FASDs are caused by a woman drinking alcohol during pregnancy. Alcohol in the mother’s blood passes to the baby through the umbilical cord. When a woman drinks alcohol, so does her baby.
Fetal alcohol spectrum disorders (FASDs) are a group of conditions that can occur in a person whose mother drank alcohol during pregnancy. These effects can include physical problems and problems with behavior and learning. Often, a person with an FASD has a mix of these problems.
FASDs are caused by a woman drinking alcohol during pregnancy. Alcohol in the mother’s blood passes to the baby through the umbilical cord. When a woman drinks alcohol, so does her baby.
There is no known safe amount of alcohol during pregnancy or when trying to get pregnant. There is also no safe time to drink during pregnancy. Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she’s pregnant. All types of alcohol are equally harmful, including all wines and beer.
To prevent FASDs, a woman should not drink alcohol while she is pregnant, or when she might get pregnant. This is because a woman could get pregnant and not know for up to 4 to 6 weeks. In the United States, nearly half of pregnancies are unplanned.

If a woman is drinking alcohol during pregnancy, it is never too late to stop drinking. Because brain growth takes place throughout pregnancy, the sooner a woman stops drinking the safer it will be for her and her baby. Resources are available here.
FASDs are completely preventable if a woman does not drink alcohol during pregnancy—so why take the risk?
FASDs refer to the whole range of effects that can happen to a person whose mother drank alcohol during pregnancy. These conditions can affect each person in different ways, and can range from mild to severe.
A person with an FASD might have:
Different terms are used to describe FASDs, depending on the type of symptoms.

Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE): ND-PAE was first included as a recognized condition in the Diagnostic and Statistical Manual 5 (DSM 5) of the American Psychiatric Association (APA) in 2013. A child or youth with ND-PAE will have problems in three areas: (1) thinking and memory, where the child may have trouble planning or may forget material he or she has already learned, (2) behavior problems, such as severe tantrums, mood issues (for example, irritability), and difficulty shifting attention from one task to another, and (3) trouble with day-to-day living, which can include problems with bathing, dressing for the weather, and playing with other children. In addition, to be diagnosed with ND-PAE, the mother of the child must have consumed more than minimal levels of alcohol before the child’s birth, which APA defines as more than 13 alcoholic drinks per month of pregnancy (that is, any 30-day period of pregnancy) or more than 2 alcoholic drinks in one sitting.

People with ND-PAE have problems with thinking, behavior, and life skills. ND-PAE occurs from being exposed to alcohol during pregnancy.
The term FASDs is not meant for use as a clinical diagnosis. CDC worked with a group of experts and organizations to review the research and develop guidelines for diagnosing FAS. The guidelines were developed for FAS only. CDC and its partners are working to put together diagnostic criteria for other FASDs, such as ARND. Clinical and scientific research on these conditions is going on now.
Diagnosing FAS can be hard because there is no medical test, like a blood test, for it. And other disorders, such as ADHD (attention-deficit/hyperactivity disorder) and Williams syndrome, have some symptoms like FAS.
To diagnose FAS, doctors look for:
Abnormal facial features (e.g., smooth ridge between nose and upper lip)
Lower-than-average height, weight, or both
Central nervous system problems (e.g., small head size, problems with attention and hyperactivity, poor coordination)
Prenatal alcohol exposure; although confirmation is not required to make a diagnosis
FASDs last a lifetime. There is no cure for FASDs, but research shows that early intervention treatment services can improve a child’s development.
There are many types of treatment options, including medication to help with some symptoms, behavior and education therapy, parent training, and other alternative approaches. No one treatment is right for every child. Good treatment plans will include close monitoring, follow-ups, and changes as needed along the way.
Also, “protective factors” can help reduce the effects of FASDs and help people with these conditions reach their full potential.1, 2
Protective factors include:
Diagnosis before 6 years of age
Loving, nurturing, and stable home environment during the school years
Absence of violence
Involvement in special education and social services

If you or the doctor thinks there could be a problem, ask the doctor for a referral to a specialist (someone who knows about FASDs), such as a developmental pediatrician, child psychologist, or clinical geneticist. In some cities, there are clinics whose staffs have special training in diagnosing and treating children with FASDs. To find doctors and clinics in your area visit the National and State Resource Directory from the National Organization on Fetal Alcohol Syndrome (NOFAS).
