Cold, flu, and allergy all affect your respiratory system, which can make it hard to breathe. Each condition has key symptoms that set them apart. Colds and flu are caused by different viruses. “As a rule of thumb, the symptoms associated with the flu are more severe,” says Hauguel.
Flu, Cold, Allergies, and Sinus Infection
Source: Centers for Disease Control and Prevention
Flu (Seasonal Influenza)
Each year in the United States, seasonal influenza kills more than 36,000 people and hospitalizes 200,000 more. NIAID scientists worldwide are working together to find better ways to prevent, diagnose, and treat seasonal and pandemic influenza, including H1N1 flu
Overview
Influenza, or flu, is a respiratory infection caused by several flu viruses. Like the common cold, it infects the nose, throat, and lungs. Most people who get the flu get better within a week, although they may have a lingering cough and tire easily for a while longer. The best way to prevent the flu is by getting a flu vaccine every year.
Flu or Cold?
The flu differs in several ways from the common cold (PDF). For example, people with colds rarely get fevers or headaches or suffer from the extreme exhaustion that flu viruses cause. The most familiar aspect of the flu is the way it can "knock you off your feet" as it sweeps through entire communities.
The Centers for Disease Control and Prevention (CDC) estimates that 5 to 20 percent of Americans come down with the flu during each flu season, which typically lasts from October to March. Children are two to three times more likely than adults to get sick with the flu, and children frequently spread the virus to others.
For elderly people, newborn babies, pregnant women, and people with certain chronic illnesses, the flu and its complications can be life-threatening. Although most people recover from the illness, CDC estimates that between 3,000 and 49,000 Americans die from the flu and its complications every year.
Seasonal Flu
Seasonal flu refers to the flu outbreaks that occur each year, mainly in the late fall and winter. The disease spreads through communities, creating an epidemic. During the epidemic, the number of cases peaks in about three weeks and subsides after another three to four weeks.
Pandemic Flu
Pandemic flu refers to particularly contagious strains of flu that spread rapidly from person to person to create a worldwide epidemic (pandemic). In the past century, there were influenza pandemics in 1918, 1957, 1968, and 2009.
Cause
About the Flu Virus
Influenza, or flu, is a respiratory infection caused by any of several flu viruses, which are classified as type A, B, or C based on their nucleic acids and protein composition. Type A viruses are found in humans and many animals, including ducks, chickens, pigs, and whales. Type A influenza viruses caused the global flu outbreaks of 1918, 1957, 1968, and 2009. Type B viruses circulate widely in humans. Type C viruses are found in humans, pigs, and dogs and cause mild respiratory infections but do not spark epidemics.
The outer coat of the virus features two kinds of protein spikes: hemagglutinin (HA), which allows the virus to stick to a human or animal cell and initiate infection; and neuraminidase (NA), which enables newly formed viruses to exit the host cell. There are 16 HA subtypes and 9 NA subtypes among Type A viruses. Strains are named based on their combination of HA and NA proteins; for example, the virus that caused the 2009 H1N1 flu pandemic contained H1 and N1 surface proteins. Inside a flu virus are eight segments of single-stranded RNA containing the genetic instructions for making new copies of the virus.
Influenza A virus.
Credit: CDC
Where Influenza Comes From
In nature, the flu virus is found in wild aquatic birds, such as ducks and shore birds. It has persisted in these birds for millions of years and does not typically harm them. But the frequently mutating flu viruses can readily jump the species barrier from wild birds to domesticated poultry and swine.
Pigs can be infected by both bird (avian) flu and the form that infects humans. In a setting such as a farm where chickens, pigs, and humans live in close proximity, pigs act as an influenza virus mixing bowl. If a pig is infected with avian and human flu simultaneously, the two types of virus may exchange genes. Such a "reassorted" flu virus can sometimes spread from pigs to people. Depending on the combination of avian flu proteins that make it into the human population, the flu may be more or less severe.
In 1997, for the first time, scientists found that a form of avian H5N1 flu skipped the pig step and infected humans directly. Alarmed health officials feared a worldwide epidemic (a pandemic). But fortunately, the virus could not pass from person to person and thus did not spark an epidemic. As of August 2012, there have been 608 confirmed cases of this avian flu virus, which have resulted in 359 deaths.
Drifting and Shifting
Influenza virus is under constant evolutionary change. These genetic changes may be small and continuous or large and abrupt.
Small genetic changes happen continuously in Type A and Type B influenza as the virus makes copies of itself. This process is called antigenic drift. Drifting happens frequently enough to make new strains of virus unrecognizable to the human immune system. For this reason, a new flu vaccine must be produced each year to combat the strains circulating that year.
Type A influenza also undergoes infrequent and sudden changes known as antigenic shift. Antigenic shift occurs when two different flu strains infect the same cell and combine portions of their genetic material. The novel assortment of HA and/or NA proteins in a shifted virus may create a new influenza A subtype. Because people have little or no immunity to such a new subtype, the appearance of a new subtype usually coincides with a very severe flu epidemic or pandemic.
Transmission
How Flu Spreads
Coughing and Sneezing
People with flu can spread it to others up to about six feet away. Flu viruses spread mainly through tiny droplets made when people with flu cough, sneeze, or talk. These droplets can land in the mouths or noses of people who are nearby or be inhaled into the lungs.
A woman covers her nose and mouth when sneezing on an airplane.
Credit: iStockPhoto
Surfaces and Objects
People can also be exposed to flu by touching a surface or object that has flu virus on it and then touching their mouth, eyes, or nose. Studies have shown that human flu viruses generally can survive on surfaces between two and eight hours.
Hand washing with soap and warm water can help people avoid becoming infected by flu virus. If soap and water are not available, an alcohol-based hand rub may be substituted. Linens, eating utensils, and dishes used by people who are sick should not be shared without washing thoroughly first.
The Flu Is Contagious
You may be able to pass on the flu to someone else before you even know you are sick—as well as while you are sick. Most healthy adults can infect others beginning one day before symptoms develop and up to a week after becoming sick. Young children and people with weakened immune systems might be able to infect others for an even longer time. To avoid spreading the flu, the Centers for Disease Control and Prevention recommends that ill people stay home for at least 24 hours after fever is gone.
Symptoms and Complications
Influenza Symptoms
People who have the flu often experience
Fever
Feeling feverish/chills
Cough
Sore throat
Runny or stuffy nose
Muscle aches
Headaches
Fatigue (tiredness)
Vomiting and diarrhea (more common in children than adults)
Signs of Emergency
Certain symptoms of the flu may signal an emergency and should be assessed by a medical professional.
In children, these include
Fast breathing or trouble breathing
Bluish skin color
Not drinking enough fluids
Not waking up or not interacting
Irritability even when being held
Improvement of flu-like symptoms followed by return of symptoms with fever and worse cough
Fever with a rash
In infants, additional symptoms that could signal an emergency include
Being unable to eat
No tears when crying
Significantly fewer wet diapers than normal
In adults, watch out for
Difficulty breathing or shortness of breath
Pain or pressure in the chest or abdomen
Sudden dizziness
Confusion
Severe or persistent vomiting
Improvement of flu-like symptoms followed by return of symptoms with fever and worse cough
Severity of Flu
Flu is unpredictable. Its severity can vary widely from one season to the next depending on many factors, including
What flu viruses are spreading
How much flu vaccine is available
When the vaccine is available
How many people get vaccinated
How well the flu vaccine matches the flu viruses that are causing illness
One study found that during the 1990s, flu-related deaths in the United States ranged from an estimated 17,000 during the mildest season to 52,000 during the most severe season, averaging 36,000 per year. Over a period of 31 flu seasons between 1976 and 2007, estimates of flu-associated deaths in the United States ranged from a low of about 3,000 to a high of about 49,000 people. During a typical flu season, about 90 percent of deaths occur in people age 65 and older.
Complications From the Flu
Most people who get influenza will recover in less than two weeks, but some people will develop complications, some of which can be life-threatening or fatal. Complications can include bacterial pneumonia, ear or sinus infections, dehydration, and worsening of chronic medical conditions, such as congestive heart failure, asthma, or diabetes.
Complications usually appear after a person starts feeling better. After a brief period of improvement, the following symptoms may suddenly appear:
High fever
Shaking chills
Chest pain with each breath
Coughing that produces thick, yellow-greenish colored mucus
Reye's syndrome, a condition that affects the nerves, sometimes develops in children and teens who are recovering from the flu. Reye's syndrome begins with nausea and vomiting, but the progressive mental changes, such as confusion or delirium, cause the greatest concern.
The syndrome often begins in young people after they take aspirin to reduce fever or pain. Acetaminophen does not seem to be connected with Reye's syndrome.
Who Is at Risk?
Certain people are at greater risk for serious complications if they get the flu. These groups include
Children younger than 5, especially children younger than 2 years old
Newborn babies recently out of intensive care units
Adults age 65 or older
Pregnant women
American Indians and Alaska Natives
Those who are obese (Body Mass Index of 40 or greater)
People younger than age 19 who are receiving long-term aspirin therapy
People with certain medical conditions, including
Asthma, even if it's controlled or mild
Weakened immune function, including those with HIV/AIDS or cancer
Neurological conditions, including disorders of the brain, spinal cord, peripheral nerves, and muscle
Chronic lung disease, such as Chronic Obstructive Pulmonary Disease (COPD) and cystic fibrosis
Heart disease, such as congenital heart disease, congestive heart failure, and coronary artery disease
Blood disorders, such as sickle cell disease
Diabetes
Certain kidney, liver, and metabolic disorders
Diagnosis and Treatment
Most people with the flu recover on their own without medical care or antiviral drugs. People with mild cases of the flu should stay home and avoid contact with others, except to get medical care.
People who are at greater risk of serious flu-related complications—including young children, elderly people, pregnant women, and people with certain medical conditions—should contact a healthcare provider if flu symptoms develop.
Healthcare providers will determine whether a laboratory influenza test or treatments are needed. Antiviral drugs, which work best when started soon after flu symptoms appear, may also prevent serious complications.
Flu is usually diagnosed in a particular patient based on whether the disease is currently epidemic in the patient's community and whether the patient's complaints fit the current pattern of symptoms. During an epidemic, providers rarely use laboratory tests to identify the virus. Local, state, and national health officials, however, monitor certain U.S. health clinics and do laboratory tests to determine which type of flu virus is responsible for the epidemic.
Key Facts About Seasonal Flu Vaccine
Visit 2014-2015 Season: What You Should Know for flu and flu vaccine information specific to the current flu season.
The single best way to protect against the flu is to get vaccinated each year.
Flu Vaccination
Why should people get vaccinated against the flu?
Influenza is a serious disease that can lead to hospitalization and sometimes even death. Every flu season is different, and influenza infection can affect people differently. Even healthy people can get very sick from the flu and spread it to others. Over a period of 31 seasons between 1976 and 2007, estimates of flu-associated deaths in the United States range from a low of about 3,000 to a high of about 49,000 people. During a regular flu season, about 90 percent of deaths occur in people 65 years and older. “Flu season” in the United States can begin as early as October and last as late as May.
During this time, flu viruses are circulating at higher levels in the U.S. population. An annual seasonal flu vaccine (either the flu shot or the nasal spray flu vaccine) is the best way to reduce the chances that you will get seasonal flu and spread it to others. When more people get vaccinated against the flu, less flu can spread through that community.
How do flu vaccines work?
Flu vaccines cause antibodies to develop in the body about two weeks after vaccination. These antibodies provide protection against infection with the viruses that are in the vaccine.
The seasonal flu vaccine protects against the influenza viruses that research indicates will be most common during the upcoming season. Traditional flu vaccines (called trivalent vaccines) are made to protect against three flu viruses; an influenza A (H1N1) virus, an influenza A (H3N2) virus, and an influenza B virus. In addition, there are flu vaccines made to protect against four flu viruses (called “quadrivalent” vaccines). These vaccines protect against the same viruses as the trivalent vaccine and an additional B virus.
What kinds of flu vaccines are available?
There are several flu vaccine options for the 2014-2015 flu season.
Traditional flu vaccines made to protect against three different flu viruses (called “trivalent” vaccines) are available. In addition, flu vaccines made to protect against four different flu viruses (called “quadrivalent” vaccines) also are available.
Trivalent flu vaccine protects against two influenza A viruses (an H1N1 and an H3N2) and an influenza B virus. The following trivalent flu vaccines are available:
Standard-dose trivalent shots (IIV3) that are manufactured using virus grown in eggs. Different flu shots are approved for people of different ages, but there are flu shots that are approved for use in people as young as 6 months of age and up. (Most flu shots are given with a needle. One flu vaccine also can be given with a jet injector, for persons aged 18 through 64 years.)
An intradermal trivalent shot, which is injected into the skin instead of the muscle and uses a much smaller needle than the regular flu shot. It is approved for people 18 through 64 years of age.
A high-dose trivalent shot, approved for people 65 and older.
A trivalent shot containing virus grown in cell culture, which is approved for people 18 and older.
A recombinant trivalent shot that is egg-free, approved for people 18 years and older.
The quadrivalent flu vaccine protects against two influenza A viruses and two influenza B viruses. The following quadrivalent flu vaccines are available:
A quadrivalent flu shot.
A quadrivalent nasal spray vaccine, approved for people 2 through 49 years of age (recommended preferentially for healthy* children 2 years through 8 years old when immediately available and there are no contraindications or precautions).
(*“Healthy” in this instance refers to children 2 years through 8 years old who do not have an underlying medical condition that predisposes them to influenza complications.)
Are any of the available flu vaccines recommended over others?
CDC has not expressed a preference for which flu vaccine people should get this season except for one: Starting in 2014-2015, CDC recommends use of the nasal spray vaccine for healthy* children 2 years through 8 years of age when it is immediately available and if the child has no contraindications or precautions to that vaccine. If the nasal spray vaccine is not immediately available and the flu shot is, vaccination should not be delayed and a flu shot should be given. For more information about the new CDC recommendation, see Nasal Spray Flu Vaccine in Children 2 Years through 8 Years Old or the 2014-2015 MMWR Influenza Vaccine Recommendations.
While there will be more than one vaccine option for many people to choose from, including high-dose vaccine, intradermal vaccine and the regular flu shot, the only preferential recommendation is for the nasal spray vaccine in healthy* children 2 years through 8 years of age. The most important thing is for all people 6 months and older to get a flu vaccine every year. If you have questions about which vaccine is best for you, talk to your doctor or other health care professional.
(*“Healthy” in this instance refers to children 2 years through 8 years old who do not have an underlying medical condition that predisposes them to influenza complications.)
Who should get vaccinated this season?
Everyone 6 months of age and older should get a flu vaccine every season. This recommendation has been in place since February 24, 2010 when CDC’s Advisory Committee on Immunization Practices (ACIP) voted for “universal” flu vaccination in the United States to expand protection against the flu to more people.
Vaccination to prevent influenza is particularly important for people who are at high risk of serious complications from influenza. See People at High Risk of Developing Flu-Related Complications for a full list of age and health factors that confer increased risk.
More information is available at Who Should Get Vaccinated Against Influenza.
