows the heart rate.
In some cases, acquired heart block may go away if the factor causing it is treated or resolved. For example, heart block that occurs after a heart attack or surgery may go away during recovery.
Also, if a medicine is causing heart block, the disorder may go away if the medicine is stopped or the dosage is lowered. Always talk with your doctor before you change the way you take your medicines.
The risk factors for congenital and acquired heart block are different.
If a pregnant woman has an autoimmune disease, such as lupus, her fetus is at risk for heart block.
Autoimmune diseases can cause the body to make proteins called antibodies that can cross the placenta. (The placenta is the organ that attaches the umbilical cord to the mother's womb.) These antibodies may damage the baby's heart and lead to congenital heart block.
Congenital heart defects also can cause heart block. These defects are problems with the heart's structure that are present at birth. Most of the time, doctors don't know what causes congenital heart defects.
Heredity may play a role in certain heart defects. For example, a parent who has a congenital heart defect might be more likely than other people to have a child with the condition.
Acquired heart block can occur in people of any age. However, most types of the condition are more common in older people. This is because many of the risk factors are more common in older people.
People who have a history of heart disease or heart attacks are at increased risk for heart block. Examples of heart disease that can lead to heart block include heart failure, coronary heart disease, and cardiomyopathy (heart muscle diseases).
Other diseases also may raise the risk of heart block, such as sarcoidosis and the degenerative muscle disorders Lev's disease and Lenegre's disease.
Exposure to toxic substances or taking certain medicines, such as digitalis, also can raise your risk for heart block.
Well-trained athletes and young people are at higher risk for first-degree heart block caused by an overly active vagus nerve. You have one vagus nerve on each side of your body. These nerves run from your brain stem all the way to your abdomen. Activity in the vagus nerve slows the heart rate.
Signs and symptoms depend on the type of heart block you have. First-degree heart block may not cause any symptoms.
Signs and symptoms of second- and third-degree heart block include:
These symptoms may suggest other health problems as well. If these symptoms are new or severe, call 9–1–1 or have someone drive you to the hospital emergency room. If you have milder symptoms, talk with your doctor right away to find out whether you need prompt treatment.
Heart block might be diagnosed as part of a routine doctor's visit or during an emergency situation. (Third-degree heart block often is an emergency.)
Your doctor will diagnose heart block based on your family and medical histories, a physical exam, and test results.
Your primary care doctor might be involved in diagnosing heart block. However, if you have the condition, you might need to see a heart specialist. Heart specialists include:
Your doctor may ask whether:
Your doctor also may ask about other health habits, such as how physically active you are.
During the physical exam, your doctor will listen to your heart. He or she will listen carefully for abnormal rhythms or heart murmurs (extra or unusual sounds heard during heartbeats).
Your doctor also may:
Doctors usually use an EKG (electrocardiogram) to help diagnose heart block. This simple test detects and records the heart's electrical activity.
An EKG shows how fast the heart is beating and its rhythm (steady or irregular). The test also records the strength and timing of electrical signals as they pass through the heart.
The data are recorded on a graph. Different types of heart block have different patterns on the graph. (For more information, go to "Types of Heart Block.")
A standard EKG only records the heart's activity for a few seconds. To diagnose heart rhythm problems that come and go, your doctor may have you wear a portable EKG monitor.
The most common types of portable EKGs are Holter and event monitors. Your doctor may have you use one of these monitors to diagnose first- or second-degree heart block.
A Holter monitor records the heart's electrical signals for a full 24- or 48-hour period. You wear one while you do your normal daily activities. This allows the monitor to record your heart for a longer time than a standard EKG.
An event monitor is similar to a Holter monitor. You wear an event monitor while doing your normal activities. However, an event monitor only records your heart's electrical activity at certain times while you're wearing it.
You may wear an event monitor for 1 to 2 months, or as long as it takes to get a recording of your heart during symptoms.
For some cases of heart block, doctors may do electrophysiology studies (EPS). During this test, a thin, flexible wire is passed through a vein in your groin (upper thigh) or arm to your heart. The wire records your heart's electrical signals.
To diagnose heart block, your doctor may recommend tests to rule out other types of arrhythmias (irregular heartbeats). For more information, go to "How Are Arrhythmias Diagnosed?"
Treatment depends on the type of heart block you have. If you have first-degree heart block, you may not need treatment.
If you have second-degree heart block, you may need a pacemaker. A pacemaker is a small device that's placed under the skin of your chest or abdomen. This device uses electrical pulses to prompt the heart to beat at a normal rate.
If you have third-degree heart block, you will need a pacemaker. In an emergency, a temporary pacemaker might be used until you can get a long-term device. Most people who have third-degree heart block need pacemakers for the rest of their lives.
Some people who have third-degree congenital heart block don't need pacemakers for many years. Others may need pacemakers at a young age or during infancy.
If a pregnant woman has an autoimmune disease, such as lupus, her fetus is at risk for heart block. If heart block is detected in a fetus, the mother might be given medicine to reduce the fetus' risk of developing serious heart block.
Sometimes acquired heart block goes away if the factor causing it is treated or resolved. For example, heart block that occurs after a heart attack or surgery may go away during recovery.
Also, if a medicine is causing heart block, the condition may go away if the medicine is stopped or the dosage is lowered. (Always talk with your doctor before you change the way you take your medicines.)
First-degree heart block may not cause any symptoms or require treatment. However, some research has shown that people who have first-degree heart block might be at higher risk for atrial fibrillation (AF) in the future.
AF is a type of arrhythmia. It occurs if rapid, disorganized electrical signals cause the heart's upper chambers to contract very fast and irregularly.
If you've been diagnosed with first-degree heart block, ask your doctor whether you need to take any special steps to control it.
Your doctor can tell you whether you need ongoing care or whether you need to change the way you take certain medicines.
If you have second-degree heart block that doesn't require a pacemaker, talk with your doctor about keeping your heart healthy. Your doctor will tell you whether you need ongoing care for your condition.
People who have third-degree heart block and some people who have second-degree heart block need pacemakers. These devices use electrical pulses to prompt the heart to beat at a normal rate.
If you have a pacemaker, you should take special care to avoid things that may interfere with it. Avoid close or prolonged contact with electrical devices and devices that have strong magnetic fields. These objects can keep your pacemaker from working properly.
Let all of your doctors, dentists, and medical technicians know that you have a pacemaker. You also should notify airport screeners.
Your doctor can give you a card that states what kind of pacemaker you have. Carry this card in your wallet. You may want to wear a medical ID bracelet or necklace that states that you have a pacemaker.
Certain medical procedures can disrupt pacemakers. Examples include MRI (magnetic resonance imaging), electrocauterization during surgery, and shock-wave lithotripsy to get rid of kidney stones.
Your doctor may need to check your pacemaker several times a year to make sure it's working well. Some pacemakers must be checked in the doctor's office, but others can be checked over the phone.
Ask your doctor about what types of physical activity are safe for you. A pacemaker usually won't limit you from doing sports and physical activity. But you may need to avoid full-contact sports, such as football, that can damage the pacemaker.
For more information about living with a pacemaker, go to the Health Topics Pacemaker article.
Source: NHLBI, NIH
An electrocardiogram (e-lek-tro-KAR-de-o-gram), also called an EKG or ECG, is a simple, painless test that records the heart's electrical activity. To understand this test, it helps to understand how the heart works.
With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As it travels, the signal causes the heart to contract and pump blood. The process repeats with each new heartbeat.
The heart's electrical signals set the rhythm of the heartbeat. For more detailed information and animations, go to the Health Topics How the Heart Works article.
An EKG shows:
Doctors use EKGs to detect and study many heart problems, such as heart attacks, arrhythmias (ah-RITH-me-ahs), and heart failure. The test's results also can suggest other disorders that affect heart function.
An electrocardiogram also is called an EKG or ECG. Sometimes the test is called a 12-lead EKG or 12-lead ECG. This is because the heart's electrical activity most often is recorded from 12 different places on the body at the same time.
Your doctor may recommend an electrocardiogram (EKG) if you have signs or symptoms that suggest a heart problem. Examples of such signs and symptoms include:
You may need to have more than one EKG so your doctor can diagnose certain heart conditions.