At the same time as you ask the doctor for a referral to a specialist, call your state or territory’s early intervention program to request a free evaluation to find out if your child can get services to help. This is sometimes called a Child Find evaluation. You do not need to wait for a doctor’s referral or a medical diagnosis to make this call.
Where to call for a free evaluation from the state depends on your child’s age:
If your child is younger than 3 years old, Call your state or territory’s early intervention program and say: “I have concerns about my child’s development and I would like to have my child evaluated to find out if he/she is eligible for early intervention services.”
Find your state’s early intervention contact information here.
Learn more about early intervention »
If your child is 3 years old or older, contact your local public school system.
Even if your child is not old enough for kindergarten or enrolled in a public school, call your local elementary school or board of education and ask to speak with someone who can help you have your child evaluated.
Learn more about this process »
For tips on sharing concerns about a child's development, click on one of the following:
Alcohol Use in Pregnancy
There is no known safe amount of alcohol use during pregnancy or while trying to get pregnant. There is also no safe time during pregnancy to drink. All types of alcohol are equally harmful, including all wines and beer. When a pregnant woman drinks alcohol, so does her baby.
Women also should not drink alcohol if they are sexually active and do not use effective contraception (birth control). This is because a woman might get pregnant and expose her baby to alcohol before she knows she is pregnant. Nearly half of all pregnancies in the United States are unplanned. Most women will not know they are pregnant for up to 4 to 6 weeks.
FASDs are completely preventable if a woman does not drink alcohol during pregnancy. Why take the risk?
Why Alcohol is Dangerous
Alcohol in the mother’s blood passes to the baby through the umbilical cord. Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral, and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders (FASDs). Children with FASDs might have the following characteristics and behaviors:
Abnormal facial features, such as a smooth ridge between the nose and upper lip (this ridge is called the philtrum)
Small head size
Shorter-than-average height
Low body weight
Poor coordination
Hyperactive behavior
Difficulty with attention
Poor memory
Difficulty in school (especially with math)
Learning disabilities
Speech and language delays
Intellectual disability or low IQ
Poor reasoning and judgment skills
Sleep and sucking problems as a baby
Vision or hearing problems
Problems with the heart, kidney, or bones

How Much Alcohol is Dangerous
There is no known safe amount of alcohol to drink while pregnant.
When Alcohol is Dangerous
There is no safe time to drink alcohol during pregnancy. Alcohol can cause problems for the developing baby throughout pregnancy, including before a woman knows she is pregnant. Drinking alcohol in the first three months of pregnancy can cause the baby to have abnormal facial features. Growth and central nervous system problems (e.g., low birthweight, behavioral problems) can occur from drinking alcohol anytime during pregnancy. The baby’s brain is developing throughout pregnancy and can be affected by exposure to alcohol at any time.
If a woman is drinking alcohol during pregnancy, it is never too late to stop. The sooner a woman stops drinking, the better it will be for both her baby and herself.
Advise about Risky Alcohol Use

Most adults who drink at risky levels and were asked about their alcohol use during a checkup did not receive advice to drink less from their providers, according to a new CDC study.
Most adults who drink at risky levels and were asked about their alcohol use during checkups were not advised to drink less, according to a new Centers for Disease Control and Prevention (CDC) study. The study looked at alcohol screening and brief counseling practices among healthcare providers in 17 states and the District of Columbia. Alcohol screening and brief counseling is an approach based on the best available scientific evidence that can help adults who drink alcohol at risky levels to reduce the amount that they drink.
In the United States, risky alcohol use resulted in more than $249 billion in economic costs in 2010 and over 88,000 deaths every year from 2006-2010. Risky alcohol use includes binge drinking, heavy drinking, and any use by pregnant women or those under age 21. Binge drinking is drinking five or more drinks on a single occasion for men or four or more drinks on a single occasion for women. Heavy drinking (also considered high weekly or daily consumption) is drinking 15 or more drinks per week for men or eight or more drinks per week for women.