Who Should Not Be Vaccinated?
Different flu vaccines are approved for use in different groups of people. Factors that can determine a person's suitability for vaccination, or vaccination with a particular vaccine, include a person's age, health (current and past) and any relevant allergies, including an egg allergy.
Flu Shot:
People who cannot get a flu shot
People who should talk to their doctor before getting the flu shot
Nasal Spray Vaccine:
People who cannot get a nasal spray vaccine
People who should talk to their doctor before getting the nasal spray vaccine
When should I get vaccinated?
Flu vaccination should begin soon after vaccine becomes available, ideally by October. However, as long as flu viruses are circulating, vaccination should continue to be offered throughout the flu season, even in January or later. While seasonal influenza outbreaks can happen as early as October, during most seasons influenza activity peaks in January or later. Since it takes about two weeks after vaccination for antibodies to develop in the body that protect against influenza virus infection, it is best that people get vaccinated so they are protected before influenza begins spreading in their community.
Flu vaccine is produced by private manufacturers, and the timing of availability depends on when production is completed. Shipments began in August and will continue throughout October and November until all vaccine is distributed.
http://www.flu.gov/stay-connected/vaccinelocator_2011.html
Where can I get a flu vaccine?
Flu vaccines are offered in many locations, including doctor’s offices, clinics, health departments, pharmacies and college health centers, as well as by many employers, and even in some schools.
Even if you don’t have a regular doctor or nurse, you can get a flu vaccine somewhere else, like a health department, pharmacy, urgent care clinic, and often your school, college health center, or work.
Why do I need a flu vaccine every year?
A flu vaccine is needed every season for two reasons. First, the body’s immune response from vaccination declines over time, so an annual vaccine is needed for optimal protection. Second, because flu viruses are constantly changing, the formulation of the flu vaccine is reviewed each year and sometimes updated to keep up with changing flu viruses. For the best protection, everyone 6 months and older should get vaccinated annually.
Does flu vaccine work right away?
No. It takes about two weeks after vaccination for antibodies to develop in the body and provide protection against influenza virus infection. That’s why it’s better to get vaccinated early in the fall, before the flu season really gets under way.
Can I get seasonal flu even though I got a flu vaccine this year?
Yes. There is still a possibility you could get the flu even if you got vaccinated. The ability of flu vaccine to protect a person depends on various factors, including the age and health status of the person being vaccinated, and also the similarity or “match” between the viruses used to make the vaccine and those circulating in the community. If the viruses in the vaccine and the influenza viruses circulating in the community are closely matched, vaccine effectiveness is higher. If they are not closely matched, vaccine effectiveness can be reduced. However, it’s important to remember that even when the viruses are not closely matched, the vaccine can still protect many people and prevent flu-related complications. Such protection is possible because antibodies made in response to the vaccine can provide some protection (called cross-protection) against different but related influenza viruses. For more information about vaccine effectiveness, visit How Well Does the Seasonal Flu Vaccine Work?
Vaccine Effectiveness
Influenza vaccine effectiveness (VE) can vary from year to year and among different age and risk groups. For more information about vaccine effectiveness, visit How Well Does the Seasonal Flu Vaccine Work? For information specific to this season, visit About the Current Flu Season.
Vaccine Benefits
What are the benefits of flu vaccination?
While how well the flu vaccine works can vary, there are a lot of reasons to get a flu vaccine each year.
Flu vaccination can keep you from getting sick from flu. Protecting yourself from flu also protects the people around you who are more vulnerable to serious flu illness.
Flu vaccination can help protect people who are at greater risk of getting seriously ill from flu, like older adults, people with chronic health conditions and young children (especially infants younger than 6 months old who are too young to get vaccinated).
Flu vaccination also may make your illness milder if you do get sick.
Flu vaccination can reduce the risk of more serious flu outcomes, like hospitalizations and deaths.
A recent study* showed that flu vaccine reduced children’s risk of flu-related pediatric intensive care unit (PICU) admission by 74% during flu seasons from 2010-2012.
One study showed that flu vaccination was associated with a 71% reduction in flu-related hospitalizations among adults of all ages and a 77% reduction among adults 50 years of age and older during the 2011-2012 flu season.
Flu vaccination is an important preventive tool for people with chronic health conditions. Vaccination was associated with lower rates of some cardiac events among people with heart disease, especially among those who had had a cardiac event in the past year. Flu vaccination also has been shown to be associated with reduced hospitalizations among people with diabetes (79%) and chronic lung disease (52%).
Vaccination helps protect women during pregnancy and their babies for up to 6 months after they are born. One study showed that giving flu vaccine to pregnant women was 92% effective in preventing hospitalization of infants for flu.
Other studies have shown that vaccination can reduce the risk of flu-related hospitalizations in older adults. A study that looked at flu vaccine effectiveness over the course of three flu seasons estimated that flu vaccination lowered the risk of hospitalizations by 61% in people 50 years of age and older.
References for the studies listed above can be found at Publications on Influenza Vaccine Benefits. Also see the What are the Benefits of Flu Vaccination? [264 KB, 2 pages] fact sheet.
Vaccine Match
Will this season's vaccine be a good match for circulating viruses?
It's not possible to predict with certainty which flu viruses will predominate during a given season. Over the course of a flu season, CDC studies samples of flu viruses circulating during that season to evaluate how close a match there is between viruses used to make the vaccine and circulating viruses. Data are published in the weekly FluView. In addition, CDC conducts studies each year to determine how well the vaccine protects against illness during that season. The results of these studies are typically published following the conclusion of the flu season and take into consideration all of the data collected during the season. Interim preliminary estimates of the vaccine’s benefits that season using data available at that time also may be provided. For more information, see Vaccine Effectiveness – How Well Does the Flu Vaccine Work?
Flu viruses are constantly changing (called “antigenic drift”) – they can change from one season to the next or they can even change within the course of one flu season. Experts must pick which viruses to include in the vaccine many months in advance in order for vaccine to be produced and delivered on time. (For more information about the vaccine virus selection process visit Selecting the Viruses in the Influenza (Flu) Vaccine.) Because of these factors, there is always the possibility of a less than optimal match between circulating viruses and the viruses in the vaccine.
Can the vaccine provide protection even if the vaccine is not a "good" match?
Yes, antibodies made in response to vaccination with one flu virus can sometimes provide protection against different but related viruses. A less than optimal match may result in reduced vaccine effectiveness against the virus that is different from what is in the vaccine, but it can still provide some protection against influenza illness.
In addition, even when there is a less than optimal match or lower effectiveness against one virus, it's important to remember that the flu vaccine is designed to protect against three or four flu viruses, depending on the vaccine.
For these reasons, even during seasons when there is a less than optimal match, CDC continues to recommend flu vaccination. This is particularly important for people at high risk for serious flu complications, and their close contacts.
Vaccine Side Effects (What to Expect)
Can the flu vaccine give me the flu?
No, a flu vaccine cannot cause flu illness. Flu vaccines that are administered with a needle are currently made in two ways: the vaccine is made either with a) flu vaccine viruses that have been ‘inactivated’ and are therefore not infectious, or b) with no flu vaccine viruses at all (which is the case for recombinant influenza vaccine). The nasal spray flu vaccine does contain live viruses. However, the viruses are attenuated (weakened), and therefore cannot cause flu illness. The weakened viruses are cold-adapted, which means they are designed to only cause infection at the cooler temperatures found within the nose. The viruses cannot infect the lungs or other areas where warmer temperatures exist.
While a flu vaccine cannot give you flu illness, there are different side effects that may be associated with getting a flu shot or a nasal spray flu vaccine. These side effects are mild and short-lasting, especially when compared to symptoms of bad case of flu.
The flu shot: The viruses in the flu shot are killed (inactivated), so you cannot get the flu from a flu shot. Some minor side effects that may occur are:
Soreness, redness, or swelling where the shot was given
Fever (low grade)
Aches
The nasal spray: The viruses in the nasal spray vaccine are weakened and do not cause severe symptoms often associated with influenza illness. In children, side effects from the nasal spray may include:
Runny nose
Wheezing
Headache
Vomiting
Muscle aches
Fever
In adults, side effects from the nasal spray vaccine may include:
Runny nose
Headache
Sore throat
Cough
If these problems occur, they begin soon after vaccination and are mild and short-lived. Almost all people who receive influenza vaccine have no serious problems from it. However, on rare occasions, flu vaccination can cause serious problems, such as severe allergic reactions. People who think that they have been injured by the flu shot can file a claim for compensation from the National Vaccine Injury Compensation Program (VICP).
More information about the safety of flu vaccines is available at Influenza Vaccine Safety.
Vaccine Supply and Distribution
How much vaccine will be available during 2014-2015?
Currently, seven influenza vaccine manufacturers are projecting that as many as 151 million to 156 million doses of influenza vaccine will be available for use in the United States during the 2014-2015 influenza season.
Where can I find information about vaccine supply?
Information about vaccine supply is available on the CDC influenza web site.
Why do manufacturers and distributors take a phased approach to vaccine distribution?
Influenza vaccine production begins as early as 6 to 9 months before the beginning of vaccine distribution. Even with this early start, it isn’t possible to complete the entire production and distribution process prior to flu season, in part because of the limited number of influenza vaccine manufacturing plants in the United States and the large number of doses that are produced each year. Instead, influenza vaccine distribution takes place in a phased fashion over a number of months. Distribution usually begins in late summer and is complete near the end of November or early in December. This may result in some uncertainty making it difficult for vaccine providers to plan their vaccination activities. Manufacturers and distributors try to get some vaccine to as many providers as possible as early as possible so that they can begin vaccinating their patients.
What role does the Department of Health and Human Services play in the supply and distribution of the seasonal influenza vaccine?
Influenza vaccine production and distribution are primarily private sector endeavors. The Department of Health and Human Services and CDC do not have the authority to control influenza vaccine distribution nor the resources to manage such an effort. However, the Department has made significant efforts to enhance production capacity of seasonal influenza vaccines, including supporting manufacturers as they invest in processes to stabilize and increase their production capacity.
More Information
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
N1H1 Influenza (Swine Flu)
The 2009 outbreak of a new strain of H1N1 influenza A demonstrated that continuing vigilance, planning, and strong public health research capability are essential defenses against emerging health threats.
Past research on H5N1 (bird flu) as well as other influenza viruses with potential to create pandemics prepared NIAID scientists to respond to this newest influenza threat. Researchers expanded and refocused projects to include studies of the course of the virus, the origin of the virus, H1N1-infected patients, and a preventive vaccine. Many of these studies involve collaborations with other federal agencies, academia, and the private sector. Scientific findings continue to shed light on the mysteries of influenza, and will help researchers create better, faster vaccine production techniques, and better treat severely ill people.
Research
Ongoing influenza research is wide-ranging, and falls into several categories:
Recent Scientific Findings
Basic Research
Diagnostic Progress
Advances in Treatment
Vaccines Research
Pandemic
Reports and Plans
Influenza is notable in its ability to produce annual epidemics of disease in both developed and developing countries. Currently, influenza vaccination is the primary method of preventing influenza and its severe complications. Learn about NIAID-supported influenza clinical studies and ongoing avian influenza clinical trials.
Common Cold and Runny Nose
Overview of Common Cold
A cold usually includes a runny nose, sore throat, sneezing, and coughing. These symptoms can last for up to two weeks.
Causes
Common Cold
Over 200 viruses can cause the common cold
The rhinovirus is the most common type of virus that causes colds
Runny Nose during a Cold
When germs that cause colds first infect the nose and sinuses, the nose makes clear mucus. This helps wash the germs from the nose and sinuses. After two or three days, the body's immune cells fight back, changing the mucus to a white or yellow color. As the bacteria that live in the nose grow back, they may also be found in the mucus, which changes the mucus to a greenish color. This is normal and does not mean you or your child needs antibiotics.
Signs and Symptoms of the Common Cold
Sneezing
Stuffy or runny nose
Sore throat
Coughing
Watery eyes
Mild headache
Mild body aches
See a Healthcare Provider if You or Your Child has:
Temperature higher than 100.4° F
Symptoms that last more than 10 days
Symptoms that are not relieved by over-the-counter medicines
Your healthcare provider can determine if you or your child has a cold and can recommend symptomatic therapy. If your child is younger than three months of age and has a fever, it’s important to always call your healthcare provider right away.
Antibiotics are Needed When…
Antibiotics are needed only if your healthcare provider tells you that you or your child has a bacterial infection. Your healthcare provider may prescribe other medicine or give tips to help with a cold's symptoms, but antibiotics are not needed to treat a cold or runny nose.
Antibiotics Will Not Help if…
Since the common cold is caused by a virus, antibiotics will not help it get better. A runny nose or cold almost always gets better on its own, so it is better to wait and take antibiotics only when they are needed. Taking antibiotics when they are not needed can be harmful, and may lead to unwanted side effects like diarrhea, rashes, nausea, and stomach pain. More severe side effects may rarely occur, including life-threatening allergic reactions, kidney toxicity, and severe skin reactions.
Each time you or your child takes an antibiotic, the bacteria that normally live in your body (on the skin, in the intestine, in the mouth and nose, etc.) are more likely to become resistant to antibiotics. Common antibiotics cannot kill infections caused by these resistant germs.
How to Feel Better
Rest, over-the-counter medicines and other self-care methods may help you or your child feel better. For more information about symptomatic relief, visit the Symptom Relief section of this website or talk to your healthcare provider or pharmacist. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Preventing the Common Cold
Practice good hand hygiene
Avoid close contact with people who have colds or other upper respiratory infections
Protect Yourself and Others
Sore throat and runny nose are usually the first signs of a cold, followed by coughing and sneezing. Most people recover in 7-10 days or so. Protect yourself and others by taking simple steps.
Common colds are the main reason that children miss school and adults miss work. Each year in the United States, there are millions of cases of the common cold. Adults have an average of 2-3 colds per year, and children have even more.
Most people get colds in the winter and spring, but it is possible to get a cold at any time of the year. Symptoms usually include sore throat, runny nose, coughing, sneezing, watery eyes, headaches and body aches. Most people recover within about 7-10 days. However, people with weakened immune systems, asthma, or respiratory conditions may develop serious illness, such as pneumonia.
Rhinoviruses
cause colds
trigger asthma attacks
have been linked to sinus and ear infections
Many different viruses can cause the common cold, but rhinoviruses are the most common. Viruses that cause colds can spread from infected people to others through the air and close personal contact. You can also get infected through contact with stool or respiratory secretions from an infected person. This can happen when you shake hands with someone who has a cold, or touch a doorknob that has viruses on it, then touch your eyes, mouth, or nose.
How to Protect Yourself and Others
You can help reduce your risk of getting a cold:
Wash your hands often with soap and water
Scrub them for 20 seconds, and help young children do the same. If soap and water are not available, use an alcohol-based hand sanitizer. Viruses live on your hands, and regular handwashing can help protect you from getting sick.
Avoid touching your eyes, nose, and mouth with unwashed hands
Viruses can enter your body this way and make you sick.
Stay away from people who are sick
Sick people can spread viruses that cause the common cold through close contact with others.