An EKG also may be done as part of a routine health exam. The test can screen for early heart disease that has no symptoms. Your doctor is more likely to look for early heart disease if your mother, father, brother, or sister had heart disease—especially early in life.
You may have an EKG so your doctor can check how well heart medicine or a medical device, such as a pacemaker, is working. The test also may be used for routine screening before major surgery.
Your doctor also may use EKG results to help plan your treatment for a heart condition.
You don't need to take any special steps before having an electrocardiogram (EKG). However, tell your doctor or his or her staff about the medicines you're taking. Some medicines can affect EKG results.
An electrocardiogram (EKG) is painless and harmless. A nurse or technician will attach soft, sticky patches called electrodes to the skin of your chest, arms, and legs. The patches are about the size of a quarter.
Often, 12 patches are attached to your body. This helps detect your heart's electrical activity from many areas at the same time. The nurse may have to shave areas of your skin to help the patches stick.
After the patches are placed on your skin, you'll lie still on a table while the patches detect your heart's electrical signals. A machine will record these signals on graph paper or display them on a screen.
The entire test will take about 10 minutes.
The standard EKG described above, called a resting 12-lead EKG, only records seconds of heart activity at a time. It will show a heart problem only if the problem occurs during the test.
Many heart problems are present all the time, and a resting 12-lead EKG will detect them. But some heart problems, like those related to an irregular heartbeat, can come and go. They may occur only for a few minutes a day or only while you exercise.
Doctors use special EKGs, such as stress tests and Holter and event monitors, to help diagnose these kinds of problems.
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise to make your heart work hard and beat fast while an EKG is done. If you can't exercise, you'll be given medicine to make your heart work hard and beat fast.
For more information, go to the Health Topics Stress Testing article.
Holter and event monitors are small, portable devices. They record your heart's electrical activity while you do your normal daily activities. A Holter monitor records your heart's electrical activity for a full 24- or 48-hour period.
An event monitor records your heart's electrical activity only at certain times while you're wearing it. For many event monitors, you push a button to start the monitor when you feel symptoms. Other event monitors start automatically when they sense abnormal heart rhythms.
For more information, go to the Health Topics Holter and Event Monitors article.
After an electrocardiogram (EKG), the nurse or technician will remove the electrodes (soft patches) from your skin. You may develop a rash or redness where the EKG patches were attached. This mild rash often goes away without treatment.
You usually can go back to your normal daily routine after an EKG.
Many heart problems change the heart's electrical activity in distinct ways. An electrocardiogram (EKG) can help detect these heart problems.
EKG recordings can help doctors diagnose heart attacks that are in progress or have happened in the past. This is especially true if doctors can compare a current EKG recording to an older one.
An EKG also can show:
An EKG can reveal whether the heartbeat starts in the correct place in the heart. The test also shows how long it takes for electrical signals to travel through the heart. Delays in signal travel time may suggest heart block or long QT syndrome.
An electrocardiogram (EKG) has no serious risks. It's a harmless, painless test that detects the heart's electrical activity. EKGs don't give off electrical charges, such as shocks.
You may develop a mild rash where the electrodes (soft patches) were attached. This rash often goes away without treatment.
Source: NHLBI, NIH
What Is Heart Valve Disease?
Heart valve disease occurs if one or more of your heart valves don't work well. The heart has four valves: the tricuspid (tri-CUSS-pid), pulmonary (PULL-mun-ary), mitral (MI-trul), and aortic (ay-OR-tik) valves.
These valves have tissue flaps that open and close with each heartbeat. The flaps make sure blood flows in the right direction through your heart's four chambers and to the rest of your body.
Figure A shows the location of the heart in the body. Figure B shows a cross-section of a healthy heart and its inside structures. The blue arrow shows the direction in which oxygen-poor blood flows through the heart to the lungs. The red arrow shows the direction in which oxygen-rich blood flows from the lungs into the heart and then out to the body.
Birth defects, age-related changes, infections, or other conditions can cause one or more of your heart valves to not open fully or to let blood leak back into the heart chambers. This can make your heart work harder and affect its ability to pump blood.
At the start of each heartbeat, blood returning from the body and lungs fills the atria (the heart's two upper chambers). The mitral and tricuspid valves are located at the bottom of these chambers. As the blood builds up in the atria, these valves open to allow blood to flow into the ventricles (the heart's two lower chambers).
After a brief delay, as the ventricles begin to contract, the mitral and tricuspid valves shut tightly. This prevents blood from flowing back into the atria.
As the ventricles contract, they pump blood through the pulmonary and aortic valves. The pulmonary valve opens to allow blood to flow from the right ventricle into the pulmonary artery. This artery carries blood to the lungs to get oxygen.
At the same time, the aortic valve opens to allow blood to flow from the left ventricle into the aorta. The aorta carries oxygen-rich blood to the body. As the ventricles relax, the pulmonary and aortic valves shut tightly. This prevents blood from flowing back into the ventricles.
For more information about how the heart pumps blood and detailed animations, go to the Health Topics How the Heart Works article.
Heart valves can have three basic kinds of problems: regurgitation (re-GUR-jih-TA-shun), stenosis (ste-NO-sis), and atresia (a-TRE-ze-ah).
Regurgitation, or backflow, occurs if a valve doesn't close tightly. Blood leaks back into the chambers rather than flowing forward through the heart or into an artery.
In the United States, backflow most often is due to prolapse. "Prolapse" is when the flaps of the valve flop or bulge back into an upper heart chamber during a heartbeat. Prolapse mainly affects the mitral valve.
Stenosis occurs if the flaps of a valve thicken, stiffen, or fuse together. This prevents the heart valve from fully opening. As a result, not enough blood flows through the valve. Some valves can have both stenosis and backflow problems.
Atresia occurs if a heart valve lacks an opening for blood to pass through.
Some people are born with heart valve disease, while others acquire it later in life. Heart valve disease that develops before birth is called congenital (kon-JEN-ih-tal) heart valve disease. Congenital heart valve disease can occur alone or with other congenital heart defects.
Congenital heart valve disease often involves pulmonary or aortic valves that don't form properly. These valves may not have enough tissue flaps, they may be the wrong size or shape, or they may lack an opening through which blood can flow properly.
Acquired heart valve disease usually involves aortic or mitral valves. Although the valves are normal at first, problems develop over time.
Both congenital and acquired heart valve disease can cause stenosis or backflow.
Many people have heart valve defects or disease but don't have symptoms. For some people, the condition mostly stays the same throughout their lives and doesn't cause any problems.
For other people, heart valve disease slowly worsens until symptoms develop. If not treated, advanced heart valve disease can cause heart failure, stroke, blood clots, or death due to sudden cardiac arrest (SCA).
Currently, no medicines can cure heart valve disease. However, lifestyle changes and medicines can relieve many of its symptoms and complications.
These treatments also can lower your risk of developing a life-threatening condition, such as stroke or SCA. Eventually, you may need to have your faulty heart valve repaired or replaced.
Some types of congenital heart valve disease are so severe that the valve is repaired or replaced during infancy, childhood, or even before birth. Other types may not cause problems until middle-age or older, if at all.
Heart conditions and other disorders, age-related changes, rheumatic fever, or infections can cause acquired heart valve disease. These factors change the shape or flexibility of once-normal valves.
The cause of congenital heart valve disease isn't known. It occurs before birth as the heart is forming. Congenital heart valve disease can occur alone or with other types of congenital heart defects.
Certain conditions can stretch and distort the heart valves, such as:
Men older than 65 and women older than 75 are prone to developing calcium and other types of deposits on their heart valves. These deposits stiffen and thicken the valve flaps and limit blood flow through the valve (stenosis).
The aortic valve is especially prone to this problem. The deposits look similar to the plaque deposits seen in people who have atherosclerosis. Some of the same processes may cause both atherosclerosis and heart valve disease.
Untreated strep throat or other infections with strep bacteria that progress to rheumatic fever can cause heart valve disease.
When the body tries to fight the strep infection, one or more heart valves may be damaged or scarred in the process. The aortic and mitral valves most often are affected. Symptoms of heart valve damage often don't appear until many years after recovery from rheumatic fever.
Today, most people who have strep infections are treated with antibiotics before rheumatic fever occurs. If you have strep throat, take all of the antibiotics your doctor prescribes, even if you feel better before the medicine is gone.