Risky alcohol use increases the risk for developing long-standing diseases (such as heart disease and breast cancer), as well as injuries and violence (such as motor vehicle crashes, suicide, and homicide). Any alcohol use by pregnant women increases the risk for miscarriage, stillbirth, and a range of lifelong disorders in their babies known as fetal alcohol spectrum disorders (FASDs).
Alcohol Screening and Brief Counseling
Similar to screenings for blood pressure or tobacco use, alcohol screening and brief counseling is an effective clinical preventive service that is supported by decades of research. It is recommended by the US Preventive Services Task Force and medical organizations, such as the American Academy of Family Physicians, the American Medical Association, the American College of Obstetricians and Gynecologists, and the American Academy of Pediatrics. In 2014, CDC published a guide to help primary medical care practices incorporate alcohol screening and brief counseling into routine clinic visits.
Recent Findings
CDC researchers found the following among U.S. adults who reported having a checkup in the past two years:
Among all adults
About 3 in 4 reported being asked about their alcohol use (in person or on a form);
However, only 1 in 3 were asked in a way to help identify risky drinking patterns.
Among binge drinkers asked about their alcohol use
Only 1 in 3 reported being advised by a provider about the harms of their alcohol use; and
Only 1 in 6 reported being advised to reduce or quit drinking.
These findings indicate that routine alcohol screening and brief counseling, as recommended, is not yet a standard part of primary medical care. This is despite evidence that it works, is cost-effective (good value for the amount of money that it costs), and is recommended for all adults during routine clinic visits with their primary healthcare providers. Continued efforts are needed to increase adoption of alcohol screening and brief counseling by healthcare providers to reduce risky alcohol use among adults.
CDC Activities
The CDC has conducted FASD research, identification, and prevention efforts since 1991. Key activities include the following:
Monitoring alcohol consumption among women of reproductive age;
Supporting the implementation, adoption, and promotion of alcohol screening and brief counseling, including CHOICES;
Promoting effective treatments for children, adolescents, and young adults living with FASDs and their families;
Enhancing healthcare provider education on prevention, identification, and treatment of FASDs; and
Offering FASD-related educational information and materials for women of reproductive age, healthcare providers, and the general public.
About this Study
The study, Screening for Excessive Alcohol Use and Brief Counseling of Adults — 17 States and the District of Columbia, 2014, was published in the March 31, 2017 issue of CDC’s Morbidity and Mortality Weekly Report (MMWR).
The data for the study were collected from 17 states and the District of Columbia (DC) from the 2014 Behavioral Risk Factor Surveillance System (BRFSS).
BRFSS is a state-based telephone survey of U.S. adults aged 18 and over. Information is collected on a variety of health conditions, health practices, and risk behaviors including alcohol use.
Resources for Health Professionals
Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use: A Step-by-Step Guide for Primary Care Practices
This guide provides steps and resources to help primary medical care practices plan and implement alcohol screening and brief counseling.
Alcohol Screening, Brief Intervention, and Referral to Treatment: Demonstration Videos
Oregon Health and Science University’s family medicine program offers videos with demonstrations of conducting alcohol screening and brief counseling.
Monitoring Alcohol Use

CDC monitors alcohol use among women of childbearing age in the United States. These data are important to help reduce alcohol-exposed pregnancies by identifying groups of women at increased risk and designing prevention programs aimed at reducing risk behaviors and improving pregnancy outcomes.
The data are collected using the Behavioral Risk Factor Surveillance System (BRFSS). The BRFSS is an ongoing, state-based, random-digit-dialed telephone survey. To determine the potential number of women at risk for an alcohol-exposed pregnancy, data from the BRFSS are analyzed for women aged 18–44 years in all 50 states. Women are asked about their use of alcohol during the 30 days before the survey. It should be noted that the BRFSS excludes households without landline telephones, so the results might not be representative of certain segments of the U.S. population. Alcohol use may also be underreported.