Other Viruses
Other viruses that can cause cold-like symptoms:
respiratry syncytial virus
human parainfluenza viruses
human metapneumovirus
If you have a cold, you should follow these tips to prevent viruses from spreading to other people:
Stay at home while you are sick
Avoid close contact with others, such as hugging, kissing, or shaking hands
Move away from people before coughing or sneezing
Cough and sneeze into a tissue then throw it away, or cough and sneeze into your upper shirt sleeve, completely covering your mouth and nose
Wash your hands after coughing, sneezing, or blowing your nose
Disinfect frequently touched surfaces, and objects such as toys and doorknobs
There is no vaccine to protect you against the common cold.
How to Feel Better
There is no cure for a cold. To feel better, you should get lots of rest and drink plenty of fluids. Over-the-counter medicines may help ease symptoms but will not make your cold go away any faster. Always read the label and use medications as directed. Talk to your doctor before giving your child nonprescription cold medicines, since some medicines contain ingredients that are not recommended for children. Learn more about symptom relief.
Antibiotics will not help you recover from a cold. They do not work against viruses, and they may make it harder for your body to fight future bacterial infections if you take them unnecessarily. Learn more about when antibiotics work.
When to See a Doctor
You should call your doctor if you or your child has one or more of these conditions:
a temperature higher than 100.4° F
symptoms that last more than 10 days
symptoms that are severe or unusual
If your child is younger than 3 months old and has a fever, you should always call your doctor right away. Your doctor can determine if you or your child has a cold and can recommend therapy to help with symptoms.
More Information
Common Cold and Runny Nose, CDC
Common Cold, U.S. National Library of Medicine
Handwashing: Clean Hands Saves Lives, CDC
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
Is It Strep Throat?
Strep throat is a common type of sore throat in children, but it's not very common in adults. Healthcare professionals can do a quick test to detemine if a sore throat is strep throat and decide if antibiotics are needed. Proper treatment can help you feel better faster and prevent spreading it to others!
Many things can cause that unpleasant, scratchy, and sometimes painful condition known as a sore throat. Viruses, bacteria, allergens, environmental irritants (such as cigarette smoke), chronic postnasal drip and fungi can all cause a sore throat. While many sore throats will get better without treatment, some throat infections—including strep throat—may need antibiotic treatment.
How You Get Strep Throat
Strep throat is an infection in the throat and tonsils caused by group A Streptococcus bacteria (called "group A strep"). Group A strep bacteria can also live in a person's nose and throat without causing illness. The bacteria are spread through contact with droplets after an infected person coughs or sneezes. If you touch your mouth, nose, or eyes after touching something that has these droplets on it, you may become ill. If you drink from the same glass or eat from the same plate as the sick person, you could also become ill. It is also possible to get strep throat from contact with sores from group A strep skin infections.
A fever is a common symptom of strep throat.
Common Symptoms of Strep Throat
The most common symptoms of strep throat include:
Sore throat, usually starts quickly and can cause severe pain when swallowing
A fever (101°F or above)
Red and swollen tonsils, sometimes with white patches or streaks of pus
Tiny red spots (petechiae) on the area at the back of the roof of the mouth (the soft or hard palate)
Headache, nausea, or vomiting
Swollen lymph nodes in the neck
Body aches or rash
A Simple Test Gives Fast Results
Healthcare professionals can test for strep by swabbing the throat to quickly see if group A strep bacteria are causing a sore throat. A strep test is needed to tell if you have strep throat; just looking at your throat is not enough to make a diagnosis. If the test is positive, your healthcare professional can prescribe antibiotics. If the strep test is negative, but your clinician still strongly suspects you have this infection, then they can take a throat culture swab to test for the bacteria.
Antibiotics reduce the length of time you’re sick and reduce your symptoms.
Antibiotics Get You Well Fast
The strep test results will help your healthcare professional decide if you need antibiotics, which can:
Decrease the length of time you're sick
Reduce your symptoms
Help prevent the spread of infection to friends and family members
Prevent more serious complications, such as tonsil and sinus infections, and acute rheumatic fever (a rare inflammatory disease that can affect the heart, joints, skin, and brain)
You should start feeling better in just a day or two after starting antibiotics. Call your healthcare professional if you don't feel better after taking antibiotics for 48 hours. People with strep throat should stay home from work, school, or daycare until they have taken antibiotics for at least 24 hours so they don't spread the infection to others.
Be sure to finish the entire prescription, even when you start feeling better, unless your healthcare professional tells you to stop taking the medicine. When you stop taking antibiotics early, you risk getting an infection later that is resistant to antibiotic treatment.
More Prevention Tips: Wash Those Hands
The best way to keep from getting strep throat is to wash your hands often and avoid sharing eating utensils, like forks or cups. It is especially important for anyone with a sore throat to wash their hands often and cover their mouth when coughing and sneezing. There is no vaccine to prevent strep throat.
What Is Sinusitis?
Sinusitis (Sinus infection)
Your nose is stuffy. You have thick, yellowish mucus. You’re coughing, and you feel tired and achy. You think that you have a cold. You take medicines to relieve your symptoms, but they don’t help. When you also get a terrible headache, you finally drag yourself to the doctor. After listening to your history of symptoms and examining your face and forehead, the doctor says you have sinusitis.
"Sinusitis" simply means your sinuses are inflamed¯red and swollen¯because of an infection or another problem. There are several types of sinusitis. Health experts usually identify them as follows:
Acute, which lasts up to four weeks
Subacute, which lasts 4 to 12 weeks
Chronic, which lasts more than 12 weeks and can continue for months or even years
Recurrent, with several attacks within a year
In 2011, the Centers for Disease Control and Prevention reported that nearly 30 million adults were diagnosed with sinusitis. Women were almost twice as likely as men to receive the diagnosis, and there were more cases in the southern United States than elsewhere in the country.
When people say, "My sinuses are killing me," they usually are referring to symptoms of congestion and achiness in one or more of the four pairs of cavities (air-filled spaces) known as paranasal sinuses. These small hollow spaces, which are located within the skull or bones of the head surrounding the nose, are named for the bones that contain them, as follows:
Frontal sinuses over the eyes in the brow area
Maxillary sinuses inside each cheekbone
Ethmoid sinuses just behind the bridge of the nose, between the eyes
Sphenoid sinuses behind the ethmoids in the upper region of the nose and behind the eyes
The paranasal sinuses open into the nasal cavity and are lined with cells that make mucus to keep the nose from drying out during breathing and to trap unwanted materials so that they do not reach the lungs.
What Are the Symptoms of Sinusitis?
Credit: iStockPhoto
One of the most common symptoms of any type of sinusitis is pain, and the location depends on which sinus is affected.
Pain in your forehead means the problem lies in your frontal sinuses.
Pain in your upper jaw and teeth, with tender cheeks, may mean your maxillary sinuses are involved.
Pain between your eyes, sometimes with swelling of the eyelids and tissues around your eyes, and tenderness when you touch the sides of your nose may mean sinusitis has developed in your ethmoid sinuses.
Pain in your neck, with earaches, and deep achiness at the top of your head could be a sign that your sphenoid sinuses are involved (though these sinuses are affected less often).
Most people with sinusitis have pain or tenderness in several places, and their symptoms usually do not clearly indicate which sinuses are inflamed. Pain is not as common in chronic sinusitis as it is in acute sinusitis.
In addition to the pain, people who have sinusitis (acute or chronic) often have thick nasal secretions that can be white, yellowish, greenish, or blood-tinged. Sometimes these secretions drain in the back of the throat and are difficult to clear. This is referred to as “post-nasal drip.” Also, cases of acute and chronic sinusitis are usually accompanied by a stuffy nose, as well as by a general feeling of fullness over the entire face.
Less common symptoms of sinusitis (acute or chronic) can include the following:
Tiredness
Decreased sense of smell
Cough that may be worse at night
Sore throat
Bad breath
Fever
On very rare occasions, acute sinusitis can result in brain infection and other serious complications.
Because your nose can get stuffy or congested when you have a condition like the common cold, you may confuse simple nasal congestion with sinusitis. A cold usually lasts about 7 to 14 days and goes away without treatment. Acute sinusitis often lasts longer and typically causes more symptoms than a cold.
What Causes the Symptoms of Sinusitis?
The paranasal sinuses, like the inside of your nose, are lined with a thin layer of tissue called the mucous membrane, which produces mucus. This mucus flows out through openings of the paranasal sinuses and into the nose. When these openings become blocked, your sinuses are affected.
Anything that causes swelling in the nose can block the openings between your paranasal sinuses and your nose, including a cold, an allergic reaction such as hay fever, or a reaction to some chemical to which you've been exposed. The blockage causes air and mucus to become trapped within the sinuses. This may cause pain and thickened mucus.
The pain of a sinus attack arises because the trapped air and mucus put pressure on the mucous membrane of the sinuses and the bony wall behind it. Also, when a swollen membrane at the opening of a paranasal sinus prevents air from entering into the sinuses, it can create a vacuum that causes pain.
Mucus thickens because it loses its water content as it stays trapped inside the sinuses for a long time. In addition, inflammation leads to extra materials being secreted into the mucus, causing thickening.
What Are the Differences Between Acute and Chronic Sinusitis?
Content:
Acute Sinusitis
Chronic Sinusitis
Acute Sinusitis
Acute sinusitis can be caused by the following:
Common cold
Allergies and other chronic conditions
Pre-existing health conditions
Common cold
Most cases of acute sinusitis start with a common cold, which is caused by a virus. Colds can inflame your sinuses and cause symptoms of sinusitis. Both the cold and the sinus inflammation usually go away without treatment within two weeks. If the inflammation produced by the cold leads to infection caused by bacteria, then this infection becomes acute sinusitis.
The inflammation caused by the cold results in swelling of the mucous membranes of your sinuses, trapping air and mucus behind the narrowed sinus openings. When mucus stays inside your sinuses and is unable to drain into your nose, it can become the source of nutrients for bacteria, which can then multiply.
Most healthy people have bacteria, such as Streptococcus pneumoniaeand Haemophilus influenzae, in their noses and throats. Usually, these bacteria cause no problems, but when you sniff or blow your nose when you have a cold, these actions create pressure changes that can send typically harmless bacteria into the sinuses. If your sinuses stop draining properly, the bacteria can begin to multiply in your sinuses, causing acute sinusitis.
Allergies and other chronic conditions
People who have allergies or other chronic problems that affect the nose also are prone to episodes of acute sinusitis. Chronic nasal problems cause the mucous membranes to swell and the sinus passages to become blocked. The normally harmless bacteria in your nose and throat again lead to acute sinusitis.
Pre-existing health conditions
In general, people who have reduced immune function, such as those with primaryimmune deficiencydisease(a defect in the way the immune system responds to infection) or HIV infection, are more likely to suffer from sinusitis. People who have abnormal mucus secretion or mucus movement, such as those with cystic fibrosis (an inherited disease in which thick and sticky mucus clogs the lungs, causing breathing problems and making it easier for bacteria to grow), also are more likely to suffer from sinusitis.
Infections caused by fungi very rarely cause acute sinusitis because the human body has a natural resistance to fungi; however, in people whose immune systems are not functioning properly, fungi can cause acute sinusitis.
Chronic Sinusitis
In chronic sinusitis, the membranes of both the paranasal sinuses and the nose thicken because they are constantly inflamed. Most health experts now use the term “chronic rhinosinusitis” to describe this condition. They also recommend that the condition be distinguished as either rhinosinusitis with or rhinosinusitis without nasal polyps.
Nasal polyps are grape-like growths of the mucous membrane that protrude into the sinuses or nasal passages, making it even more difficult for the sinuses to drain and for air to pass through the nose. The causes of chronic rhinosinusitis are largely unknown, but there are some conditions that may put you at higher risk for developing it, including the following:
Asthma and allergies
Recurrent acute sinusitis
Pre-existing health conditions
Asthma and allergies
Chronic rhinosinusitis often occurs in people who have asthma, many of whom also have allergies. It is possible that constant exposure to airborne allergens (substances that causes an allergic reaction) from house dust mites, pets, mold, and cockroaches causes chronic inflammation of the lining of the nose and the sinuses. An allergic reaction to certain fungi causes some cases of chronic rhinosinusitis: this condition is called allergic fungal sinusitis. However, at least half of all people who have chronic rhinosinusitis do not have allergies.
Recurrent acute sinusitis
Although most health experts believe that chronic rhinosinusitis is not an infectious disease like acute sinusitis, if you suffer from frequent episodes of acute sinusitis, you may be prone to developing chronic rhinosinusitis. Some experts believe that chronic rhinosinusitis is caused by an exaggerated immune response to fungi that normally are found in the sinuses or to the bacterium Staphylococcus aureus, which commonly lives inside the nose.
Pre-existing health conditions
As with acute sinusitis, other causes of chronic rhinosinusitis may be an immune deficiency disorder or cysticfibrosis.
Some people are born with a physical structure inside the nose that makes mucus flow out of the sinuses difficult. Others may develop a structural problem after experiencing an injury to the nose. These people are at higher risk for developing chronic rhinosinusitis.
How Is Sinusitis Diagnosed?
Your healthcare provider usually can diagnose acute sinusitis by noting your symptoms and examining your nose and face. If your symptoms do not clearly indicate that you have sinusitis or if they persist for a long time and do not get better with treatment, your healthcare professional may order a CT (computerized tomography) scan (a form of X-ray that shows some soft-tissue and other structures that cannot be seen in conventional X-rays) to confirm that you have sinusitis.
Other laboratory tests your healthcare professional may use to check for possible causes of chronic rhinosinusitis include the following:
Blood tests to rule out conditions, such as an immune deficiency disorder, that are associated with sinusitis
A sweat test or a blood test to rule out cystic fibrosis
Tests on the material inside your sinuses to detect bacterial or fungal infection
Credit: NIAID
Sinusitis
How Is Sinusitis Treated?
After diagnosing sinusitis and identifying a possible cause, your healthcare provider can suggest various treatments.
Acute sinusitis
If you have acute sinusitis, your healthcare provider may recommend the following:
Antibiotics to control a bacterial infection, if present
Pain relievers to reduce any pain
Decongestants (medicines that shrink the swollen membranes in the nose and make it easier to breathe)
Even if you have acute sinusitis, your healthcare provider may choose not to use an antibiotic because many cases of acute sinusitis will end on their own. However, if you do not feel better after a few days, you should contact your healthcare provider again.
Follow your healthcare provider's instructions on how to use over-the-counter or prescription decongestant nose drops and sprays. You should use these medicines for only a few days, as longer term use can lead to even more congestion and swelling of your nasal passages.
If you suffer from nasal allergies, such as hay fever, along with sinusitis, your healthcare provider may recommend medicine to control your allergies. This may include a nasal steroid spray that reduces the swelling around the sinus passages and allows the sinuses to drain.
If you have asthma and then get sinusitis, your asthma may worsen. You should contact your healthcare profvider, who may change your asthma treatment.
Chronic Rhinosinusitis
Healthcare providers often find it difficult to treat chronic rhinosinusitis successfully. They have two options to offer patients: medicine and surgery.