Heart valve disease caused by rheumatic fever mainly affects older adults who had strep infections before antibiotics were available. It also affects people from developing countries, where rheumatic fever is more common.
Common germs that enter the bloodstream and get carried to the heart can sometimes infect the inner surface of the heart, including the heart valves. This rare but serious infection is called infective endocarditis (EN-do-kar-DI-tis), or IE.
The germs can enter the bloodstream through needles, syringes, or other medical devices and through breaks in the skin or gums. Often, the body's defenses fight off the germs and no infection occurs. Sometimes these defenses fail, which leads to IE.
IE can develop in people who already have abnormal blood flow through a heart valve as the result of congenital or acquired heart valve disease. The abnormal blood flow causes blood clots to form on the surface of the valve. The blood clots make it easier for germs to attach to and infect the valve.
IE can worsen existing heart valve disease.
Many other conditions and factors are linked to heart valve disease. However, the role they play in causing heart valve disease often isn't clear.
Older age is a risk factor for heart valve disease. As you age, your heart valves thicken and become stiffer. Also, people are living longer now than in the past. As a result, heart valve disease has become an increasing problem.
People who have a history of infective endocarditis (IE), rheumatic fever, heart attack, or heart failure—or previous heart valve disease—also are at higher risk for heart valve disease. In addition, having risk factors for IE, such as intravenous drug use, increases the risk of heart valve disease.
You're also at higher risk for heart valve disease if you have risk factors for coronary heart disease. These risk factors include high blood cholesterol, high blood pressure, smoking, insulin resistance, diabetes, overweight or obesity, lack of physical activity, and a family history of early heart disease.
Some people are born with an aortic valve that has two flaps instead of three. Sometimes an aortic valve may have three flaps, but two flaps are fused together and act as one flap. This is called a bicuspid or bicommissural aortic valve. People who have this congenital condition are more likely to develop aortic heart valve disease.
The main sign of heart valve disease is an unusual heartbeat sound called a heart murmur. Your doctor can hear a heart murmur with a stethoscope.
However, many people have heart murmurs without having heart valve disease or any other heart problems. Others may have heart murmurs due to heart valve disease, but have no other signs or symptoms.
Heart valve disease often worsens over time, so signs and symptoms may occur years after a heart murmur is first heard. Many people who have heart valve disease don't have any symptoms until they're middle-aged or older.
Other common signs and symptoms of heart valve disease relate to heart failure, which heart valve disease can cause. These signs and symptoms include:
Heart valve disease can cause chest pain that may happen only when you exert yourself. You also may notice a fluttering, racing, or irregular heartbeat. Some types of heart valve disease, such as aortic or mitral valve stenosis, can cause dizziness or fainting.
Your primary care doctor may detect a heart murmur or other signs of heart valve disease. However, a cardiologist usually will diagnose the condition. A cardiologist is a doctor who specializes in diagnosing and treating heart problems.
To diagnose heart valve disease, your doctor will ask about your signs and symptoms. He or she also will do a physical exam and look at the results from tests and procedures.
Your doctor will listen to your heart with a stethoscope. He or she will want to find out whether you have a heart murmur that's likely caused by a heart valve problem.
Your doctor also will listen to your lungs as you breathe to check for fluid buildup. He or she will check for swollen ankles and other signs that your body is retaining water.
Echocardiography (echo) is the main test for diagnosing heart valve disease. But an EKG (electrocardiogram) or chest x ray commonly is used to reveal certain signs of the condition. If these signs are present, echo usually is done to confirm the diagnosis.
Your doctor also may recommend other tests and procedures if you're diagnosed with heart valve disease. For example, you may have cardiac catheterization, (KATH-eh-ter-ih-ZA-shun), stress testing, or cardiac MRI (magnetic resonance imaging). These tests and procedures help your doctor assess how severe your condition is so he or she can plan your treatment.
This simple test detects and records the heart's electrical activity. An EKG can detect an irregular heartbeat and signs of a previous heart attack. It also can show whether your heart chambers are enlarged.
An EKG usually is done in a doctor's office.
This test can show whether certain sections of your heart are enlarged, whether you have fluid in your lungs, or whether calcium deposits are present in your heart.
A chest x ray helps your doctor learn which type of valve defect you have, how severe it is, and whether you have any other heart problems.
Echo uses sound waves to create a moving picture of your heart as it beats. A device called a transducer is placed on the surface of your chest.
The transducer sends sound waves through your chest wall to your heart. Echoes from the sound waves are converted into pictures of your heart on a computer screen.
Echo can show:
Your doctor may recommend transesophageal (tranz-ih-sof-uh-JEE-ul) echo, or TEE, to get a better image of your heart.
During TEE, the transducer is attached to the end of a flexible tube. The tube is guided down your throat and into your esophagus (the passage leading from your mouth to your stomach). From there, your doctor can get detailed pictures of your heart.
You'll likely be given medicine to help you relax during this procedure.
For this procedure, a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. Your doctor uses x-ray images to guide the catheter.
Through the catheter, your doctor does diagnostic tests and imaging that show whether backflow is occurring through a valve and how fully the valve opens. You'll be given medicine to help you relax, but you will be awake during the procedure.
Your doctor may recommend cardiac catheterization if your signs and symptoms of heart valve disease aren't in line with your echo results.
The procedure also can help your doctor assess whether your symptoms are due to specific valve problems or coronary heart disease. All of this information helps your doctor decide the best way to treat you.
During stress testing, you exercise to make your heart work hard and beat fast while heart tests and imaging are done. If you can't exercise, you may be given medicine to raise your heart rate.
A stress test can show whether you have signs and symptoms of heart valve disease when your heart is working hard. It can help your doctor assess the severity of your heart valve disease.
Cardiac MRI uses a powerful magnet and radio waves to make detailed images of your heart. A cardiac MRI image can confirm information about valve defects or provide more detailed information.
This information can help your doctor plan your treatment. An MRI also may be done before heart valve surgery to help your surgeon plan for the surgery.
Currently, no medicines can cure heart valve disease. However, lifestyle changes and medicines often can successfully treat symptoms and delay problems for many years. Eventually, though, you may need surgery to repair or replace a faulty heart valve.
The goals of treating heart valve disease might include:
To relieve the symptoms of heart conditions related to heart valve disease, your doctor may advise you to quit smoking and follow a healthy diet.
A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
For more information about following a healthy diet, go to the National Heart, Lung, and Blood Institute's "Your Guide to Lowering Your Blood Pressure With DASH" and the U.S. Department of Agriculture's ChooseMyPlate.gov Web site. Both resources provide general information about healthy eating.
Your doctor may ask you to limit physical activities that make you short of breath and tired. He or she also may ask that you limit competitive athletic activity, even if the activity doesn't leave you unusually short of breath or tired.
Your doctor may prescribe medicines to:
If you've had previous heart valve disease and now have a man-made valve, you may be at risk for a heart infection called infective endocarditis (IE). This infection can worsen your heart valve disease.
One of the most common causes of IE is poor dental hygiene. To prevent this serious infection, floss and brush your teeth and regularly see a dentist. Gum infections and tooth decay can increase the risk of IE.
Let your doctors and dentists know if you have a man-made valve or if you've had IE before. They may give you antibiotics before dental procedures (such as dental cleanings) that could allow bacteria to enter your bloodstream. Talk to your doctor about whether you need to take antibiotics before such procedures.
Your doctor may recommend repairing or replacing your heart valve(s), even if your heart valve disease isn't causing symptoms. Repairing or replacing a valve can prevent lasting damage to your heart and sudden death.
Having heart valve repair or replacement depends on many factors, including:
When possible, heart valve repair is preferred over heart valve replacement. Valve repair preserves the strength and function of the heart muscle. People who have valve repair also have a lower risk of IE after the surgery, and they don't need to take blood-thinning medicines for the rest of their lives.
However, heart valve repair surgery is harder to do than valve replacement. Also, not all valves can be repaired. Mitral valves often can be repaired. Aortic and pulmonary valves often have to be replaced.
Heart surgeons can repair heart valves by:
Sometimes cardiologists repair heart valves using cardiac catheterization. Although catheter procedures are less invasive than surgery, they may not work as well for some patients.
Work with your doctor to decide whether repair is appropriate. If so, your doctor can advise you on the best procedure for doing it.