The following patterns of alcohol drinking are examined:
Any alcohol use (one or more drinks)
Binge drinking (4 or more drinks on any one occasion).
Interventions

CDC promotes two strategies to reduce the number of alcohol-exposed pregnancies – alcohol screening and brief intervention (SBI) and CHOICES. Broadening CDC’s FASD prevention efforts to include both alcohol SBI and CHOICES provides the opportunity to offer both brief and extended intervention options to women of reproductive age as appropriate, and to address risky alcohol use within the broader context of women’s health.
Women report that the drinking behavior of their partner, family members, and friends are strong influences on their alcohol consumption.
Providing alcohol SBI to all individuals— men, women, and adolescents—might normalize discussion of alcohol use and begin to reduce the stigma associated with getting help.
Alcohol screening and brief intervention (SBI) is an effective but underused preventive health service recommended by the U.S. Preventive Services Task Force and covered under the Affordable Care Act. Similar to hypertension or cholesterol screening, alcohol SBI can occur as part of a patient’s wellness visit.
It involves:
A validated set of screening questions to identify a patient’s drinking patterns, which takes only a few minutes.
A short conversation with patients who are drinking too much, and referral to specialized treatment as appropriate.
CDC has developed an Alcohol SBI Implementation Guide to help staff in primary care practices plan and implement alcohol SBI to reduce alcohol use. The guide also presents information on risky alcohol use and how it can be addressed through alcohol SBI.
CHOICES is an evidence-based counseling intervention (i.e., based on activities that research has shown to be valid and effective) for non-pregnant women that helps them reduce or stop their drinking, use contraception effectively, or both. CHOICES uses motivational interviewing to increase a woman’s motivation and commitment to change.
Training & Education
Improvements in FASD prevention, identification and care can be enhanced through systematic efforts to educate healthcare professionals. Such efforts will contribute toward the goals of better alcohol screening and intervention for women at risk for an alcohol-exposed pregnancy and identification and treatment for individuals living with FASDs.
Parents, caregivers, school staff, and others who are with children with FASDs every day can benefit from learning more about FASDs, how they affect the child, strategies for working with the child to best enable him or her to meet his or her full potential, and how to locate appropriate services for the affected child and his or her family.
CDC is committed to improving practice, education, and awareness of those who care for women at risk for an alcohol-exposed pregnancy and those who work with individuals living with FASDs. CDC supports the following activities:
Collaborative for Alcohol-Free Pregnancy:
Partnering for Practice Change
CDC works with FASD Practice and Implementation Centers (PICs) and National Partners, to prevent FASDs by improving healthcare practice, education, and awareness among healthcare professionals. CDC recognizes the following strategies as essential among healthcare professionals working to preventing FASDs:
Use of evidence-based practices, such as alcohol screening and brief intervention (SBI), to prevent alcohol-exposed pregnancy and risky alcohol use
Care for women at risk of an alcohol-exposed
Work with people living with FASDs
In 2014, CDC funded FASD Practice and Implementation Centers (PICs) to expand previous efforts from FASD training programs and shift the perspective from individual training for medical and allied health care professionals to impacting healthcare practice at the systems level and focusing on prevention opportunities. Grantees include:
Baylor College of Medicine
University of Alaska Anchorage
University of California, San Diego
University of Missouri
University of Nevada, Reno
University of Wisconsin
In 2014, CDC funded national partners to strengthen strategic partnerships with key national medical societies, professional organizations, and constituent groups. The two main components include: (1) supporting strategies to improve the delivery of care related to FASDs through promotion of training opportunities; creating change around Maintenance of Certification and other continuing educational requirements for provider groups; developing, integrating, and disseminating FASD-related content and messaging; and fostering collaboration among medical organizations and CDC-funded Practice and Implementation Centers to create complementary products, messages, and approaches; (2) ensuring messages are scientifically accurate and consistent with the perspectives of families and individuals living with FASDs; and increasing the availability and reach of community-level FASD resources and materials. Grantees are:
American Academy of Pediatrics
American College of Obstetricians and Gynecologists
University of Pittsburgh, School of Nursing
University of Texas at Austin, School of Social Work
National Organization on Fetal Alcohol Syndrome
Collaboration with the Administration for Children and Families

CDC and the Administration for Children and Families (ACF) Children’s Bureau are working together to improve the identification and care of children who were exposed to alcohol and other drugs during pregnancy. The focus of this work is the Prenatal Alcohol and Other Drug Exposures in Child Welfare project.