Medicine
Nasal steroid sprays are helpful for many people, but most people still do not get full relief of symptoms with these medicines.
A long course of antibiotics is occasionally recommended by doctors, but results from clinical research do not support this kind of antibiotic use.
Saline (saltwater) washes or saline nasal sprays can be helpful in chronic rhinosinusitis because they remove thick secretions and allow the sinuses to drain.
Oral steroids, such as prednisone, may be prescribed for severe chronic rhinosinusitis. However, oral steroids are powerful medicines with significant side effects, and these medicines typically are prescribed when other medicines have failed.
Research is needed to develop new, more effective treatments.
Surgery
When medicine fails, surgery may be the only alternative for treating chronic rhinosinusitis. The goal of surgery is to improve sinus drainage and reduce blockage of the nasal passages. Nasal surgery usually is performed to accomplish the following:
Enlarge the natural openings of the sinuses
Remove nasal polyps
Correct significant structural problems inside the nose and the sinuses if they contribute to sinus obstruction
Although most people have fewer symptoms and a better quality of life after surgery, problems can recur, sometimes even after a short period of time.
In children, problems can sometimes be eliminated by removing the adenoids. These gland-like tissues, located high in the throat behind and above the roof of the mouth, can obstruct the nasal passages.
Can Sinusitis Be Prevented?
There are no methods that have been proven scientifically to prevent acute or chronic sinusitis. Your healthcare provider may recommend the following measures that can help:
Keep your nose as moist as possible with frequent use of saline sprays or washes.
Avoid very dry indoor environments and use a humidifier, if necessary. Be aware, however, that a humid environment also may increase the amount of mold, dust mite, or cockroach allergens in your home; this is important only if you are allergic to any of those organisms.
Avoid exposure to irritants such as cigarette and cigar smoke or strong odors from chemicals.
Avoid exposure to substances to which you are allergic.
If you haven’t been tested for allergies and you are getting frequent sinus infections, ask your healthcare provider to give you an allergy evaluation or refer you to an allergy specialist.
Avoid long periods of swimming in pools treated with chlorine, which can irritate the lining of the nose and sinuses.
Avoid water diving, which forces water into the sinuses from the nasal passages.
Credit: iStock Photo
Air travel may pose a problem if you suffer from acute or chronic sinusitis. When air pressure in a plane is reduced, pressure can build up in your head, blocking your sinuses or the eustachian tubes (the airways between the middle ear and the back of the throat that equalize air pressure on either side of the eardrum). As a result, you might feel discomfort in your sinuses or middle ear during the plane’s ascent or descent. Some health experts recommend using decongestant nose drops or sprays before a flight to avoid this problem
Are Researchers Studying Sinusitis?
NIAID supports research to better understand the immune system in health and disease and to develop new treatments. Examples of NIAID-supported research to improve our understanding of the causes of sinusitis and to develop treatments for the condition include the following:
Most people who have moderate to severe asthma also have chronic rhinosinusitis, suggesting that these two diseases may be the same disease occurring in the lower and upper parts of the respiratory system, respectively. NIAID supports research to understand the causes of chronic airway inflammation in asthma that could help scientists understand chronic rhinosinusitis and develop more effective treatment and prevention strategies.
Streptococcus pneumoniae
At least two-thirds of acute sinusitis cases are caused by two bacteria: Streptococcus pneumoniae and Haemophilus influenzae. NIAID supports studies to better understand how these bacteria cause infection and to identify potential targets for future vaccination strategies that could prevent these infections.
NIAID funds research that examines the causes of thickening and inflammation of the lining of the sinuses and nasal passages. These projects also focus on the cells that produce mucus and line the sinuses and nasal passages.
In many people who have chronic rhinosinusitis, especially those with nasal polyps, a large number of eosinophils (white blood cells that have strong inflammatory properties) are found in the tissues that line the sinuses and nasal passages. NIAID funds several projects that examine the role of eosinophils and the messenger molecules they produce in causing chronic sinus inflammation and chronic rhinosinusitis with polyps.
NIAID supports research to test the theory that chronic rhinosinusitis is caused by an exaggerated immune response to fungi. One study has shown that when blood cells from people who have chronic rhinosinusitis are exposed to fungal material, these cells make messenger molecules that cause inflammation.
NIAID supports projects to identify human genes and proteins that are different in patients who have chronic rhinosinusitis from those whose sinuses are healthy. The results will help us understand the causes of chronic rhinosinusitis and develop promising new treatments. For example, research has found that some people who have chronic rhinosinusitis also have certain alterations in the gene that causes cysticfibrosis.
Source: NIAID, NIH
Allergy
Also called: Hypersensitivity
An allergy is a reaction by your immune system to something that does not bother most other people. People who have allergies often are sensitive to more than one thing. Substances that often cause reactions are
Pollen
Dust mites
Mold spores
Pet dander
Food
Insect stings
Medicines
Normally, your immune system fights germs. It is your body's defense system. In most allergic reactions, however, it is responding to a false alarm. Genes and the environment probably both play a role.
Allergies can cause a variety of symptoms such as a runny nose, sneezing, itching, rashes, swelling, or asthma. Allergies can range from minor to severe. Anaphylaxis is a severe reaction that can be life-threatening. Doctors use skin and blood tests to diagnose allergies. Treatments include medicines, allergy shots, and avoiding the substances that cause the reactions.
Latex Allergy

Latex is a milky fluid that comes from the tropical rubber tree. Hundreds of everyday products contain latex. Repeated exposure to a protein in natural latex can make you more likely to develop a latex allergy. If your immune system detects the protein, a reaction can start in minutes. You could get a rash, asthma and in rare cases shock from latex exposure.
Your doctor may use a physical exam and skin and blood tests to diagnose it. There are medicines to treat a reaction, but it is best to try to avoid latex. Common latex products include
Gloves
Condoms
Balloons
Rubber bands
Shoe soles
Pacifiers
You can find latex-free versions of these products.
NIH: National Institute of Allergy and Infectious Diseases
Pollen Allergy
Each spring, summer, and fall, tiny pollen grains are released from trees, weeds, and grasses. These grains hitch rides on currents of air. Although the job of pollen is to fertilize plants, many grains never reach their targets. Instead, pollen can enter your eyes, nose, and throat and trigger pollen allergy.
Introduction to Pollen Allergy
Many people know pollen allergy as hay fever, but health experts usually refer to it as “seasonal allergic rhinitis.” This simply means an allergy to pollen that makes your nose run during certain seasons.
Of all the things that can cause an allergy, pollen is one of the most common. To a great extent, people can avoid many of the foods, medicines, or animals that cause allergies. But, short of staying indoors with the windows closed when the pollen count is high—and even that may not help—people have no easy way to avoid breathing in pollen that floats in the air.
What is an allergy?
An allergy is a specific reaction of your body’s immune system to a normally harmless substance. People who have allergies often are sensitive to more than one substance. Symptoms of pollen allergy include any of the following:
Runny nose
Sneezing
Itchy eyes
Congestion of the nose
Red and watery eyes
Content
What Is Pollen?
Which Types of Pollen Cause Allergies?
When Do Plants Make Pollen?
What Is a Pollen Count?
What Is Pollen?
Plants produce round pollen grains. Individual grains are too tiny to see with the naked eye, but some can form large, visible clusters. For fertilization to take place and seeds to form in some plants, pollen must be moved from the flower of one plant to that of another of the same species—for example, from one oak tree to another oak tree—by a process called cross-pollination. Insects do this job for certain flowering plants, while other plants, such as ragweed, rely on wind to transport their pollen grains.
Scanning electron micrograph of ragweed. Small, round pollen grains are visible. Credit: CDC/Janice Haney Carr
Some grasses that produce pollen
Timothy grass
Kentucky bluegrass
Johnson grass
Bermuda grass
Redtop grass
Orchard grass
Sweet vernal grass
Which Types of Pollen Cause Allergies?
Most of the pollen that causes allergic reactions comes from plants that don’t have showy flowers, such as trees, weeds, and grasses. These plants make small, light, and dry pollen grains that are made to be carried by wind.
Because airborne pollen can drift for many miles, removing an offending plant may not help. Amazingly, scientists have collected samples of ragweed pollen 400 miles out at sea and 2 miles high in the air. In addition, most allergy-causing pollen comes from plants that produce it in huge quantities. For example, a single ragweed plant can generate a million grains of pollen every day.
The components of a pollen grain are the main factors that determine whether that pollen is likely to cause allergic rhinitis. For example, pine tree pollen is produced in large amounts by a common tree, but it is not a major cause of pollen allergy because the components of pine pollen are less likely to cause an allergic reaction.
Some trees that produce pollen
Oak
Ash
Elm
Hickory
Pecan
Box elder
Mountain elder
Among North American plants, weeds produce the largest amounts of allergenic pollen. Ragweed is the major culprit, but other important sources of weed pollen come from sagebrush, redroot pigweed, lamb’s quarters, Russian thistle (tumbleweed), and English plantain. Some species of grasses and trees also produce highly allergenic pollen.
Although some people may think they are allergic to colorful or scented flowers like roses, it’s not usually the case. Only florists, gardeners, and others who have close contact with flowers over a long period of time are likely to be sensitive to pollen from these plants. In fact, most people have little contact with the large, heavy, and waxy pollen grains of flowering plants because this type of pollen is not carried by wind, but by insects such as butterflies and bees.
When Do Plants Make Pollen?
One of the obvious features of pollen allergy is its seasonal nature—people have symptoms only when the pollen grains to which they are allergic are in the air. Each plant pollinates more or less at the same time from year to year. Exactly when a plant starts to pollinate seems to depend on the relative length of night and day—and therefore on geographical location—rather than on the weather. But weather conditions during pollination can affect the amount of pollen produced and carried by the wind in a specific year. For example, in the Northern Hemisphere, areas farther north experience a later start to the pollinating period and the pollen allergy season.
What Is a Pollen Count?
A pollen count, often reported by local weather broadcasts or allergy websites each year, is a measure of how much pollen is in the air. This count represents the concentration of all the pollen (or of one particular type, like ragweed) in the air in a certain area at a specific time. It is reported as grains of pollen per cubic meter of air collected over 24 hours.
Pollen counts tend to be the highest early in the morning on warm, dry, breezy days and the lowest during chilly, wet periods. Although the pollen count changes, it is useful as a general guide for when it may be wise for you to stay indoors and avoid contact with that pollen.
How is Pollen Allergy Diagnosed?
A person receiving a skin prick test. A number of allergens can be tested with a skin prick test, including ragweed and grass pollens. Credit: NIAID
Skin test
A doctor with expertise in allergic diseases, known as an allergist, or other healthcare professional will use a skin prick test to find out whether you have antibodies that react to a specific allergen. These antibodies, produced by the immune system, attach to mast cells in your skin. When the allergen binds to its antibody like a lock and key, the mast cells release histamine and other chemicals that cause allergy symptoms. A skin test is simple and relatively safe, and the results are ready in minutes.
With a skin prick test, your healthcare professional uses a needle to place a tiny amount of pollen extract (liquid substance) just below the surface of the skin on your lower arm or back. If you are allergic, there will be swelling or redness at the test site. Although such a reaction shows that you produce antibodies to a specific allergen, you might not have the respiratory and eye symptoms (runny nose, sneezing, itchy eyes) of an allergic reaction.
Blood tests
Instead of the skin test, your healthcare professional can take a blood sample to measure the levels of pollen-specific antibodies your body produces.
As with skin testing, positive blood tests don't necessarily mean that you have pollen allergy.
Medicines to Treat Pollen Allergy
Because it is nearly impossible to avoid contact with pollen, you might be able to control your symptoms with medicines. You can buy some allergy medicines without a prescription. Most over-the-counter medicines are antihistamines. These medicines are often helpful in people who have mild disease. If these medicines don’t give you relief or they cause unwanted side effects, your healthcare professional may write a prescription for a more powerful medicine. For example, you may be prescribed a topical nasal steroid to take with an antihistamine. Some people with seasonal allergic rhinitis develop complications, including asthma and sinusitis. If these complications develop, it's important to see a healthcare professional.
Types of medicines available to treat pollen allergy symptoms include the following:
Antihistamines
Topical nasal steroids
Cromolyn sodium
Decongestants
Antihistamines
Antihistamines have proven useful in relieving sneezing and itching in the nose and eyes and in reducing swelling and drainage in the nose because of pollen allergy.
Many people who take some types of antihistamines, available over the counter or by prescription, have some unwelcome side effects, such as drowsiness and loss of alertness and coordination. When children have such reactions, adults may interpret those reactions as behavior problems.
Effective antihistamines that cause fewer of these side effects are available over the counter or by prescription.
Topical nasal steroids
Topical nasal steroids are anti-inflammatory medicines that inhibit the allergic reaction. The combination of antihistamines and nasal steroids is a very effective way to treat pollen allergy, especially if your reaction to pollen is moderate or severe.
You should not confuse topical nasal steroids with anabolic steroids, which athletes sometimes use to improve their performance. The chemicals in nasal steroids are different from those in anabolic steroids.
Although topical nasal steroids can have side effects, they are safe when used at the recommended doses and for the recommended times.
Cromolyn sodium
Cromolyn sodium is a nasal spray that helps prevent allergic rhinitis from starting in some people. When used as a nasal spray, it can safely inhibit the release of chemicals that cause allergy symptoms. It has few side effects when used as directed and significantly helps some people manage their allergies.
Decongestants
Decongestants can help shrink your nasal passages. This, in turn, can help relieve congestion, swelling, and general discomfort in the sinus areas caused by nasal allergies. Your healthcare professional may recommend using oral or nasal decongestants to reduce congestion, along with an antihistamine to control your symptoms.
You shouldn’t use over-the-counter or prescription decongestant nose drops and sprays for more than a few days. When you use them for longer periods, these medicines can lead to even more congestion and swelling inside your nose and sinuses.
Allergy Shots
Currently, a series of allergy shots, called allergen immunotherapy, is the only available treatment that can provide a long-lasting benefit against allergies, even after the treatment is stopped. Allergy shots are given as subcutaneous (under the skin) injections. They contain increasing concentrations of the pollen allergen(s) to which you are sensitive. These shots reduce the level of antibodies to pollen in your blood and cause your body to make another protective antibody called IgG. Because these shots may have significant side effects, people need to stay in the healthcare professional’s office for a period of time after receiving the shots.
Health experts recommend that people who benefit from allergy shots continue receiving them for 3 years and then consider stopping them with the guidance of an allergy specialist. Although many people are able to stop the injections with good results lasting for several years, others do get worse after the shots are stopped.
As researchers improve allergy shots, they promise to become an even more effective treatment.
Are Researchers Studying Pollen Allergy?
Research on allergic diseases is a major area of emphasis for NIAID. The Institute supports laboratory and clinical studies related to pollen allergy at universities and research centers in the United States and abroad. The goal of NIAID’s allergic diseases program is to improve the understanding of the causes and development of these diseases and to help translate these findings into more effective methods of diagnosis, prevention, and treatment.