Balloon valvuloplasty. Heart valves that don't fully open (stenosis) can be repaired with surgery or with a less invasive catheter procedure called balloon valvuloplasty (VAL-vyu-lo-plas-tee). This procedure also is called balloon valvotomy (val-VOT-o-me).
During the procedure, a catheter (thin tube) with a balloon at its tip is threaded through a blood vessel to the faulty valve in your heart. The balloon is inflated to help widen the opening of the valve. Your doctor then deflates the balloon and removes both it and the tube.
You're awake during the procedure, which usually requires an overnight stay in a hospital.
Balloon valvuloplasty relieves many of the symptoms of heart valve disease, but it may not cure it. The condition can worsen over time. You still may need medicines to treat symptoms or surgery to repair or replace the faulty valve.
Balloon valvuloplasty has a shorter recovery time than surgery. The procedure may work as well as surgery for some patients who have mitral valve stenosis. Thus, for these people, balloon valvuloplasty often is preferred over surgical repair or replacement.
Balloon valvuloplasty doesn't work as well as surgery for adults who have aortic valve stenosis.
Doctors often use balloon valvuloplasty to repair valve stenosis in infants and children.
Sometimes heart valves can't be repaired and must be replaced. This surgery involves removing the faulty valve and replacing it with a man-made or biological valve.
Biological valves are made from pig, cow, or human heart tissue and may have man-made parts as well. These valves are specially treated, so you won't need medicines to stop your body from rejecting the valve.
Man-made valves last longer than biological valves and usually don't have to be replaced. Biological valves usually have to be replaced after about 10 years, although newer ones may last 15 years or longer.
Unlike biological valves, however, man-made valves require you to take blood-thinning medicines for the rest of your life. These medicines prevent blood clots from forming on the valve. Blood clots can cause a heart attack or stroke. Man-made valves also raise your risk of IE.
You and your doctor will decide together whether you should have a man-made or biological replacement valve.
If you're a woman of childbearing age or if you're athletic, you may prefer a biological valve so you don't have to take blood-thinning medicines. If you're elderly, you also may prefer a biological valve, as it will likely last for the rest of your life.
Some newer forms of heart valve repair and replacement surgery are less invasive than traditional surgery. These procedures use smaller incisions (cuts) to reach the heart valves. Hospital stays for these newer types of surgery usually are 3–5 days, compared with 5-day stays for traditional heart valve surgery.
New surgeries tend to cause less pain and have a lower risk of infection. Recovery time also tends to be shorter—2–4 weeks versus 6–8 weeks for traditional surgery.
Some cardiologists and surgeons are exploring catheter procedures that involve threading clips or other devices through blood vessels to faulty heart valves. The clips or devices are used to reshape the valves and stop the backflow of blood.
People who receive these clips recover more easily than people who have surgery. However, the clips may not treat backflow as well as surgery. Researchers are still studying this treatment method.
Doctor also may use catheters to replace faulty aortic valves. This procedure is called transcatheter aortic valve implantation (TAVI).
For this procedure, the catheter usually is inserted into an artery in the groin (upper thigh) and threaded to the heart. At the end of the catheter is a deflated balloon with a folded replacement valve around it.
Once the replacement valve is properly placed, the balloon is used to expand the new valve so it fits securely within the old valve. The balloon is then deflated, and the balloon and catheter are removed.
A replacement valve also can be inserted in an existing replacement valve that is failing. This is called a valve-in-valve procedure.
Catheter procedures may be an option for patients who have conditions that make open-heart surgery too risky. Only a few medical centers have experience with these fairly new procedures.
Doctors also treat faulty aortic valves with a procedure called the Ross operation. During this operation, your doctor removes your faulty aortic valve and replaces it with your pulmonary valve. Your pulmonary valve is then replaced with a pulmonary valve from a deceased human donor.
This is more involved surgery than typical valve replacement, and it has a greater risk of complications.
The Ross operation may be especially useful for children because the surgically replaced valves continue to grow with the child. Also, lifelong treatment with blood-thinning medicines isn't required.
But in some patients, one or both valves fail to work well within a few years of the surgery. Experts continue to debate and study the usefulness of this procedure.
Serious risks from all types of heart valve surgery vary according to your age, health, the type of valve defect(s) you have, and the surgical procedures used.
To prevent heart valve disease caused by rheumatic fever, see your doctor if you have signs of a strep infection. These signs include a painful sore throat, fever, and white spots on your tonsils.
If you do have a strep infection, be sure to take all medicines prescribed to treat it. Prompt treatment of strep infections can prevent rheumatic fever, which damages the heart valves.
It's possible that exercise, a healthy diet, and medicines that lower cholesterol might prevent aortic stenosis (thickening and stiffening of the aortic valve). Researchers continue to study this possibility.
A healthy diet, physical activity, other lifestyle changes, and medicines aimed at preventing a heart attack, high blood pressure, or heart failure also may help prevent heart valve disease.
If you've had previous heart valve disease and now have a man-made valve, you're at risk for a heart infection called infective endocarditis (IE).
One of the most common causes of IE is poor dental hygiene. Thus, to prevent this serious infection, floss and brush your teeth and regularly see a dentist. Gum infections and tooth decay can increase the risk of IE.
Let your doctors and dentists know if you have a man-made valve or if you've had IE before. They may give you antibiotics before dental procedures (such as dental cleanings) that could allow bacteria to enter your bloodstream. Talk to your doctor about whether you need to take antibiotics before such procedures.
Heart valve disease is a lifelong condition. However, many people have heart valve defects or disease but don't have symptoms. For some people, the condition mostly stays the same throughout their lives and doesn't cause any problems.
For other people, the condition slowly worsens until symptoms develop. If not treated, advanced heart valve disease can cause heart failure or other life-threatening conditions.
Eventually, you may need to have your faulty heart valve(s) repaired or replaced. After repair or replacement, you'll still need certain medicines and regular checkups with your doctor.
If you have heart valve disease, see your doctor regularly for checkups and for echocardiography or other tests. This will allow your doctor to check the progress of your heart valve disease.
Call your doctor if your symptoms worsen or you have new symptoms. Also, discuss with your doctor whether lifestyle changes might benefit you. Ask him or her which types of physical activity are safe for you.
Call your doctor if you have symptoms of infective endocarditis (IE). Symptoms of this heart infection include fever, chills, muscle aches, night sweats, problems breathing, fatigue (tiredness), weakness, red spots on the palms and soles, and swelling of the feet, legs, and belly.
Let your doctors and dentists know if you have a man-made valve or if you've had IE before. They may give you antibiotics before dental procedures (such as dental cleanings) that could allow bacteria to enter your bloodstream. Talk to your doctor about whether you need to take antibiotics before such procedures.
Take all of your medicines as prescribed.
Mild or moderate heart valve disease during pregnancy usually can be managed with medicines or bed rest. With proper care, the disease usually won't pose heightened risks to the mother or fetus.
Doctors can treat most heart valve conditions with medicines that are safe to take during pregnancy. Your doctor can advise you on which medicines are safe for you.
Severe heart valve disease can make pregnancy or labor and delivery risky. If you have severe heart valve disease, consider having your heart valves repaired or replaced before getting pregnant. This treatment also can be done during pregnancy, if needed. However, this surgery poses danger to both the mother and fetus.
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has uncovered some of the causes of heart diseases and conditions, as well as ways to prevent or treat them.
Many more questions remain about heart diseases and conditions, including heart valve disease. Thus, the NHLBI continues to support research to learn more. For example, NHLBI-supported research on heart valve disease includes studies that explore:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart valve disease, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Source: NHLBI, NIH
What Is Heart Surgery?
Heart surgery is done to correct problems with the heart. Many heart surgeries are done each year in the United States for various heart problems.
Heart surgery is used for both children and adults. This article discusses heart surgery for adults. For more information about heart surgery for children, go to the Health Topics articles about congenital heart defects, holes in the heart, and tetralogy of Fallot.
The most common type of heart surgery for adults is coronary artery bypass grafting (CABG). During CABG, a healthy artery or vein from the body is connected, or grafted, to a blocked coronary (heart) artery.
The grafted artery or vein bypasses (that is, goes around) the blocked portion of the coronary artery. This creates a new path for oxygen-rich blood to flow to the heart muscle. CABG can relieve chest pain and may lower your risk of having a heart attack.