There are approximately 3.4 million children in the U.S. child welfare system, with 415,000 of these children in foster care. ACF estimates that 6 out of 10 children in foster care come from homes where alcohol and/or other drugs are misused.
Exposure to alcohol and other drugs during pregnancy can cause significant problems for newborns, children, and adolescents. Alcohol can cause life-long birth defects and developmental disabilities such as fetal alcohol spectrum disorders (FASDs). Children with FASDs can have difficulty with learning, controlling impulses, and behaving in appropriate ways. ACF research found that developmental issues can make parenting difficult and frustrating, often leading to periods of abuse or neglect.
The goal of the Prenatal Alcohol and Other Drug Exposures in Child Welfare project is to improve the health and developmental outcomes of children in the welfare system who were exposed to alcohol and other drugs during pregnancy. Over the course of this multi-year project, activities will include the following:
Exploring current knowledge, attitudes, policies, practices, and needs of child welfare agencies for identifying and caring for children who were exposed to alcohol and other drugs during pregnancy, as well as caring for their families
Developing resources based on the best available evidence of success for training professional staff, families, and foster families to promote identification, referral, and care of children who were exposed to alcohol and other drugs during pregnancy
Promoting the best ways to identify, refer, and care for children who were exposed to alcohol and other drugs during pregnancy, as well as care for their families
Establishing methods for national, state, and local monitoring of children who were exposed to alcohol and other drugs during pregnancy
For more information on children who were exposed to alcohol during pregnancy, visit https://www.cdc.gov/ncbddd/fasd/facts.html.
Key Findings: Alcohol use and binge drinking among women of childbearing age – United States, 2011-2013
The Morbidity and Mortality Weekly Report (MMWR) has published a new study looking at alcohol use among pregnant and nonpregnant women of childbearing age in the United States.
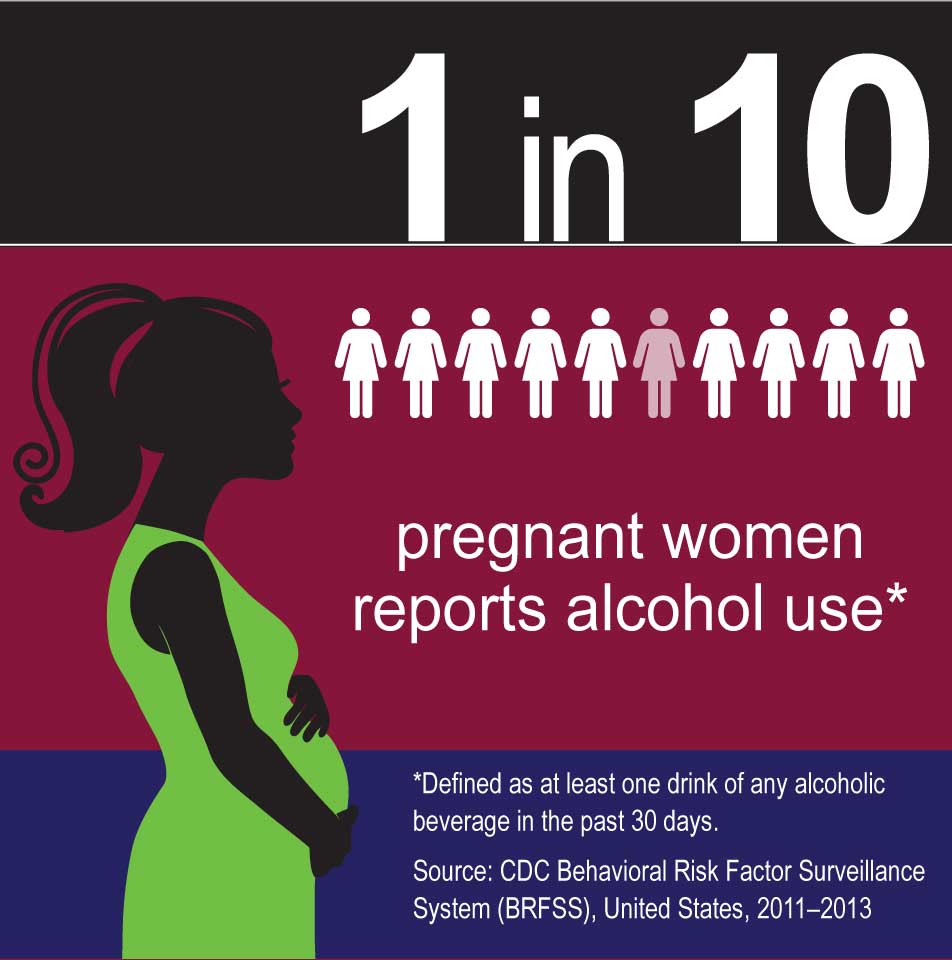
CDC researchers found that 1 in 10 pregnant women aged 18-44 years reported consuming alcohol* and about 1 in 33 reported binge drinking† in the past 30 days. This means that about one third of pregnant women who consume alcohol engage in binge drinking.
This is important information for healthcare professionals and women of childbearing age. Healthcare professionals who provide primary care to women of childbearing age should inform women that there is no known safe level of alcohol consumption when they are pregnant or might be pregnant. In addition, healthcare professionals can also implement alcohol screening and brief intervention in their primary care practices.