Food Allergies
Anaphylaxis
Problem foods
Similar medical problems
Diagnosis and treatment
More information on food allergies
About one in four people think that they are allergic to certain foods. In fact, only about 4 percent of persons age 5 and older actually have a food allergy.
In a true food allergy, your body's defense system, called the immune system, reacts to a certain food or food component as if it were a harmful substance. Symptoms of an allergic reaction to a food usually develop within a few minutes to an hour after eating the food.
If you are allergic to a particular food, you may first feel itching in your mouth as you start to eat the food.
Your nose could become stuffy or itchy.
You might start sneezing.
Your eyes could itch and develop tears.
You may get swelling of the lips, face, tongue, throat, or other parts of your body.
After the food reaches your stomach, you may have symptoms such as vomiting, diarrhea, or stomach cramps.
Your skin could become red, itchy, or develop a rash.
Anaphylaxis
For some people, an allergic reaction to a food is uncomfortable but not serious. For others, an allergic food reaction can lead to death. A life-threatening reaction caused by allergy is called anaphylaxis (an-uh-fuh-LAK-suhss). Symptoms of anaphylaxis include:
Hoarseness, throat tightness, or a lump in your throat
Wheezing, chest tightness, or having a hard time breathing
Rapid heart rate
Dizziness, lightheadedness, or fainting
Tingling in the hands, feet, lips, or scalp
Cold, clammy grayish or bluish skin
If you or someone you know is having these symptoms after eating something, call 9-1-1 right away. Anaphylaxis needs emergency treatment with a medicine called epinephrine (ep-uh-NEF-rin).
Problem Foods
In adults, the foods that most often cause allergic reactions include:
Shellfish, such as scallops, oysters, shrimp, crayfish, lobster, and crab
Peanuts
Tree nuts, such as walnuts, cashews, and pecans
Fish
Eggs
Similar medical problems
Other medical problems can have some of the same symptoms as a food allergy, such as:
Food poisoning from contaminated food or foods containing poisons, such as certain mushrooms
Lactose intolerance
Irritable bowel syndrome
Reactions to large amounts of some food additives, such as MSG (a flavor enhancer)
Diagnosis and treatment
If you have food allergy symptoms shortly after eating, see a doctor or allergist. If possible, see your doctor when the allergic reaction is occurring. This will help your doctor diagnose your problem.
The best treatment for a food allergy is to avoid eating the foods that cause your symptoms. This may require reading the ingredients on food labels to make sure that the foods don't contain anything that might cause you to have symptoms.
If you have anaphylactic reactions to certain foods, your doctor may give you a prescription for injectable epinephrine. You need to carry this medicine with you at all times so that you or someone you're with can give you an emergency injection if needed.
Source: NIAID, NIH
Cold, Flu, or Allergy? Tips and Treatments
|
Symptoms |
Cold |
Flu |
Airborne Allergy |
|
Fever |
Rare |
Usual, high (100-102 °F), sometimes higher, especially in young children); lasts 3-4 days |
Never |
|
Headache |
Uncommon |
Common |
Uncommon |
|
General Aches, Pains |
Slight |
Usual; often severe |
Never |
|
Fatigue, Weakness |
Sometimes |
Usual, can last up to 3 weeks |
Sometimes |
|
Extreme Exhaustion |
Never |
Usual, at the beginning of the illness |
Never |
|
Stuffy, Runny Nose |
Common |
Sometimes |
Common |
|
Sneezing |
Usual |
Sometimes |
Usual |
|
Sore Throat |
Common |
Sometimes |
Sometimes |
|
Cough |
Common |
Common, can become severe |
Sometimes |
|
Chest Discomfort |
Mild to moderate |
Common |
Rare, except for those with allergic asthma |
|
Treatment |
Get plenty of rest. |
Get plenty of rest. |
Avoid allergens (things that you’re allergic to) |
|
Prevention |
Wash your hands often. |
Get the flu vaccine each year. |
Avoid allergens, such as pollen, house dust mites, mold, pet dander, cockroaches. |
|
Complications |
Sinus infection middle ear infection, asthma |
Bronchitis, pneumonia; can be life-threatening |
Sinus infection, middle ear infection, asthma |
CONTACT US
NIH Office of Communications
and Public Liaison
Building 31, Room 5B64
Bethesda, MD 20892-2094
nihnewsinhealth@od.nih.gov
Tel: 301-402-7337
Managing Editor: Harrison Wein, Ph.D.
Editor: Vicki Contie
Contributors: Vicki Contie, Alan Defibaugh (illustrations), and Carol Torgan.
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
Sinus Infection (Sinusitis)
Content
Overview of a Sinus Infection
Causes
Signs and Symptoms
See a Healthcare Provider if...
Antibiotics are Needed When…
Antibiotics Will Not Help if...
How to Feel Better
Prevention
Overview of a Sinus Infection
Sinusitis, or a sinus infection, occurs when the sinuses and nasal passages become inflamed. If you or your child is diagnosed with sinusitis, the infection does not need to be treated with antibiotics unless you or your child has acute bacterial sinusitis, which is caused by bacteria. Acute bacterial sinusitis can last up to 4 weeks and subacute bacterial sinusitis can last 4 to 12 weeks, occurring less than 4 times per year.
Acute viral sinusitis, caused by a virus, typically lasts for less than 4 weeks and occurs less than 3 times per year. Acute viral sinusitis usually occurs after having an upper respiratory infection.
Chronic sinusitis typically lasts more than 4 weeks and occurs more than 4 times per year. If you are diagnosed with chronic sinusitis, you should visit a specialist for evaluation. Chronic sinusitis can be caused by nasal polyps or tumors, allergies, or respiratory tract infections (viral, bacterial, or fungal), among other reasons.
Causes of a Sinus Infection
Most sinus infections are caused by a virus
Sinus infections are rarely caused by bacteria
Other causes of sinusitis include:
Allergies
Pollutants (airborne chemicals or irritants)
Fungal infections
Structural problems within the nasal cavity
A weak immune system
Signs and Symptoms of a Sinus Infection
Headaches
Nasal congestion/discharge
Postnasal drip (mucus drips down the throat from the nose)
Sore throat
Fever
Cough
Fatigue
Bad breath
See a Healthcare Provider if You or Your Child has:
Temperature higher than 100.4° F
Symptoms that last more than 10 days
Multiple episodes of sinusitis in the past year
Symptoms that are not relieved with over-the-counter medicines
Your healthcare provider can determine if you or your child has sinusitis and if treatment is needed. If your child is younger than three months of age and has a fever, it’s important to always call your healthcare provider right away.
Antibiotics are Needed When…
Sometimes antibiotics may be needed if the sinus infection is likely to be caused by bacteria. By asking about your symptoms and doing a physical examination, a healthcare provider can determine if you or your child needs antibiotics.
Antibiotics Will Not Help if…
When sinusitis is caused by a virus or irritation in the air (like cigarette smoke), antibiotics will not help it get better. Acute sinusitis will almost always get better on its own. It is better to wait and take antibiotics only when they are needed. Taking antibiotics when they are not needed can be harmful, and may lead to unwanted side effects like diarrhea, rashes, nausea, and stomach pain. More severe side effects may rarely occur, including life-threatening allergic reactions, kidney toxicity, and severe skin reactions.
Each time you or your child takes an antibiotic, the bacteria that normally live in your body (on the skin, in the intestine, in the mouth and nose, etc.) are more likely to become resistant to antibiotics. Common antibiotics cannot kill infections caused by these resistant germs. Learn more about antibiotic resistance.
If symptoms continue for more than 10 days, schedule a follow-up appointment with a healthcare provider for re-evaluation to avoid any complications![]() .
.
How to Feel Better
Rest, over-the-counter medicines and other self-care methods may help you or your child feel better. For more information about symptomatic relief, visit the Symptom Relief section of this website or talk to your healthcare provider or pharmacist. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Preventing a Sinus Infection
Practice good hand hygiene
Keep you and your child up to date with recommended immunizations
Avoid close contact with people who have colds or other upper respiratory infections
Avoid smoking or exposure to second hand smoke and do not expose children to second hand smoke
Use a clean humidifier to moisten the air at home
Sore Throat
On this Page
Overview of a Sore Throat
Causes
Signs and Symptoms
See a Healthcare Provider if...
Antibiotics are Needed When…
Antibiotics Will Not Help if…
How to Feel Better
Prevention
Español: Dolor de garganta
Overview of a Sore Throat
A sore throat often makes it painful to swallow. A sore throat can also feel dry and scratchy. A sore throat is a frequent symptom of the common cold or other acute respiratory tract infections. In some cases, a lab test will need to be done to determine if you or your child needs antibiotics.
Causes of a Sore Throat
Most sore throats are caused by viruses, like ones that cause a cold or the flu
Some sore throats, like strep throat, are caused by bacteria; strep throat is caused by Group A streptococcus (strep-tuh-KOK-us)
Other causes include:
Allergies
Dry air
Pollution (airborne chemicals or irritants)
Smoking or exposure to second hand smoke
Signs and Symptoms of a Viral Infection Accompanied by a Sore Throat
Sneezing
Cough
Watery eyes
Mild headache
Mild body aches
Runny nose
Low-grade fever (less than 102°F)
See a Healthcare Provider if You or Your Child has:
A sore throat that lasts longer than 1 week
Difficulty swallowing or breathing
Excessive drooling (young children)
Temperature higher than 100.4° F
Pus on the back of the throat
Rash
Hoarseness![]() lasting longer than 2 weeks
lasting longer than 2 weeks
Blood in saliva or phlegm
Symptoms of dehydration (dry, sticky mouth, sleepiness or tiredness, thirst, decreased urination or fewer wet diapers, few or no tears when crying, muscle weakness, headache, dizziness or lightheadedness)
Contact with someone with strep throat
Recurring sore throats
Your healthcare provider can determine the cause of a sore throat and if treatment is needed. If your child is younger than three months of age and has a fever, it’s important to always call your healthcare provider right away.
Antibiotics are Needed When…
Antibiotics are needed if a healthcare provider diagnoses you or your child with strep throat, which is caused by bacteria. Strep throat cannot be diagnosed by looking in the throat – a lab test must also be done. Antibiotics are prescribed for strep throat for the purpose of preventing rheumatic fever![]() . If the test result shows strep throat, the infected patient should stay home from work, school, or day care until 24 hours after starting an antibiotic. For information about the bacteria that cause strep throat, visit CDC's Group A Streptococcal (strep-tuh-KOK-uhl) (GAS) Disease website.
. If the test result shows strep throat, the infected patient should stay home from work, school, or day care until 24 hours after starting an antibiotic. For information about the bacteria that cause strep throat, visit CDC's Group A Streptococcal (strep-tuh-KOK-uhl) (GAS) Disease website.
A healthcare provider may prescribe other medicine or give you tips to help with other symptoms like fever and cough, but antibiotics are not needed to treat most sore throats.
Antibiotics Will Not Help if…
When a sore throat is caused by a virus or irritation from the air, antibiotic treatment will not help it get better. Most sore throats will improve on their own within 1-2 weeks. It is important to take antibiotics only when they are needed. Taking antibiotics when they are not needed can be harmful, and may lead to unwanted side effects like diarrhea, rashes, nausea, and stomach pain. More severe side effects may rarely occur, including life-threatening allergic reactions, kidney toxicity, and severe skin reactions.
Each time you or your child takes an antibiotic, the bacteria that normally live in the body (on the skin, in the intestine, in the mouth and nose, etc.) are more likely to become resistant to antibiotics. Common antibiotics cannot kill infections caused by these resistant germs. Learn more about antibiotic resistance.
How to Feel Better
Rest, over-the-counter medicines and other self-care methods may help you or your child feel better. For more information about symptomatic relief, visit the Symptom Relief section of this website or talk to your healthcare provider or pharmacist. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Preventing a Sore Throat
Practice good hand hygiene
Avoid close contact with people who have colds or other upper respiratory infections
Avoid smoking
Avoid exposure to second hand smoke and do not expose children to second hand smoke
Common Cold and Runny Nose
On this Page
Overview
Causes
Signs and Symptoms
See a Healthcare Provider if...
Antibiotics are Needed When...
Antibiotics Will Not Help if...
How to Feel Better
Prevention
Español: El resfriado común y la secreción nasal o moqueo
Overview of Common Cold
A cold usually includes a runny nose, sore throat, sneezing, and coughing. These symptoms can last for up to two weeks.
Causes
Common Cold
Over 200 viruses can cause the common cold
The rhinovirus is the most common type of virus that causes colds
Runny Nose during a Cold
When germs that cause colds first infect the nose and sinuses, the nose makes clear mucus. This helps wash the germs from the nose and sinuses. After two or three days, the body's immune cells fight back, changing the mucus to a white or yellow color. As the bacteria that live in the nose grow back, they may also be found in the mucus, which changes the mucus to a greenish color. This is normal and does not mean you or your child needs antibiotics.
Signs and Symptoms of the Common Cold
Sneezing
Stuffy or runny nose
Sore throat
Coughing
Watery eyes
Mild headache
Mild body aches
See a Healthcare Provider if You or Your Child has:
Temperature higher than 100.4° F
Symptoms that last more than 10 days
Symptoms that are not relieved by over-the-counter medicines
Your healthcare provider can determine if you or your child has a cold and can recommend symptomatic therapy. If your child is younger than three months of age and has a fever, it’s important to always call your healthcare provider right away.
Antibiotics are Needed When…
Antibiotics are needed only if your healthcare provider tells you that you or your child has a bacterial infection. Your healthcare provider may prescribe other medicine or give tips to help with a cold's symptoms, but antibiotics are not needed to treat a cold or runny nose.
Antibiotics Will Not Help if…
Since the common cold is caused by a virus, antibiotics will not help it get better. A runny nose or cold almost always gets better on its own, so it is better to wait and take antibiotics only when they are needed. Taking antibiotics when they are not needed can be harmful, and may lead to unwanted side effects like diarrhea, rashes, nausea, and stomach pain. More severe side effects may rarely occur, including life-threatening allergic reactions, kidney toxicity, and severe skin reactions.
Each time you or your child takes an antibiotic, the bacteria that normally live in your body (on the skin, in the intestine, in the mouth and nose, etc.) are more likely to become resistant to antibiotics. Common antibiotics cannot kill infections caused by these resistant germs. Learn more about antibiotic resistance.
How to Feel Better
Rest, over-the-counter medicines and other self-care methods may help you or your child feel better. For more information about symptomatic relief, visit the Symptom Relief section of this website or talk to your healthcare provider or pharmacist. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Preventing the Common Cold
Practice good hand hygiene
Avoid close contact with people who have colds or other upper respiratory infections
Ear Infections
On this Page
Overview of Ear Infections
Causes
Signs and Symptoms
See a Healthcare Provider if...
Antibiotics are Needed When…
Antibiotics Might Not Help if…
How to Feel Better
Prevention
Español: Infecciones del oído
Overview of Ear Infections
There are three main kinds of ear infections, which are called acute otitis (oh-TIE-tus) media (AOM), otitis media with effusion (uh-FEW-zhun) (OME), and otitis externa (Swimmer’s Ear). Sometimes ear infections can be painful and may even need antibiotics. Your healthcare provider will be able to determine what kind of ear infection you or your child has and if antibiotics would help.