Doctors also use heart surgery to:
Traditional heart surgery, often called open-heart surgery, is done by opening the chest wall to operate on the heart. The surgeon cuts through the patient's breastbone (or just the upper part of it) to open the chest.
Once the heart is exposed, the patient is connected to a heart-lung bypass machine. The machine takes over the heart's pumping action and moves blood away from the heart. This allows the surgeon to operate on a heart that isn't beating and that doesn't have blood flowing through it.
Another type of heart surgery is called off-pump, or beating heart, surgery. It's like traditional open-heart surgery because the chest bone is opened to access the heart. However, the heart isn't stopped, and a heart-lung bypass machine isn't used. Off-pump heart surgery is limited to CABG.
Surgeons can now make small incisions (cuts) between the ribs to do some types of heart surgery. The breastbone is not opened to reach the heart. This is called minimally invasive heart surgery. This type of heart surgery may or may not use a heart-lung bypass machine.
Newer methods of heart surgery (such as off-pump and minimally invasive) may reduce risks and speed up recovery time. Studies are under way to compare these types of heart surgery with traditional open-heart surgery.
The results of these studies will help doctors decide the best surgery to use for each patient.
The results of heart surgery in adults often are excellent. Heart surgery can reduce symptoms, improve quality of life, and improve the chances of survival.
To understand heart surgery, it's helpful to know how a normal heart works. Go to the Health Topics article on How the Heart Works for more information.
Coronary artery bypass grafting (CABG) is the most common type of heart surgery. CABG improves blood flow to the heart. Surgeons use CABG to treat people who have severe coronary heart disease (CHD).
CHD is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause chest pain or discomfort called angina (an-JI-nuh or AN-juh-nuh).
If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. This is the most common cause of a heart attack. Over time, ruptured plaque also hardens and narrows the coronary arteries.
During CABG, a healthy artery or vein from the body is connected, or grafted, to the blocked coronary artery. The grafted artery or vein bypasses (that is, goes around) the blocked portion of the coronary artery. This creates a new path for oxygen-rich blood to flow to the heart muscle.
Surgeons can bypass multiple blocked coronary arteries during one surgery.
Figure A shows the location of the heart. Figure B shows how vein and artery bypass grafts are attached to the heart.
CABG isn't the only treatment for CHD. A nonsurgical procedure that opens blocked or narrow coronary arteries is percutaneous (per-ku-TA-ne-us) coronary intervention (PCI), sometimes referred to as angioplasty (AN-jee-oh-plas-tee).
During PCI, a thin, flexible tube with a balloon at its tip is threaded through a blood vessel to the narrow or blocked coronary artery. Once in place, the balloon is inflated to push the plaque against the artery wall. This restores blood flow through the artery.
During PCI, a stent might be placed in the coronary artery to help keep it open. A stent is a small mesh tube that supports the inner artery wall.
If both CABG and PCI are options, your doctor can help you decide which treatment is right for you.
Transmyocardial (tranz-mi-o-KAR-de-al) laser revascularization (re-VAS-kyu-lar-ih-ZA-shun), or TMR, is surgery used to treat angina.
TMR is most often used when no other treatments work. For example, if you've already had one CABG procedure and can't have another one, TMR might be an option. For some people, TMR is combined with CABG.
If TMR is done alone, the procedure may be performed through a small opening in the chest.
During TMR, a surgeon uses lasers to make small channels through the heart muscle and into the heart's lower left chamber (the left ventricle).
It isn't fully known how TMR relieves angina. The surgery may help the heart grow tiny new blood vessels. Oxygen-rich blood may flow through these vessels into the heart muscle, which could relieve angina.
For the heart to work well, blood must flow in only one direction. The heart's valves make this possible. Healthy valves open and close in a precise way as the heart pumps blood.
Each valve has a set of flaps called leaflets. The leaflets open to allow blood to pass from one heart chamber into another or into the arteries. Then the leaflets close tightly to stop blood from flowing backward.
Heart surgery is used to fix leaflets that don't open as wide as they should. This can happen if they become thick or stiff or fuse together. As a result, not enough blood flows through the valve.
Heart surgery also is used to fix leaflets that don't close tightly. This problem can cause blood to leak back into the heart chambers, rather than only moving forward into the arteries as it should.
To fix these problems, surgeons either repair the valve or replace it with a man-made or biological valve. Biological valves are made from pig, cow, or human heart tissue and may have man-made parts as well.
To repair a mitral (MI-trul) or pulmonary (PULL-mun-ary) valve that's too narrow, a cardiologist (heart specialist) will insert a catheter (a thin, flexible tube) through a large blood vessel and guide it to the heart.
The cardiologist will place the end of the catheter inside the narrow valve. He or she will inflate and deflate a small balloon at the tip of the catheter. This widens the valve, allowing more blood to flow through it. This approach is less invasive than open-heart surgery.
Researchers also are testing new ways to use catheters in other types of valve surgeries. For example, catheters might be used to place clips on the mitral valve leaflets to hold them in place.
Catheters also might be used to replace faulty aortic valves. For this procedure, the catheter usually is inserted into an artery in the groin (upper thigh) and threaded to the heart.
In some cases, surgeons might make a small cut in the chest and left ventricle (the lower left heart chamber). They will thread the catheter into the heart through the small opening.
The catheter has a deflated balloon at its tip with a folded replacement valve around it. The balloon is used to expand the new valve so it fits securely within the old valve.
Currently, surgery to replace the valve is the traditional treatment for reasonably healthy people. However, catheter procedures might be a safer option for patients who have conditions that make open-heart surgery very risky.
An arrhythmia (ah-RITH-me-ah) is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
Many arrhythmias are harmless, but some can be serious or even life threatening. If the heart rate is abnormal, the heart may not be able to pump enough blood to the body. Lack of blood flow can damage the brain, heart, and other organs.
Medicine usually is the first line of treatment for arrhythmias. If medicine doesn't work well, your doctor may recommend surgery. For example, surgery may be used to implant a pacemaker or an implantable cardioverter defibrillator (ICD).
A pacemaker is a small device that's placed under the skin of your chest or abdomen. Wires connect the pacemaker to your heart chambers. The device uses low-energy electrical pulses to control your heart rhythm. Most pacemakers have a sensor that starts the device only if your heart rhythm is abnormal.
An ICD is another small device that's placed under the skin of your chest or abdomen. This device also is connected to your heart with wires. An ICD checks your heartbeat for dangerous arrhythmias. If the device senses one, it sends an electric shock to your heart to restore a normal heart rhythm.
Another arrhythmia treatment is called maze surgery. For this surgery, the surgeon makes new paths for the heart's electrical signals to travel through. This type of surgery is used to treat atrial fibrillation, the most common type of serious arrhythmia.
Simpler, less invasive procedures also are used to treat atrial fibrillation. These procedures use high heat or intense cold to prevent abnormal electrical signals from moving through the heart.
An aneurysm (AN-u-rism) is a balloon-like bulge in the wall of an artery or the heart muscle. This bulge can occur if the artery wall weakens. Pressure from blood moving through the artery or heart causes the weak area to bulge.
Over time, an aneurysm can grow and burst, causing dangerous, often fatal bleeding inside the body. Aneurysms also can develop a split in one or more layers of the artery wall. The split causes bleeding into and along the layers of the artery wall.
Aneurysms in the heart most often occur in the heart's lower left chamber (the left ventricle). Repairing an aneurysm involves surgery to replace the weak section of the artery or heart wall with a patch or graft.
A heart transplant is surgery to remove a person's diseased heart and replace it with a healthy heart from a deceased donor. Most heart transplants are done on patients who have end-stage heart failure.
Heart failure is a condition in which the heart is damaged or weak. As a result, it can't pump enough blood to meet the body's needs. "End-stage" means the condition is so severe that all treatments, other than heart transplant, have failed.
Patients on the waiting list for a donor heart receive ongoing treatment for heart failure and other medical conditions. Ventricular assist devices (VADs) or total artificial hearts (TAHs) might be used to treat these patients.
A VAD is a mechanical pump that is used to support heart function and blood flow in people who have weak hearts.
Your doctor may recommend a VAD if you have heart failure that isn't responding to treatment or if you're waiting for a heart transplant. You can use a VAD for a short time or for months or years, depending on your situation.