You can read the MMWR article here.
Main Findings
About half of nonpregnant women reported any alcohol use* and about 1 in 5 reported binge drinking† in the past 30 days.
Among pregnant women, 1 in 10 reported any alcohol use and 1 in 33 reported binge drinking in the past 30 days.
Among pregnant women, the highest prevalence of any alcohol use was among those who were
35-44 years
college graduates
not married
Among women who reported binge drinking in the past 30 days, pregnant women reported an average of 4.6 binge drinking episodes. This was higher than the average of 3.1 such episodes reported by nonpregnant women. The intensity (largest number of drinks consumed per episode) of binge drinking did not differ between pregnant and nonpregnant women.
Among nonpregnant women who reported binge drinking, those aged 18-20 years reported the highest frequency and intensity compared to other age groups.
* Any alcohol use was defined as having at least one drink of any alcoholic beverage in the past 30 days
† Binge drinking was defined as having consumed four or more drinks on an occasion at least one time in the past 30 days.
About this Study
The study uses data collected from the Behavioral Risk Factor Surveillance System (BRFSS), a state-based, landline and cellphone survey of the U.S. population.
To estimate alcohol use and binge drinking for women aged 18-44 years, data from the 2011-2013 BRFSS were analyzed for all 50 states and the District of Columbia.
Among binge drinkers, the frequency (number of binge drinking episodes in the past 30 days) and intensity (largest number of drinks consumed per episode) of binge drinking was also estimated.
CDC’s Activities: Preventing alcohol-exposed pregnancies and FASDs
CDC is working to prevent alcohol-exposed pregnancies with the following activities:
CDC tracks alcohol use among women of reproductive age in the United States.
CDC supports the implementation of evidence-based interventions to reduce risky alcohol use and alcohol-exposed pregnancies, including alcohol screening and brief intervention and CHOICES.
CDC collaborates with FASD Practice and Implementation Centers and National Partners to promote systems level practice changes among healthcare providers in the prevention, identification, and management of FASDs.
CDC promotes effective interventions to improve the lives of children, adolescents, and young adults living with FASDs and their families.
CDC offers FASD-related educational information and materials for women of reproductive age, healthcare providers, and the general public.
More Information
Key Findings Reference
Alcohol use and binge drinking among women of childbearing age – United States, 2011–2013 Morbidity and Mortality Weekly Report; September 25, 2015; 64(37); 1042-1046 CDC
Source: Centers for Disease Control and Prevention