Acute otitis media
The type of ear infection that is usually painful and may improve with antibiotic treatment is called acute otitis (oh-TIE-tus) media, or AOM. Symptoms of AOM include pain, redness of the eardrum, pus in the ear, and fever. Children may pull on the affected ear, and infants or toddlers may be irritable. Antibiotics are often prescribed to children for AOM, but are not always necessary.
Otitis media with effusion
Otitis media with effusion (uh-FEW-zhun), or OME, is a build up of fluid in the middle ear without signs and symptoms of acute infection (pain, redness of the eardrum, pus, and fever). OME is more common than AOM, and may be caused by viral upper respiratory infections, allergies, or exposure to irritants (such as cigarette smoke). The build up of fluid in the middle ear does not usually cause pain and almost always goes away on its own. OME will not usually benefit from antibiotic treatment.
Otitis externa (Swimmer’s Ear)
Otitis externa, more commonly known as Swimmer's Ear, is an infection of the ear and/or outer ear canal. It can cause the ear to itch or become red and swollen so that touching of or pressure on the ear is very painful. There may also be pus that drains from the ear. Antibiotics are usually needed to treat otitis externa. For more information about symptoms, treatment, causes, and prevention of Swimmer's Ear, visit CDC's Healthy Swimming website.
Causes of Ear Infections
Acute otitis media (AOM)
AOM is often caused by bacteria, but can also be caused by viruses. The bacteria that usually cause AOM are Streptococcus pneumoniae (strep-toh-KOK-us KNEW-moh-NEE-ay), Haemophilus influenzae (he-MO-fill-us in-flu-EN-zay), and Moraxella catarrhalis (more-ax-EL-la ka-tar-HUL-iss). The viruses that most commonly cause AOM are respiratory syncytial (sin-SIH-shull) virus (RSV), rhinoviruses, influenza viruses, and adenoviruses.
Otitis media with effusion (OME)
The part of the ear that gets blocked by fluid is called the eustachian (you-STAY-shun) tube, which connects the inside of the ear to the back of the throat. Fluid may build up in the middle ear for several reasons. When you or your child has a cold, the middle ear can get filled with fluid just as the nose does - it just doesn't run out as easily from the middle ear. Sometimes the fluid becomes infected, leading to AOM. After an episode of AOM has been treated with antibiotics or has resolved on its own, fluid may remain in the middle ear and may take a month or longer to go away.
Signs and Symptoms of Ear Infections
Acute otitis media (AOM)
Pulling at ears
Excessive crying
Fluid draining from ears
Sleep disturbances
Fever
Headaches
Problems with hearing
Irritability
Difficulty balancing
Otitis media with effusion (OME)
Problems with hearing
See a Healthcare Provider if You or Your Child has:
Temperature higher than 100.4° F
Discharge of blood or pus from the ears
Been diagnosed with an ear infection and symptoms do not improve, or worsen
Your healthcare provider can determine what kind of ear infection is present and if treatment is needed. If your child is younger than three months of age and has a fever, it’s important to always call your healthcare provider right away.
Antibiotics are Needed When…
Acute otitis media (AOM)
Your healthcare provider will consider several factors when determining if antibiotics are needed for you or your child: age, severity of illness, diagnostic certainty, and follow-up options. Your healthcare provider may decide to wait a couple of days before prescribing antibiotics since you or your child may get better without them.
To learn more about how healthcare providers determine when to prescribe antibiotics for ear infections, visit websites of the American Academy of Pediatrics![]() and the American Academy of Family Physician
and the American Academy of Family Physician
Antibiotics Might Not Help if…
When an ear infection is caused by a virus, antibiotic treatment will not help it get better. Ear infections will often get better on their own without antibiotic treatment. Your healthcare provider will determine what treatment is best for you or your child. Taking antibiotics when they are not needed can be harmful, and may lead to unwanted side effects like diarrhea, rashes, nausea, and stomach pain. More severe side effects may rarely occur; these include life-threatening allergic reactions, kidney toxicity, and severe skin reactions.
Each time you or your child takes an antibiotic, the bacteria that normally live in your body (on the skin, in the intestine, in the mouth and nose, etc.) are more likely to become resistant to antibiotics. Common antibiotics cannot kill infections caused by these resistant germs. Learn more about antibiotic resistance.
If symptoms continue to last for more than one month for OME or 2 days for AOM, you should schedule a follow-up appointment with your healthcare provider.
How to Feel Better
Rest, over-the-counter medicines and other self-care methods may help you or your child feel better. For more information about symptomatic relief, visit the Symptom Relief section of this website or talk to your healthcare provider or pharmacist. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Preventing Ear Infections
Avoid smoking or exposure to second hand smoke and do not expose children to second hand smoke
Avoid exposure to air pollution
Keep you and your child up to date with recommended immunizations
Breastfeed your baby for 12 months or more if possible
Bottle feed your baby in the upright position
Bronchitis (Chest Cold)
On this Page
Overview of Bronchitis
Causes
Signs and Symptoms
See a Healthcare Provider if...
Antibiotics are Needed When...
Antibiotics Will Not Help if...
How to Feel Better
Prevention
Español: Bronquitis (resfriado del pecho)
Overview of Bronchitis
Acute bronchitis (brahn-KITE-uss), or chest cold, is a condition that occurs when the bronchial (BRAHN-kee-uhl) tubes in the lungs become inflamed. The bronchial tubes swell and produce mucus, which causes a person to cough. This often occurs after an upper respiratory infection like a cold. Most symptoms of acute bronchitis (chest pain, shortness of breath, etc.) last for up to 2 weeks, but the cough can last for up to 8 weeks in some people.
Chronic bronchitis lasts a long time, and is more common among smokers. People with chronic bronchitis have a cough with mucus most days for 3 months a year for 2 consecutive years. If you have been diagnosed with chronic bronchitis, you should visit a specialist to be evaluated.
Visit the American Academy of Family Physicians' website to learn more about acute bronchitis![]() .
.
Another kind of lung infection that parents should know about is bronchiolitis (BRAHN-kee-oh-LIE-tus). Infants can be diagnosed with bronchiolitis, a viral infection, which can obstruct the small airways and may require treatment. Learn more about bronchiolitis by visiting the National Institutes for Health website![]()
Causes of Bronchitis
Several types of viruses, most often:
Respiratory syncytial (sin-SIH-shull) virus (RSV)
Adenovirus
Influenza
Parainfluenza
Bacteria, in rare cases
Pollutants (airborne chemicals or irritants)
Signs and Symptoms of Bronchitis
Cough that produces mucus (may be without mucus the first few days)
Soreness in the chest
Fatigue
Mild headache
Mild body aches
Low-grade fever (less than 102°F)
Watery eyes
Sore throat
See a Healthcare Provider if You or Your Child has:
Temperature higher than 100.4° F
A fever and cough with thick or bloody mucus
A chronic heart or lung problem
Shortness of breath or trouble breathing
Symptoms that last more than 3 weeks
Repeated episodes of bronchitis/bronchiolitis
If your child is younger than three months of age and has a fever, it’s important to always call your healthcare provider right away.
Your healthcare provider can determine if you or your child has acute bronchitis, chronic bronchitis, bronchiolitis, or another type of respiratory infection. Then a decision can be made about possible needed treatment.
Antibiotics are Needed When…
Antibiotics will rarely be needed since acute bronchitis and bronchiolitis are almost always caused by a virus and chronic bronchitis requires other therapies. However, treatment may be prescribed to relieve symptoms. If your healthcare provider diagnoses you or your child with another type of respiratory infection such as pneumonia (knew-MOHN-ya) or whooping cough (pertussis: purr-TUSS-uss), antibiotics will most likely be prescribed.
Antibiotics Will Not Help if…
When bronchitis is caused by a virus or irritation in the air (like cigarette smoke) , antibiotic treatment will not help it get better. Since acute bronchitis almost always gets better on its own, it is better to wait and take antibiotics only when they are needed. Taking antibiotics when they are not needed can be harmful, and may lead to unwanted side effects like diarrhea, rashes, nausea, and stomach pain. More severe side effects may rarely occur, including life-threatening allergic reactions, kidney toxicity, and severe skin reactions.
Each time you or your child takes an antibiotic, the bacteria that normally live in your body (on the skin, in the intestine, in the mouth and nose, etc.) are more likely to become resistant to antibiotics. Common antibiotics cannot kill infections caused by these resistant germs. Learn more about antibiotic resistance.
How to Feel Better
Rest, over-the-counter medicines and other self-care methods may help you or your child feel better. For more information about symptomatic relief, visit the Symptom Relief section of this website or talk to your healthcare provider or pharmacist. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Preventing Acute Bronchitis
Avoid smoking
Avoid exposure to second hand smoke and do not expose children to second hand smoke
Practice good hand hygiene
Keep you and your child up to date with recommended immunizations
Symptom Relief
On this Page
Overview
How to Feel Better
Over-the-Counter (OTC) Medicines
Questions and Answers for Parents about Over-the-Counter (OTC) Medicines
Related Materials
Español: Alivio de síntomas
Overview
Children and adults with viral infections, which antibiotics cannot treat, usually recover when the illness has run its course. Colds, a type of viral infection, can last for up to two weeks. You should keep your healthcare provider informed if your or your child’s illness gets worse or lasts longer than expected. Over-the-counter medicines may help relieve some symptoms.
How to Feel Better
What can I do to feel better if antibiotics won’t treat my illness because it’s caused by a virus?
For upper respiratory infections, such as sore throats, ear infections, sinus infections, colds, and bronchitis, try the following:
Get plenty of rest
Drink plenty of fluids
Use a clean humidifier![]() or cool mist vaporizer
or cool mist vaporizer
Avoid smoking, second-hand smoke, and other pollutants (airborne chemicals or irritants)
Take acetaminophen, ibuprofen or naproxen to relieve pain or fever (read about what is safe to give your child)
For children and adults, over-the-counter pain relievers, decongestants and saline nasal sprays may help relieve some symptoms. Remember, always use over-the-counter products as directed. Many over-the-counter products are not recommended for children younger than certain ages.
Over-the-counter medicines may help relieve symptoms such as runny nose, congestion, fever and aches, but they do not shorten the length of time you or your child is sick.
Learn more by reading below about over-the-counter medicines. Here are some helpful tips for how to feel better depending on how you or your child feels.
Sore Throat
Soothe a sore throat with ice chips, sore throat spray, or lozenges (do not give lozenges to young children)
Use a clean humidifier or cool mist vaporizer
Take acetaminophen, ibuprofen or naproxen to relieve pain or fever (read about what is safe to give your child)
Ear Pain
Put a warm moist cloth over the ear that hurts
Take acetaminophen, ibuprofen or naproxen to relieve pain or fever (read about what is safe to give your child)
Runny Nose
Use a decongestant or saline nasal spray to help relieve nasal symptoms (read about what is safe to give your child)
Sinus Pain/Pressure
Put a warm compress over the nose and forehead to help relieve sinus pressure
Use a decongestant or saline nasal spray
Breathe in steam from a bowl of hot water or shower
Take acetaminophen, ibuprofen or naproxen to relieve pain or fever (read about what is safe to give your child)
Cough
Use a clean humidifier or cool mist vaporizer or breathe in steam from a bowl of hot water or shower (read about what is safe to give your child)
Over-the-Counter (OTC) Medicines
For children and adults, over-the-counter pain relievers, decongestants and saline nasal sprays may help relieve some symptoms. Remember, always use over-the-counter products as directed. Not all products are recommended for children younger than certain ages. Overuse and misuse of OTC cough and cold medicines in young children can result in serious and potentially life-threatening side effects.
These medicines may help relieve symptoms such as runny nose, congestion, fever and aches, but they do not shorten the length of time you or your child is sick.
More information is available about pain relievers![]() (National Institutes of Health), decongestants
(National Institutes of Health), decongestants![]() (American Academy of Family Physicians), nasal wash treatment
(American Academy of Family Physicians), nasal wash treatment![]() (National Jewish Health), and humidifiers
(National Jewish Health), and humidifiers![]() (Humidifier Health).
(Humidifier Health).
Questions and Answers for Parents about Over-the-Counter (OTC) Medicines
For adults, over-the-counter pain relievers, decongestants and saline nasal sprays may help relieve some symptoms. Remember, always use over-the-counter products as directed.
For children, over-the-counter pain relievers, decongestants and saline nasal sprays may help relieve some symptoms. Not all products are recommended for children of certain ages.
These medicines may help relieve symptoms such as runny nose, congestion, fever and aches, but they do not shorten the length of time you or your child is sick.
Q: What pain relievers can I give my child?
A: For babies 6 months of age or younger, parents should only give acetaminophen for pain relief. For a child 6 months of age or older, either acetaminophen or ibuprofen can be given for pain relief. Be sure to ask your child’s healthcare provider for the right dosage for your child’s age and size. Do not give aspirin to your child because of Reye's syndrome, a rare but very serious illness that harms the liver and brain. Learn more about Reye’s syndrome![]() .
.
Q: Should parents give cough and cold medicines to young children?
A: The Consumer Healthcare Products Association (CHPA), a group that represents most of the makers of nonprescription over-the-counter (OTC) cough and cold medicines, recommends that these products not be used in children under 4 years of age. The Food and Drug Administration (FDA)![]() supports this recommendation. Overuse and misuse of OTC cough and cold medicines in young children can result in serious and potentially life-threatening side effects.
supports this recommendation. Overuse and misuse of OTC cough and cold medicines in young children can result in serious and potentially life-threatening side effects.
Q: What can parents do to help their children feel better if they are too young to take cough and cold medicines or the healthcare provider advises against using them?
A: Parents might consider clearing nasal congestion in infants with a rubber suction bulb. Also, a stuffy nose can be relieved with saline nose drops or a clean humidified or cool-mist vaporizer.
Q: Should parents give cough and cold medicines to children over 4 years of age?
A: Cough and cold symptoms usually go away without treatment after a certain amount of time. Over-the-counter cough and cold medicines will not cure the common cold, but may give some temporary relief of symptoms. Parents should consult their child’s healthcare provider if they have any concerns or questions about giving their child a medication. Parents should always tell their child’s healthcare provider about all prescription and over-the-counter medicines they are giving their child.
Q: What should parents and doctors be careful of if they want to give cough and cold medicines to children over 4 years of age?
A: Always keep medications in original bottles or containers, with the cap secure, and up and away from children. Children getting into and taking medications without adult supervision can lead to serious and potentially life-threatening effects. Avoid giving more than one cough and cold medicine at a time to children. Two medicines may have different brand names but may contain the same ingredient. Some cough and cold medicines contain more than one active ingredient. Also, follow directions carefully to avoid giving too much medication; the right amount of medication often depends on your child’s age and weight.
What Everyone Should Know and Do
Snort. Sniffle. Sneeze. No Antibiotics Please!
Content
If You Have a Cold or Flu, Antibiotics Won't Work For You!