A TAH is a device that replaces the two lower chambers of the heart (the ventricles). You may benefit from a TAH if both of your ventricles don't work well due to end-stage heart failure.
Placing either device requires open-heart surgery.
Surgeons can use different approaches to operate on the heart, including open-heart surgery, off-pump heart surgery, and minimally invasive heart surgery.
The surgical approach will depend on the patient's heart problem, general health, and other factors.
Open-heart surgery is any kind of surgery in which a surgeon makes a large incision (cut) in the chest to open the rib cage and operate on the heart. "Open" refers to the chest, not the heart. Depending on the type of surgery, the surgeon also may open the heart.
Once the heart is exposed, the patient is connected to a heart-lung bypass machine. The machine takes over the heart's pumping action and moves blood away from the heart. This allows the surgeon to operate on a heart that isn't beating and that doesn't have blood flowing through it.
Open-heart surgery is used to do CABG, repair or replace heart valves, treat atrial fibrillation, do heart transplants, and place VADs and TAHs.
Surgeons also use off-pump, or beating heart, surgery to do CABG. This approach is like traditional open-heart surgery because the chest bone is opened to access the heart. However, the heart isn't stopped, and a heart-lung bypass machine isn't used.
Off-pump heart surgery isn't right for all patients. Work with your doctor to decide whether this type of surgery is an option for you. Your doctor will carefully consider your heart problem, age, overall health, and other factors that may affect the surgery.
For minimally invasive heart surgery, a surgeon makes small incisions (cuts) in the side of the chest between the ribs. This type of surgery may or may not use a heart-lung bypass machine.
Minimally invasive heart surgery is used to do some bypass and maze surgeries. It's also used to repair or replace heart valves, insert pacemakers or ICDs, or take a vein or artery from the body to use as a bypass graft for CABG.
One type of minimally invasive heart surgery that is becoming more common is robotic-assisted surgery. For this surgery, a surgeon uses a computer to control surgical tools on thin robotic arms.
The tools are inserted through small incisions in the chest. This allows the surgeon to do complex and highly precise surgery. The surgeon always is in total control of the robotic arms; they don't move on their own.
Heart surgery is used to treat many heart problems. For example, it's used to:
If other treatments—such as lifestyle changes, medicines, and medical procedures—haven't worked or can't be used, heart surgery might be an option.
Your primary care doctor, a cardiologist, and a cardiothoracic (KAR-de-o-tho-RAS-ik) surgeon will work with you to decide whether you need heart surgery.
A cardiologist specializes in diagnosing and treating heart problems. A cardiothoracic surgeon specializes in surgery on the heart and lungs.
These doctors will talk with you and do tests to learn about your general health and your heart problem. They'll discuss the test results with you and help you make decisions about the surgery.
Your doctors will talk with you about:
You also may have blood tests, such as a complete blood count, a lipoprotein panel (cholesterol test), and other tests as needed.
Tests are done to find out more about your heart problem and your general health. This helps your doctors decide whether you need heart surgery, what type of surgery you need, and when to do it.
An EKG is a painless, noninvasive test that records the heart's electrical activity. "Noninvasive" means that no surgery is done and no instruments are inserted into your body.
The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage due to CHD and signs of a previous or current heart attack.
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise to make your heart work hard and beat fast. If you can't exercise, you may be given medicine to raise your heart rate.
As part of the test, your blood pressure is checked and an EKG is done. Other heart tests also might be done.
Echocardiography (echo) is a painless, noninvasive test. This test uses sound waves to create a moving picture of your heart. Echocardiography shows the size and shape of your heart and how well your heart chambers and valves are working.
The test also can show areas of poor blood flow to your heart, areas of heart muscle that aren't working well, and previous injury to your heart muscle caused by poor blood flow.
Coronary angiography (an-jee-OG-rah-fee) is a test that uses dye and special x rays to show the insides of your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-eh-ter-ih-ZA-shun).
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through the coronary arteries. These
x rays are called angiograms.
The dye lets your doctor study blood flow through the heart and blood vessels. This helps your doctor find blockages that can cause a heart attack.
An aortogram is an angiogram of the aorta. The aorta is the main artery that carries blood from your heart to your body. An aortogram may show the location and size of an aortic aneurysm.
A chest x ray creates pictures of the structures inside your chest, such as your heart, lungs, and blood vessels.
This test gives your doctor information about the size and shape of your heart. A chest x ray also shows the position and shape of the large arteries around your heart.
A cardiac computed tomography (to-MOG-rah-fee) scan, or cardiac CT scan, is a painless test that uses an x-ray machine to take clear, detailed pictures of the heart.
Sometimes an iodine-based dye (contrast dye) is injected into one of your veins during the scan. The contrast dye highlights your coronary (heart) arteries on the x-ray pictures. This type of CT scan is called a coronary CT angiography, or CTA.
A cardiac CT scan can show whether plaque is narrowing your coronary arteries or whether you have an aneurysm. A CT scan also can find problems with the heart's function and valves.
Magnetic resonance imaging (MRI) is a safe, noninvasive test that uses magnets, radio waves, and a computer to create pictures of your organs and tissues.
Cardiac MRI creates images of your heart as it is beating. The computer makes both still and moving pictures of your heart and major blood vessels.
Cardiac MRI shows the structure and function of your heart. This test can show the size and location of an aneurysm.
There are many types of heart surgery. One person's experience before surgery can be very different from another's.
Some people carefully plan their surgeries with their doctors. They know exactly when and how their surgeries will happen. Other people need emergency heart surgery. For example, they might be diagnosed with blocked coronary arteries and admitted to the hospital right away for surgery.
If you're having a planned surgery, your doctors and others on your health care team will meet with you to explain what will happen. They'll tell you how to prepare for the surgery. You might be admitted to the hospital the afternoon or morning before your surgery.
You may have some tests before the surgery, such as an EKG (electrocardiogram), chest x ray, or blood tests. An intravenous (IV) line will be placed into a blood vessel in your arm or chest to give you fluids and medicines.
A member of your health care team may shave the area where your surgeon will make the incision (cut). Also, your skin might be washed with special soap to reduce the risk of infection.
Just before the surgery, you'll be moved to the operating room. You'll be given medicine so that you fall asleep and don't feel pain during the surgery.
Heart surgery is done in a hospital, and a team of experts is involved. Cardiothoracic surgeons perform the surgery with other doctors and nurses who help.
How long the surgery takes will depend on the type of surgery you're having. CABG, the most common type of heart surgery, takes about 3–6 hours.
For this type of surgery, you'll be given medicine to help you fall asleep. A doctor will check your heartbeat, blood pressure, oxygen levels, and breathing during the surgery.
A breathing tube will be placed in your lungs through your throat. The tube will connect to a ventilator (a machine that supports breathing).
Your surgeon will make a 6- to 8-inch incision (cut) down the center of your chest wall. Then, he or she will cut your breastbone and open your rib cage to reach your heart.
During the surgery, you'll receive medicine to thin your blood and keep it from clotting. A heart-lung bypass machine will be connected to your heart. The machine will take over your heart's pumping action and move blood away from your heart.
A specialist will oversee the heart-lung bypass machine. The machine will allow the surgeon to operate on a heart that isn't beating and that doesn't have blood flowing through it.
The image shows how a heart-lung bypass machine works during surgery.
You'll be given medicine to stop your heartbeat once you're connected to the heart-lung bypass machine. A tube will be placed in your heart to drain blood to the machine.
The machine will remove carbon dioxide (a waste product) from your blood, add oxygen to your blood, and then pump the blood back into your body. Your surgeon will insert tubes into your chest to drain fluid.
Once the bypass machine starts to work, the surgeon will repair your heart problem. After the surgery is done, he or she will restore blood flow to your heart. Usually, your heart will start beating again on its own. Sometimes mild electric shocks are used to restart the heart.
Once your heart has started beating again, your surgeon will remove the tubes and stop the heart-lung bypass machine. You'll be given medicine to allow your blood to clot again.
The surgeon will use wires to close your breastbone. The wires will stay in your body permanently. After your breastbone heals, it will be as strong as it was before the surgery.
Stitches or staples will be used to close the skin incision. Your breathing tube will be removed when you're able to breathe without it.