What Can You Do To Protect Yourself Or Your Child?
Are you aware that colds, flu, most sore throats, and bronchitis are caused by viruses? Did you know that antibiotics do not help fight viruses? It's true. Plus, taking antibiotics when you have a virus may do more harm than good. Taking antibiotics when they are not needed increases your risk of getting an infection later that resists antibiotic treatment.
If You Have a Cold or Flu, Antibiotics Won't Work For You!
Get Smart…Read The Chart! [1 page] to know which common illnesses are usually viral or bacterial and when antibiotics are necessary.
Antibiotics cure bacterial infections, not viral infections such as:
Colds or flu;
Most coughs and bronchitis;
Sore throats not caused by strep; or
Runny noses.
Taking antibiotics for viral infections, such as a cold, cough, the flu, or most bronchitis, will not:
Cure the infections;
Keep other individuals from catching the illness; or
Help you feel better.
What Can You Do To Protect Yourself Or Your Child?
When you use antibiotics appropriately, you do the best for your health, your family's health, and the health of those around you. "We want Americans to keep their families and communities healthy by getting smart about the proper use of antibiotics," said Lauri Hicks, D.O., medical director of CDC's Get Smart campaign.
What To Do
Talk with your healthcare provider about antibiotic resistance.
When you are prescribed an antibiotic,
Take it exactly as the doctor tells you. Complete the prescribed course even if you are feeling better. If treatment stops too soon, some bacteria may survive and re-infect you.
This goes for children, too. Make sure your children take all medication as prescribed, even if they feel better.
Throw away any leftover medication once you have completed your prescription
What Not To Do
Antibiotics cure bacteria, not viruses such as:
Colds or flu;
Most coughs and bronchitis;
Sore throats not caused by strep; or
Runny noses.
Antibiotic Resistance Questions & Answers
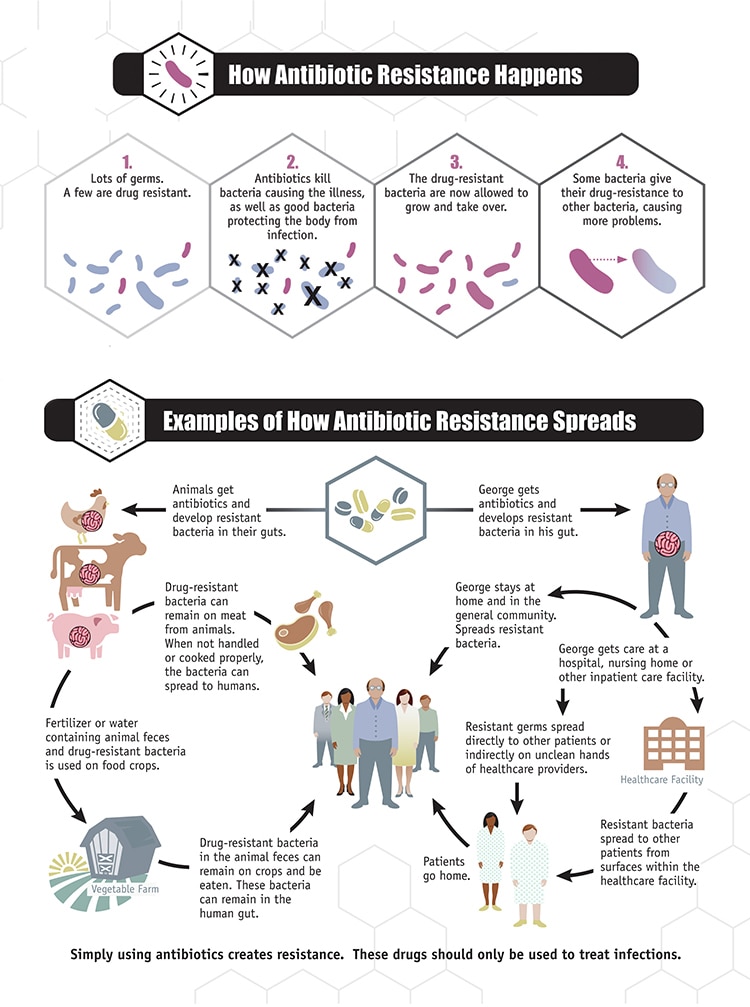
Click for larger view ![]() [PDF - 114 pages]
[PDF - 114 pages]
On this Page
Questions about Bacteria, Viruses, and Antibiotics
Questions about Antibiotic Resistance
Questions about Antibacterial Cleaning Agents, Acne Medication, and Probiotics
Questions about Bacteria, Viruses, and Antibiotics
Q: What are bacteria and viruses?
A: Bacteria are single-celled organisms usually found all over the inside and outside of our bodies, except in the blood and spinal fluid. Many bacteria are not harmful. In fact, some are actually beneficial. However, disease-causing bacteria trigger illnesses, such as strep throat and some ear infections. Viruses are even smaller than bacteria. A virus cannot survive outside the body's cells. It causes illnesses by invading healthy cells and reproducing.
Q: What kinds of infections are caused by viruses and should not be treated with antibiotics?
A: Viral infections that should not be treated with antibiotics include:
Colds
Flu
Most coughs and bronchitis
Sore throats (except for those resulting from strep throat)
Some ear infections
Q: What is an antibiotic?
A: Antibiotics, also known as antimicrobial drugs, are drugs that fight infections caused by bacteria. Alexander Fleming discovered the first antibiotic, penicillin, in 1928. After the first use of antibiotics in the 1940s, they transformed medical care and dramatically reduced illness and death from infectious diseases.
The term "antibiotic" originally referred to a natural compound produced by a fungus or another microorganism that kills bacteria which cause disease in humans or animals. Some antibiotics may be synthetic compounds (not produced by microorganisms) that can also kill or inhibit the growth of microbes. Technically, the term "antimicrobial agent" refers to both natural and synthetic compounds; however, many people use the word "antibiotic" to refer to both. Although antibiotics have many beneficial effects, their use has contributed to the problem of antibiotic resistance.
Questions about Antibiotic Resistance
Q: What is antibiotic resistance?
A: Antibiotic resistance is the ability of bacteria or other microbes to resist the effects of an antibiotic. Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. The bacteria survive and continue to multiply causing more harm.
Q: Why should I be concerned about antibiotic resistance?
A: Antibiotic resistance has been called one of the world's most pressing public health problems. Almost every type of bacteria has become stronger and less responsive to antibiotic treatment when it is really needed. These antibiotic-resistant bacteria can quickly spread to family members, schoolmates, and co-workers - threatening the community with a new strain of infectious disease that is more difficult to cure and more expensive to treat. For this reason, antibiotic resistance is among CDC's top concerns.
Antibiotic resistance can cause significant danger and suffering for children and adults who have common infections, once easily treatable with antibiotics. Microbes can develop resistance to specific medicines. A common misconception is that a person's body becomes resistant to specific drugs. However, it is microbes, not people, that become resistant to the drugs.
If a microbe is resistant to many drugs, treating the infections it causes can become difficult or even impossible. Someone with an infection that is resistant to a certain medicine can pass that resistant infection to another person. In this way, a hard-to-treat illness can be spread from person to person. In some cases, the illness can lead to serious disability or even death.
Q: Why are bacteria becoming resistant to antibiotics?
A: Antibiotic use promotes development of antibiotic-resistant bacteria. Every time a person takes antibiotics, sensitive bacteria are killed, but resistant germs may be left to grow and multiply. Repeated and improper uses of antibiotics are primary causes of the increase in drug-resistant bacteria.
While antibiotics should be used to treat bacterial infections, they are not effective against viral infections like the common cold, most sore throats, and the flu. Widespread use of antibiotics promotes the spread of antibiotic resistance. Smart use of antibiotics is the key to controlling the spread of resistance.
Antibiotics kill bacteria, not viruses
Q: How do bacteria become resistant to antibiotics?
A: Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. The bacteria survive and continue to multiply causing more harm. Bacteria can do this through several mechanisms. Some bacteria develop the ability to neutralize the antibiotic before it can do harm, others can rapidly pump the antibiotic out, and still others can change the antibiotic attack site so it cannot affect the function of the bacteria.
Antibiotics kill or inhibit the growth of susceptible bacteria. Sometimes one of the bacteria survives because it has the ability to neutralize or escape the effect of the antibiotic; that one bacterium can then multiply and replace all the bacteria that were killed off. Exposure to antibiotics therefore provides selective pressure, which makes the surviving bacteria more likely to be resistant. In addition, bacteria that were at one time susceptible to an antibiotic can acquire resistance through mutation of their genetic material or by acquiring pieces of DNA that code for the resistance properties from other bacteria. The DNA that codes for resistance can be grouped in a single easily transferable package. This means that bacteria can become resistant to many antimicrobial agents because of the transfer of one piece of DNA.
The Food and Drug Administration's (FDA's) Center for Veterinary Medicine (CVM) produced a nine-minute animation![]() explaining how antimicrobial resistance both emerges and proliferates among bacteria. Over time, the use of antimicrobial drugs will result in the development of resistant strains of bacteria, complicating clinicians' efforts to select the appropriate antimicrobial for treatment.
explaining how antimicrobial resistance both emerges and proliferates among bacteria. Over time, the use of antimicrobial drugs will result in the development of resistant strains of bacteria, complicating clinicians' efforts to select the appropriate antimicrobial for treatment.
Q: How can I prevent antibiotic-resistant infections?
Only use antibiotics when they are likely to be beneficial
A: By visiting this website, you are taking the first step to reducing your risk of getting antibiotic-resistant infections. It is important to understand that, although they are very useful drugs, antibiotics designed for bacterial infections are not useful for viral infections such as a cold, cough, or the flu. Some useful tips to remember are:
Talk with your healthcare provider about antibiotic resistance:Do not take an antibiotic for a viral infection like a cold or the flu.
Ask whether an antibiotic is likely to be beneficial for your illness
Ask what else you can do to feel better sooner
Do not save some of your antibiotic for the next time you get sick. Discard any leftover medication once you have completed your prescribed course of treatment.
Take an antibiotic exactly as the healthcare provider tells you. Do not skip doses. Complete the prescribed course of treatment even if you are feeling better. If treatment stops too soon, some bacteria may survive and re-infect.
Do not take antibiotics prescribed for someone else. The antibiotic may not be appropriate for your illness. Taking the wrong medicine may delay correct treatment and allow bacteria to multiply.
If your healthcare provider determines that you do not have a bacterial infection, ask about ways to help relieve your symptoms. Do not pressure your provider to prescribe an antibiotic.
Q: How can healthcare providers help prevent the spread of antibiotic resistance?
A: Prevent the spread of antibiotic resistance by
Only prescribe antibiotic therapy when likely to be beneficial to the patient
Use an agent targeting the likely pathogens
Use the antibiotic for the appropriate dose and duration
View CDC's Adult and Pediatric Academic Detailing Sheets for providers
Questions about Antibacterial Cleaning Agents, Acne Medication, and Probiotics
Q: Are antibacterial-containing products (soaps, household cleaners, etc.) better for preventing the spread of infection? Does their use add to the problem of resistance?
A: An essential part of preventing the spread of infection in the community and at home is proper hygiene. This includes handwashing and cleaning shared items and surfaces. Using soap to wash hands is more effective than using water alone because the surfactants in soap lift soil and microbes from skin, and people tend to scrub hands more thoroughly when using soap, which further removes germs. To date, studies have shown that there is no added health benefit for consumers (this does not include professionals in the healthcare setting) using soaps containing antibacterial ingredients compared with using plain soap. A link between antibacterial chemicals used in personal cleaning products and bacterial resistance has been shown in vitro studies (in a controlled environment).
FDA released a proposed rule![]() in December 2013 to require manufacturers to submit data showing the data supporting the efficacy and safety of antibacterial soaps and body washes. View the related press release
in December 2013 to require manufacturers to submit data showing the data supporting the efficacy and safety of antibacterial soaps and body washes. View the related press release![]() and consumer updates on antibacterial soap
and consumer updates on antibacterial soap![]() and the common ingredient triclosan
and the common ingredient triclosan![]() . This proposed rule does not affect hand sanitizers, wipes, or antibacterial products used in healthcare settings. CDC looks forward to any future data about the safety and effectiveness of antibacterial consumer products and will continue to adjust recommendations based on the best available science.
. This proposed rule does not affect hand sanitizers, wipes, or antibacterial products used in healthcare settings. CDC looks forward to any future data about the safety and effectiveness of antibacterial consumer products and will continue to adjust recommendations based on the best available science.
Suggested readings:
Weber JT, Hughes JM. Beyond Semmelweis: Moving Infection Control into the Community![]() . Ann Intern Med. 2004;140:397-398.
. Ann Intern Med. 2004;140:397-398.
Larson EL, Lin SX, Gomez-Pichardo C, Della-Latta P. Effect of antibacterial home cleaning and handwashing products on infectious disease symptoms: a randomized, double-blind trial![]() . Ann Intern Med. 2004;140(5):321-9.
. Ann Intern Med. 2004;140(5):321-9.
Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, Hoekstra RM. Effect of handwashing on child health: a randomised controlled trial![]() . Lancet. 2005;366:225-33.
. Lancet. 2005;366:225-33.
Luby SP, Agboatwalla M, Painter J, Altaf A, Billhimer WL, Hoekstra RM. Effect of intensive handwashing promotion on childhood diarrhea in high-risk communities in Pakistan: a randomized controlled trial![]() . JAMA. 2004;291(21):2547-54.
. JAMA. 2004;291(21):2547-54.
Q: Can antibiotic resistance develop from acne medication?
A: Antibiotic use, appropriate or otherwise, contributes to the development of antibiotic resistance. This is true for acne medications that contain antibiotics. Short and long-term use of antibiotics for treatment or prevention of bacterial infections should be under the direction of a physician to ensure appropriate use and detection of resistance.
Q: Do probiotics have a role in preventing or treating drug resistance or drug-resistant infections?
A: Probiotics are defined as microorganisms that when administered in sufficient quantities may improve health. There are a variety of probiotics that have been studied for various health benefits. Their role in preventing drug-resistant infections in humans has not been established. CDC is currently monitoring research on probiotic use, but cannot make any recommendations at this time.
Fast Facts
On this Page
Facts About Antibiotic Resistance
Antibiotic Prescribing: Attitudes, Behaviors, Trends & Cost
Facts About Antibiotic Resistance
Antibiotic resistance has been called one of the world’s most pressing public health problems.
The number of bacteria resistant to antibiotics has increased in the last decade. Many bacterial infections are becoming resistant to the most commonly prescribed antibiotic treatments.
Every time a person takes antibiotics, sensitive bacteria are killed, but resistant germs may be left to grow and multiply. Repeated and improper uses of antibiotics are primary causes of the increase in drug-resistant bacteria.
Know the Facts?

Download 6 color fact sheets that address smart use of antibiotics.
Misuse of antibiotics jeopardizes the usefulness of essential drugs. Decreasing inappropriate antibiotic use is the best way to control resistance.
Children are of particular concern because they have the highest rates of antibiotic use.
Antibiotic resistance can cause significant danger and suffering for people who have common infections that once were easily treatable with antibiotics. When antibiotics fail to work, the consequences are longer-lasting illnesses, more doctor visits or extended hospital stays, and the need for more expensive and toxic medications. Some resistant infections can even cause death.
Antibiotic Prescribing: Attitudes, Behaviors, Trends & Cost
Parent pressure makes a difference. For pediatric care, a study showed that doctors prescribe antibiotics 62% of the time if they perceive parents expect them and 7% of the time if they feel parents do not expect them.
Antibiotics were prescribed in 68% of acute respiratory tract visits – and of those, 80% were unnecessary according to CDC guidelines.
National Ambulatory Medical Care Survey (NAMCS) data shows that overall antibiotic prescribing dropped from 13.8 prescriptions per 100 office visits to 12.0 prescriptions per 100 office visits comparing 1997-98 to 2005-06 with a 13% reduction in overall antimicrobial prescribing.
According to NAMCS, the Get Smart Campaign contributed to a reduction in antimicrobials prescribed for children [4]
Among children younger than 5 years, annual ARTI (acute respiratory tract infections) visit rates decreased by 17% from 1883 per 1000 population in 1995-96 to 1560 per 1000 population in 2005-06, primarily due to a 33% decrease in visit rates for otitis media.
$1.1 billion is spent annually on unnecessary adult upper respiratory infection antibiotic prescriptions.
Get Smart has contributed to 25% reduction in antimicrobial use per outpatient office visit for presumed viral infections (NAMCS); intervention studies show a reduction of 8 to 26% for antibiotic prescriptions.
Partial References
Mangione-Smith R, McGlynn EA, Elliott MN, et al: The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics 103:711-718, 1999.
Scott JG, Cohen D, DiCicco-Bloom B, Orzano AJ, et al: Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Pract: 50(10): 853-8, 2001.
National Ambulatory Medical Care Survey (NAMCS).
Glossary
The terms defined on this page are commonly used throughout the Get Smart site.
Adverse drug events
When therapeutic drugs (example, antibiotics) have injurious effects; when someone has been harmed by a medication.
Antibiotic
Type of antimicrobial agent made from a mold or a bacterium that kills, or slows the growth of other microbes, specifically bacteria. Examples include penicillin and streptomycin.
Antimicrobial agents
A general term for the drugs, chemicals, or other substances that either kill or slow the growth of microbes. Among the antimicrobial agents in use today are antibacterial drugs (which kill bacteria), antiviral agents (which kill viruses), antifungal agents (which kill fungi), and antiparisitic drugs (which kill parasites).
Antimicrobial resistance
Antimicrobial resistance is the result of microbes changing in ways that reduce or eliminate the effectiveness of drugs, chemicals, or other agents to cure or prevent infections.
Bacteria
Bacteria are single-celled organisms that live in and around us. Bacteria may be helpful, but in certain conditions may cause illnesses such as strep throat, most ear infections, and bacterial pneumonia.
Bacterium
The singular form of bacteria.
Drug resistance
Drug resistance is the result of microbes changing in ways that reduce or eliminate the effectiveness of drugs, chemicals, or other agents to cure or prevent infections.
Epidemiology
The study of the spread of diseases. Epidemiologists are often sent to investigate outbreaks.
Fungi
Single-celled or multicellular organisms. Fungi can be either opportunistic pathogens (such as aspergillosis, candidiasis, and cryptococcosis) that cause infections in immunocompromised persons (including cancer patients, transplant recipients, and persons with AIDS) or pathogens (such as the endemic mycoses, histoplasmosis and coccidioidomycosis, and superficial mycoses) that cause infections in healthy persons. Fungi are also used for the development of antibiotics, antitoxins, and other drugs used to control various human diseases.
Immunization
The process or procedure by which a subject (person, animal, or plant) is rendered immune, or resistant to a specific disease. This term is often used interchangeably with vaccination or inoculation, although the act of inoculation does not always result in immunity.
Infection
An invasion of an organism by a pathogen such as bacteria or viruses. Some infections lead to disease.
Long-term care facility
A long-term care facility is a facility that provides rehabilitative, restorative, and/or ongoing skilled nursing care to patients or residents in need of assistance with activities of daily living. Long-term care facilities include nursing homes, rehabilitation facilities, inpatient behavioral health facilities, and long-term chronic care hospitals.
Microbes
Organisms so small that a microscope is required to see them. Microbes are also called microorganisms.
Nosocomial
Referring to an infection acquired by a patient while in a hospital.
Organism
Any living thing. Organisms include humans, animals, plants, bacteria, protozoa, and fungi.
Parasites
Any organism that lives in or on another organism without benefiting the host organism; commonly refers to pathogens, most commonly in reference to protozoans and helminths.
Pathogens
Bacteria, viruses, parasites, or fungi that can cause disease.
Surveillance Systems
The ongoing systematic collection and analysis of data. The data may lead to actions taken to prevent and control an infectious disease.
Virus
A strand of DNA or RNA in a protein coat that must get inside a living cell to grow and reproduce. Viruses cause many types of illness; for example, varicella virus causes chickenpox, and the human immunodeficiency virus (HIV) causes the acquired immune deficiency syndrome, or AIDS.
Source: Centers for Disease Control and Prevention
Cold, Flu, or Allergy?
Know the Difference for Best Treatment
You’re feeling pretty lousy. You’ve got sniffles, sneezing, and a sore throat. Is it a cold, flu, or allergies? It can be hard to tell them apart because they share so many symptoms. But understanding the differences will help you choose the best treatment.
“If you know what you have, you won’t take medications that you don’t need, that aren’t effective, or that might even make your symptoms worse,” says NIH’s Dr. Teresa Hauguel, an expert on infectious diseases that affect breathing.
Cold, flu, and allergy all affect your respiratory system, which can make it hard to breathe. Each condition has key symptoms that set them apart.
Colds and flu are caused by different viruses. “As a rule of thumb, the symptoms associated with the flu are more severe,” says Hauguel. Both illnesses can lead to a runny, stuffy nose; congestion; cough; and sore throat. But the flu can also cause high fever that lasts for 3-4 days, along with a headache, fatigue, and general aches and pain. These symptoms are less common when you have a cold.
“Allergies are a little different, because they aren’t caused by a virus,” Hauguel explains. “Instead, it’s your body’s immune system reacting to a trigger, or allergen, which is something you’re allergic to.” If you have allergies and breathe in things like pollen or pet dander, the immune cells in your nose and airways may overreact to these harmless substances. Your delicate respiratory tissues may then swell, and your nose may become stuffed up or runny.
“Allergies can also cause itchy, watery eyes, which you don’t normally have with a cold or flu,” Hauguel adds.
Allergy symptoms usually last as long as you’re exposed to the allergen, which may be about 6 weeks during pollen seasons in the spring, summer, or fall. Colds and flu rarely last beyond 2 weeks.
Most people with a cold or flu recover on their own without medical care. But check with a health care provider if symptoms last beyond 10 days or if symptoms aren’t relieved by over-the-counter medicines. For more about when to see a doctor, go to CDC's Flu Page ![]() .
.
To treat colds or flu, get plenty of rest and drink lots of fluids. If you have the flu, pain relievers such as aspirin, acetaminophen, or ibuprofen can reduce fever or aches. Allergies can be treated with antihistamines or decongestants. See the “Wise Choices” box for more details.
Be careful to avoid “drug overlap” when taking medicines that list 2 or more active ingredients on the label. For example, if you take 2 different drugs that contain acetaminophen—one for a stuffy nose and the other for headache—you may be getting too much acetaminophen.
“Read medicine labels carefully—the warnings, side effects, dosages. If you have questions, talk to your doctor or pharmacist, especially if you have children who are sick,” Hauguel says. “You don’t want to overmedicate, and you don’t want to risk taking a medication that may interact with another.”
Source: NIH, HHS
Flu
Also called: Grippe, Influenza
Flu is a respiratory infection caused by a number of viruses. The viruses pass through the air and enter your body through your nose or mouth. Between 5% and 20% of people in the U.S. get the flu each year. The flu can be serious or even deadly for elderly people, newborn babies, and people with certain chronic illnesses.
Symptoms of the flu come on suddenly and are worse than those of the common cold. They may include
Body or muscle aches
Chills
Cough
Fever
Headache
Sore throat
Is it a cold or the flu? Colds rarely cause a fever or headaches. Flu almost never causes an upset stomach. And "stomach flu" isn't really flu at all, but gastroenteritis.
Most people with the flu recover on their own without medical care. People with mild cases of the flu should stay home and avoid contact with others, except to get medical care. If you get the flu, your health care provider may prescribe medicine to help your body fight the infection and lessen symptoms.
The main way to keep from getting the flu is to get a yearly flu vaccine. Good hygiene, including hand washing, can also help.
Common Cold
Sneezing, sore throat, a stuffy nose, coughing - everyone knows the symptoms of the common cold. It is probably the most common illness. In the course of a year, people in the United States suffer 1 billion colds.
You can get a cold by touching your eyes or nose after you touch surfaces with cold germs on them. You can also inhale the germs. Symptoms usually begin 2 or 3 days after infection and last 2 to 14 days. Washing your hands and staying away from people with colds will help you avoid colds.
There is no cure for the common cold. For relief, try
Getting plenty of rest
Drinking fluids
Gargling with warm salt water
Using cough drops or throat sprays
Taking over-the-counter pain or cold medicines
However, do not give aspirin to children. And do not give cough medicine to children under four.
NIH: National Institute of Allergy and Infectious Diseases
Sore Throat
Also called: Pharyngitis
Your throat is a tube that carries food to your esophagus and air to your windpipe and larynx (also called the voice box). The technical name for the throat is pharynx.
You can have a sore throat for many reasons. Often, colds and flu cause sore throats. Other causes can include:
Allergies
Mononucleosis
Smoking
Strep throat
Tonsillitis - an infection in the tonsils
Treatment depends on the cause. Sucking on lozenges, drinking lots of liquids, and gargling may ease the pain. Over-the-counter pain relievers can also help, but children should not take aspirin.
Streptococcal Infections
Also called: Strep
Strep is short for Streptococcus, a type of bacteria. There are two types: group A and group B.
Group A strep causes
Strep throat - a sore, red throat, sometimes with white spots on the tonsils
Scarlet fever - an illness that follows strep throat. It causes a red rash on the body.
Impetigo - a skin infection
Toxic shock syndrome
Cellulitis and necrotizing fasciitis (flesh-eating disease)
Group B strep can cause blood infections, pneumonia and meningitis in newborns. A screening test during pregnancy can tell if you have it. If you do, I.V. antibiotics during labor can save your baby's life. Adults can also get group B strep infections, especially if they are elderly or already have health problems. Strep B can cause urinary tract infections, blood infections, skin infections and pneumonia in adults.
Antibiotics are used to treat strep infections.
Pneumococcal Infections
Also called: Streptococcus pneumoniae infections
Pneumococci are a type of streptococcus bacteria. The bacteria spread through contact with people who are ill or by healthy people who carry the bacteria in the back of their nose. Pneumococcal infections can be mild or severe. The most common types of infections are
Ear infections
Sinus infections
Pneumonia
Sepsis
Meningitis
How the diagnosis is made depends upon where the infection is. Your doctor will do a physical exam and health history. Possible tests may include blood, imaging, or lab tests. Treatment is with antibiotics. Vaccines can prevent pneumococcal infections. There are two vaccines. One is for infants and young children. The other is for people at high risk, including those who are over 65 years old, have chronic illnesses or weak immune systems, smoke, have asthma, or live in long-term care facilities.
Sinusitis
Sinusitis means your sinuses are inflamed. The cause can be an infection or another problem. Your sinuses are hollow air spaces within the bones surrounding the nose. They produce mucus, which drains into the nose. If your nose is swollen, this can block the sinuses and cause pain.
There are several types of sinusitis, including
Acute, which lasts up to 4 weeks
Subacute, which lasts 4 to 12 weeks
Chronic, which lasts more than 12 weeks and can continue for months or even years
Recurrent, with several attacks within a year
Acute sinusitis often starts as a cold, which then turns into a bacterial infection. Allergies, nasal problems, and certain diseases can also cause acute and chronic sinusitis.
Symptoms of sinusitis can include fever, weakness, fatigue, cough, and congestion. There may also be mucus drainage in the back of the throat, called postnasal drip. Your health care professional diagnoses sinusitis based on your symptoms and an examination of your nose and face. You may also need imaging tests. Treatments include antibiotics, decongestants, and pain relievers. Using heat pads on the inflamed area, saline nasal sprays, and vaporizers can also help.
Bird Flu
Also called: Avian flu, Avian influenza, H5N1, H7N9
Birds, just like people, get the flu. Bird flu viruses infect birds, including chickens, other poultry, and wild birds such as ducks. Most bird flu viruses can only infect other birds. However, bird flu can pose health risks to people. The first case of a bird flu virus infecting a person directly, H5N1, was in Hong Kong in 1997. Since then, the bird flu virus has spread to birds in countries in Asia, Africa, the Middle East, and Europe.
Human infection is still very rare, but the virus that causes the infection in birds might change, or mutate, to more easily infect humans. This could lead to a pandemic, a worldwide outbreak of the illness.
During an outbreak of bird flu, people who have contact with infected birds can become sick. It may also be possible to catch bird flu by eating poultry or eggs that are not well cooked or through contact with a person who has it. Bird flu can make people very sick or even cause death. Antiviral medicines may make the illness less severe, and may help prevent the flu in people who were exposed to it. There is currently no vaccine.
H1N1 Flu (Swine Flu)
Also called: Swine flu
Swine flu is an infection caused by a virus. It's named for a virus that pigs can get. People do not normally get swine flu, but human infections can and do happen. In 2009 a strain of swine flu called H1N1 infected many people around the world.
The virus is contagious and can spread from human to human. Symptoms of swine flu in people are similar to the symptoms of regular human flu and include fever, cough, sore throat, body aches, headache, chills and fatigue.
There are antiviral medicines you can take to prevent or treat swine flu. There is a vaccine available to protect against swine flu. You can help prevent the spread of germs that cause respiratory illnesses like influenza by
Covering your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.
Washing your hands often with soap and water, especially after you cough or sneeze. You can also use alcohol-based hand cleaners.
Avoiding touching your eyes, nose or mouth. Germs spread this way.
Trying to avoid close contact with sick people.
Staying home from work or school if you are sick.
Viral Infections
Viruses are capsules with genetic material inside. They are very tiny, much smaller than bacteria. Viruses cause familiar infectious diseases such as the common cold, flu and warts. They also cause severe illnesses such as HIV/AIDS, smallpox and hemorrhagic fevers.
Viruses are like hijackers. They invade living, normal cells and use those cells to multiply and produce other viruses like themselves. This eventually kills the cells, which can make you sick.
Viral infections are hard to treat because viruses live inside your body's cells. They are "protected" from medicines, which usually move through your bloodstream. Antibiotics do not work for viral infections. There are a few antiviral medicines available. Vaccines can help prevent you from getting many viral diseases.
Source: NIAID, CDC, NIH