Off-pump heart surgery is like traditional open-heart surgery because the chest bone is opened to access the heart. However, the heart isn't stopped, and a heart-lung bypass machine isn't used.
Instead, your surgeon will steady your heart with a mechanical device so he or she can work on it. Your heart will continue to pump blood to your body.
For this type of heart surgery, your surgeon will make small incisions in the side of your chest between the ribs. These cuts can be as small as 2–3 inches. The surgeon will insert surgical tools through these small cuts.
A tool with a small video camera at the tip also will be inserted through an incision. This tool will allow the surgeon to see inside your body.
Some types of minimally invasive heart surgery use a heart-lung bypass machine and others don't.
You may spend a day or more in the hospital's intensive care unit (ICU), depending on the type of heart surgery you have. An intravenous (IV) needle might be inserted in a blood vessel in your arm or chest to give you fluids until you're ready to drink on your own.
Your health care team may give you extra oxygen through a face mask or nasal prongs that fit just inside your nose. They will remove the mask or prongs when you no longer need them.
When you leave the ICU, you'll be moved to another part of the hospital for several days before you go home. While you're in the hospital, doctors and nurses will closely watch your heart rate, blood pressure, breathing, and incision site(s).
People respond differently to heart surgery. Your recovery at home will depend on what kind of heart problem and surgery you had. Your doctor will tell you how to:
You also will get information about followup appointments, medicines, and situations when you should call your doctor right away.
After-effects of heart surgery are normal. They may include muscle pain, chest pain, or swelling (especially if you have an incision in your leg from coronary artery bypass grafting, or CABG).
Other after-effects may include loss of appetite, problems sleeping, constipation, and mood swings and depression. After-effects usually go away over time.
Recovery time after heart surgery depends on the type of surgery you had, your overall health before the surgery, and any complications from the surgery.
Your doctor will let you know when you can go back to your daily routine, such as working, driving, and physical activity.
Ongoing care after your surgery will include checkups with your doctor. During these visits, you may have blood tests, an EKG (electrocardiogram), echocardiography, or a stress test. These tests will show how your heart is working after the surgery.
After some types of heart surgery, you'll need to take a blood-thinning medicine. Your doctor will do routine tests to make sure you're getting the right amount of medicine.
Your doctor also may recommend lifestyle changes and medicines to help you stay healthy. Lifestyle changes may include quitting smoking, changing your diet, being physically active, and reducing and managing stress.
Your doctor also may refer you to cardiac rehabilitation (rehab). Cardiac rehab is a medically supervised program that helps improve the health and well-being of people who have heart problems.
Cardiac rehab includes exercise training, education on heart healthy living, and counseling to reduce stress and help you recover. Your doctor can tell you where to find a cardiac rehab program near your home.
Heart surgery has risks, even though its results often are excellent. Risks include:
Memory loss and other issues, such as problems concentrating or thinking clearly, may occur in some people.
These problems are more likely to affect older patients and women. These issues often improve within 6–12 months of surgery.
In general, the risk of complications is higher if heart surgery is done in an emergency situation (for example, during a heart attack). The risk also is higher if you have other diseases or conditions, such as diabetes, kidney disease, lung disease, or peripheral arterial disease (P.A.D.).
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has evaluated various treatments for heart problems, including heart surgery.
The NHLBI continues to support research on heart surgery. For example, the NHLBI is involved in studies that:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart surgery, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Source: NHLBI, NIH
A heart transplant is surgery to remove a person's diseased heart and replace it with a healthy heart from a deceased donor. Most heart transplants are done on patients who have end-stage heart failure.
Heart failure is a condition in which the heart is damaged or weak. As a result, it can't pump enough blood to meet the body's needs. "End-stage" means the condition is so severe that all treatments, other than a heart transplant, have failed.
Heart transplants are done as a life-saving measure for end-stage heart failure.
Because donor hearts are in short supply, patients who need heart transplants go through a careful selection process. They must be sick enough to need a new heart, yet healthy enough to receive it.
Survival rates for people receiving heart transplants have improved, especially in the first year after the transplant.
About 88 percent of patients survive the first year after transplant surgery, and 75 percent survive for 5 years. The 10-year survival rate is about 56 percent.
After the surgery, most heart transplant patients can return to their normal levels of activity. However, less than 30 percent return to work for many different reasons.
The heart transplant process starts when doctors refer a patient who has end-stage heart failure to a heart transplant center.
Staff members at the center assess whether the patient is eligible for the surgery. If the patient is eligible, he or she is placed on a waiting list for a donor heart.
Heart transplant surgery is done in a hospital when a suitable donor heart is found. After the transplant, the patient is started on a lifelong health care plan. The plan involves multiple medicines and frequent medical checkups.
Most patients referred to heart transplant centers have end-stage heart failure. Their heart failure might have been caused by:
Most patients considered for heart transplants have tried other, less drastic treatments. They also have been hospitalized many times for heart failure.
The specialists at the heart transplant center will assess whether a patient is eligible for a transplant. Specialists often include a:
In general, patients selected for heart transplants have severe end-stage heart failure, but are healthy enough to have the transplant. Heart failure is considered “end stage” when all possible treatments—such as medicines, implanted devices, and surgery—have failed.
Certain conditions and factors make it less likely that a heart transplant will work well. Examples include:
Patients who have one or more of the above conditions might not be eligible for heart transplant surgery.
Patients who are eligible for a heart transplant are added to a waiting list for a donor heart. This waiting list is part of a national allocation system for donor organs. The Organ Procurement and Transplantation Network (OPTN) runs this system.
OPTN has policies in place to make sure donor hearts are given out fairly. These policies are based on urgency of need, available organs, and the location of the patient who is receiving the heart (the recipient).
Organs are matched for blood type and size of donor and recipient.
Guidelines for how a donor heart is selected require that the donor meet the legal requirement for brain death and that the correct consent forms are signed.
Guidelines suggest that the donor should be younger than 65 years old, have little or no history of heart disease or trauma to the chest, and not be exposed to hepatitis or HIV.
The guidelines recommend that the donor heart should not be without blood circulation for more than 4 hours.
About 3,000 people in the United States are on the waiting list for a heart transplant on any given day. About 2,000 donor hearts are available each year. Wait times vary from days to several months and will depend on a recipient's blood type and condition.
A person might be taken off the list for some time if he or she has a serious medical event, such as a stroke, infection, or kidney failure.
Time spent on the waiting list plays a part in who receives a donor heart. For example, if two patients have equal need, the one who has been waiting longer will likely get the first available donor heart.
Patients on the waiting list for a donor heart get ongoing treatment for heart failure and other medical conditions.
For example, doctors may treat them for arrhythmias (irregular heartbeats). Arrhythmias can cause sudden cardiac arrest in people who have heart failure.
The doctors at the transplant centers may place implantable cardioverter defibrillators (ICDs) in patients before surgery. ICDs are small devices that are placed in the chest or abdomen. They help control life-threatening arrhythmias.
Another possible treatment for waiting list patients is a ventricular assist device (VAD). A VAD is a mechanical pump that helps support heart function and blood flow.
Routine outpatient care for waiting list patients may include frequent exercise testing, testing the strength of the heartbeat, and right cardiac catheterization (a test to measure blood pressure in the right side of the heart).
You also might start a cardiac rehabilitation (rehab) program. Cardiac rehab is a medically supervised program that helps improve the health and well-being of people who have heart problems.
The program can help improve your physical condition before the transplant. Also, you will learn the types of exercises used in the program, which will help you take part in cardiac rehab after the transplant.
Patients on the waiting list often are in close contact with their transplant centers. Most donor hearts must be transplanted within 4 hours after removal from the donor.
At some heart transplant centers, patients get a pager so the center can contact them at any time. They're asked to tell the transplant center staff if they're going out of town. Patients often need to be prepared to arrive at the hospital within 2 hours of being notified about a donor heart.
Not all patients who are called to the hospital will get a heart transplant. Sometimes, at the last minute, doctors find that a donor heart isn't suitable for a patient. Other times, patients from the waiting list are called to come in as possible backups, in case something happens with the selected recipient.
Just before heart transplant surgery, the patient will get general anesthesia (AN-es-THE-ze-ah). The term "anesthesia" refers to a loss of feeling and awareness. General anesthesia temporarily puts you to sleep.
Surgeons use open-heart surgery to do heart transplants. The surgeon will make a large incision (cut) in the patient’s chest to open the rib cage and operate on the heart.
A heart-lung bypass machine is hooked up to the heart’s arteries and veins. The machine pumps blood through the patient's lungs and body during the surgery.
The surgeon removes the patient’s diseased heart and sews the healthy donor heart into place. The patient’s aorta and pulmonary arteries are not replaced as part of the surgery.
Heart transplant surgery usually takes about 4 hours. Patients often spend the first days after surgery in the intensive care unit of the hospital.
The amount of time a heart transplant recipient spends in the hospital varies. Recovery often involves 1 to 2 weeks in the hospital and 3 months of monitoring by the transplant team at the heart transplant center.
Monitoring may include frequent blood tests, lung function tests, EKGs (electrocardiograms), echocardiograms, and biopsies of the heart tissue.
A heart biopsy is a standard test that can show whether your body is rejecting the new heart. This test is often done in the weeks after a transplant.
During a heart biopsy, a tiny grabbing device is inserted into a vein in the neck or groin (upper thigh). The device is threaded through the vein to the right atrium of the new heart to take a small tissue sample. The tissue sample is checked for signs of rejection.
While in the hospital, your health care team may suggest that you start a cardiac rehabilitation (rehab) program. Cardiac rehab is a medically supervised program that helps improve the health and well-being of people who have heart problems.
Cardiac rehab includes counseling, education, and exercise training to help you recover. Rehab may start with a member of the rehab team helping you sit up in a chair or take a few steps. Over time, you'll increase your activity level.
Your body will regard your new heart as a foreign object. You’ll need medicine to prevent your immune system from attacking the heart.
You and the transplant team will work together to protect the new heart. You’ll watch for signs and symptoms that your body is rejecting the organ. These signs and symptoms include:
You and the team also will work together to manage the transplant medicines and their side effects, prevent infections, and continue treatment of ongoing medical conditions.
Your doctors may ask you to check your temperature, blood pressure, and pulse when you go home.
You'll need to take medicine to suppress your immune system so that it doesn't reject the new heart. These medicines are called immunosuppressants.
Immunosuppressants are a combination of medicines that are tailored to your situation. Often, they include cyclosporine, tacrolimus, MMF (mycophenolate mofetil), and steroids (such as prednisone).
Your doctors may need to change or adjust your transplant medicines if they aren't working well or if you have too many side effects.
You'll have to manage multiple medicines after having a heart transplant. It's helpful to set up a routine for taking medicines at the same time each day and for refilling prescriptions. It's crucial to never run out of medicine. Always using the same pharmacy may help.
Keep a list of all your medicines with you at all times in case of an accident. When traveling, keep extra doses of medicine with you (not packed in your luggage). Bring your medicines with you to all doctor visits.
Side effects from medicines can be serious. Side effects include risk of infection, diabetes, osteoporosis (thinning of the bones), high blood pressure, kidney disease, and cancer—especially lymphoma and skin cancer.
Discuss any side effects of the medicines with your transplant team. Your doctors may change or adjust your medicines if you're having problems. Make sure your doctors know all of the medicines you're taking.
Some transplant medicines can increase your risk of infection. You may be asked to watch for signs of infection, including fever, sore throat, cold sores, and flu-like symptoms.
Signs of possible chest or lung infections include shortness of breath, cough, and a change in the color of sputum (spit).
Watching closely for these signs is important because transplant medicines can sometimes mask them. Also, pay close attention to signs of infection at the site of your incision (cut). These signs can include redness, swelling, or drainage.
Ask your doctor what steps you should take to reduce your risk of infection. For example, your doctor may suggest that you avoid contact with animals or crowds of people in the first few months after your transplant.
Regular dental care also is important. Your doctor or dentist may prescribe antibiotics before any dental work to prevent infections.
Many successful pregnancies have occurred after heart transplant surgeries; however, special care is needed. If you've had a heart transplant, talk with your doctor before planning a pregnancy.
Having a heart transplant may cause fear, anxiety, and stress. While you're waiting for a heart transplant, you may worry that you won't live long enough to get a new heart. After surgery, you may feel overwhelmed, depressed, or worried about complications.
All of these feelings are normal for someone going through major heart surgery. Talk about how you feel with your health care team. Talking to a professional counselor also can help.
If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to life after a heart transplant. You can see how other people who have had the surgery have coped with it. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Although heart transplant surgery is a life-saving measure, it has many risks. Careful monitoring, treatment, and regular medical care can prevent or help manage some of these risks.
The risks of having a heart transplant include:
Over time, the new heart may fail due to the same reasons that caused the original heart to fail. Failure of the donor heart also can occur if your body rejects the donor heart or if cardiac allograft vasculopathy (CAV) develops. CAV is a blood vessel disease.
Patients who have a heart transplant that fails can be considered for another transplant (called a retransplant).
The most frequent cause of death in the first 30 days after transplant is primary graft dysfunction. This occurs if the new donor heart fails and isn't able to function.
Factors such as shock or trauma to the donor heart or narrow blood vessels in the recipient's lungs can cause primary graft dysfunction. Doctors may prescribe medicines (for example, inhaled nitric oxide and intravenous nitrates) to treat this condition.
Rejection is one of the leading causes of death in the first year after transplant. The recipient's immune system sees the new heart as a foreign object and attacks it.
During the first year, heart transplant patients have an average of one to three episodes of rejection. Rejection is most likely to occur within 6 months of the transplant surgery.
CAV is a chronic (ongoing) disease in which the walls of the coronary arteries in the new heart become thick, hard, and less stretchy. CAV can destroy blood circulation in the new heart and cause serious damage.
CAV is a leading cause of donor heart failure and death in the years following transplant surgery. CAV can cause heart attack, heart failure, dangerous arrhythmias, and sudden cardiac arrest.
To detect CAV, your doctor may recommend coronary angiography yearly and other tests, such as stress echocardiography or intravascular ultrasound.
Taking daily medicines that stop the immune system from attacking the new heart is crucial, even though the medicines have serious side effects.
Cyclosporine and other medicines can cause kidney damage. Kidney damage affects more than 25 percent of patients in the first year after transplant.
When the immune system—the body's defense system—is suppressed, the risk of infection increases. Infection is a major cause of hospital admission for heart transplant patients. It also is a leading cause of death in the first year after transplant.
Suppressing the immune system leaves patients at risk for cancers and malignancies. Malignancies are a major cause of late death in heart transplant patients.
The most common malignancies are tumors of the skin and lips (patients at highest risk are older, male, and fair-skinned) and malignancies in the lymph system, such as non-Hodgkin's lymphoma.
High blood pressure develops in more than 70 percent of heart transplant patients in the first year after transplant and in nearly 95 percent of patients within 5 years.
High levels of cholesterol and triglycerides in the blood develop in more than 50 percent of heart transplant patients in the first year after transplant and in 84 percent of patients within 5 years.
Osteoporosis can develop or worsen in heart transplant patients. This condition thins and weakens the bones.
Not following a lifelong care plan increases the risk of all heart transplant complications. Heart transplant patients are asked to closely follow their doctors' instructions and check their own health status throughout their lives.
Lifelong health care includes taking multiple medicines on a strict schedule, watching for signs and symptoms of complications, going to all medical checkups, and making healthy lifestyle changes (such as quitting smoking).
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. For example, this research has helped evaluate many treatments for heart problems.
The NHLBI continues to support research on various heart treatments, including heart transplants. For example, NHLBI-sponsored research includes studies that explore:
Much of this research depends on the willingness of volunteers to take part in clinical trials. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions.
For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they’re widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don’t directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You’ll learn about treatments and tests you may receive, and the benefits and risks they may pose. You’ll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you’ll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to heart transplant surgery, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
For more information about clinical trials for children, visit the NHLBI’s Children and Clinical Studies Web page.
Source: NHLBI, NIH
Heart Health Tools
You have tremendous power to prevent heart disease—and you can start today. By learning your own personal risk factors and by making healthful lifestyle changes such as improving your diet or increasing your physical activity, you can greatly reduce your risk of developing heart-related problems. Even if you already have heart disease, you can take steps to lessen its severity. Use the many tools and resources in the sections listed below to find out how to lower your risk of heart disease.
Source: NHLBI, NIH