Diabetes Insipidus
What is diabetes insipidus?
Diabetes insipidus is a rare disorder that occurs when a person's kidneys pass an abnormally large volume of urine that is insipid—dilute and odorless. In most people, the kidneys pass about 1 to 2 quarts of urine a day. In people with diabetes insipidus, the kidneys can pass 3 to 20 quarts of urine a day. As a result, a person with diabetes insipidus may feel the need to drink large amounts of liquids.
Diabetes insipidus and diabetes mellitus—which includes both type 1 and type 2 diabetes—are unrelated, although both conditions cause frequent urination and constant thirst. Diabetes mellitus causes high blood glucose, or blood sugar, resulting from the body's inability to use blood glucose for energy. People with diabetes insipidus have normal blood glucose levels; however, their kidneys cannot balance fluid in the body.
What are the kidneys and what do they do?
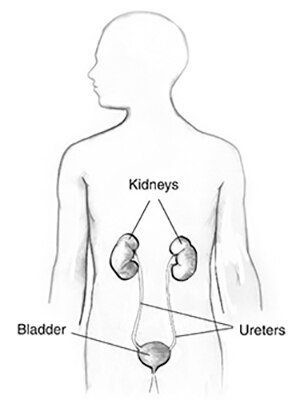
The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the kidneys normally filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. The urine flows from the kidneys to the bladder through tubes called ureters. The bladder stores urine. When the bladder empties, urine flows out of the body through a tube called the urethra, located at the bottom of the bladder.
Every day, the kidneys normally filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine.
How is fluid regulated in the body?
A person's body regulates fluid by balancing liquid intake and removing extra fluid. Thirst usually controls a person’s rate of liquid intake, while urination removes most fluid, although people also lose fluid through sweating, breathing, or diarrhea. The hormone vasopressin, also called antidiuretic hormone, controls the fluid removal rate through urination. The hypothalamus, a small gland located at the base of the brain, produces vasopressin. The nearby pituitary gland stores the vasopressin and releases it into the bloodstream when the body has a low fluid level. Vasopressin signals the kidneys to absorb less fluid from the bloodstream, resulting in less urine. When the body has extra fluid, the pituitary gland releases smaller amounts of vasopressin, and sometimes none, so the kidneys remove more fluid from the bloodstream and produce more urine.
What are the types of diabetes insipidus?
The types of diabetes insipidus include
central
nephrogenic
dipsogenic
gestational
Each type of diabetes insipidus has a different cause.
Central Diabetes Insipidus
Central diabetes insipidus happens when damage to a person's hypothalamus or pituitary gland causes disruptions in the normal production, storage, and release of vasopressin. The disruption of vasopressin causes the kidneys to remove too much fluid from the body, leading to an increase in urination. Damage to the hypothalamus or pituitary gland can result from the following:
surgery
infection
inflammation
a tumor
head injury
Central diabetes insipidus can also result from an inherited defect in the gene that produces vasopressin, although this cause is rare. In some cases, the cause is unknown.
Nephrogenic Diabetes Insipidus
Nephrogenic diabetes insipidus occurs when the kidneys do not respond normally to vasopressin and continue to remove too much fluid from a person's bloodstream. Nephrogenic diabetes insipidus can result from inherited gene changes, or mutations, that prevent the kidneys from responding to vasopressin. Other causes of nephrogenic diabetes insipidus include
chronic kidney disease
certain medications, particularly lithium
low potassium levels in the blood
high calcium levels in the blood
blockage of the urinary tract
The causes of nephrogenic diabetes insipidus can also be unknown.
Dipsogenic Diabetes Insipidus
A defect in the thirst mechanism, located in a person's hypothalamus, causes dipsogenic diabetes insipidus. This defect results in an abnormal increase in thirst and liquid intake that suppresses vasopressin secretion and increases urine output. The same events and conditions that damage the hypothalamus or pituitary—surgery, infection, inflammation, a tumor, head injury—can also damage the thirst mechanism. Certain medications or mental health problems may predispose a person to dipsogenic diabetes insipidus.
Gestational Diabetes Insipidus
Gestational diabetes insipidus occurs only during pregnancy. In some cases, an enzyme made by the placenta—a temporary organ joining mother and baby—breaks down the mother's vasopressin. In other cases, pregnant women produce more prostaglandin, a hormone-like chemical that reduces kidney sensitivity to vasopressin. Most pregnant women who develop gestational diabetes insipidus have a mild case that does not cause noticeable symptoms. Gestational diabetes insipidus usually goes away after the mother delivers the baby; however, it may return if the mother becomes pregnant again.
What are the complications of diabetes insipidus?
The main complication of diabetes insipidus is dehydration if fluid loss is greater than liquid intake. Signs of dehydration include
thirst
dry skin
fatigue
sluggishness
dizziness
confusion
nausea
Severe dehydration can lead to seizures, permanent brain damage, and even death.
How is diabetes insipidus diagnosed?
A health care provider can diagnose a person with diabetes insipidus based on the following:
medical and family history
physical exam
urinalysis
blood tests
fluid deprivation test
magnetic resonance imaging (MRI)
Medical and Family History
Taking a medical and family history can help a health care provider diagnose diabetes insipidus. A health care provider will ask the patient to review his or her symptoms and ask whether the patient's family has a history of diabetes insipidus or its symptoms.
Physical Exam
A physical exam can help diagnose diabetes insipidus. During a physical exam, a health care provider usually examines the patient's skin and appearance, checking for signs of dehydration.
Urinalysis
Urinalysis tests a urine sample. A patient collects the urine sample in a special container at home, in a health care provider's office, or at a commercial facility. A health care provider tests the sample in the same location or sends it to a lab for analysis. The test can show whether the urine is dilute or concentrated. The test can also show the presence of glucose, which can distinguish between diabetes insipidus and diabetes mellitus. The health care provider may also have the patient collect urine in a special container over a 24-hour period to measure the total amount of urine produced by the kidneys.
Blood Tests
A blood test involves drawing a patient's blood at a health care provider’s office or a commercial facility and sending the sample to a lab for analysis. The blood test measures sodium levels, which can help diagnose diabetes insipidus and in some cases determine the type.
Fluid Deprivation Test
A fluid deprivation test measures changes in a patient’s body weight and urine concentration after restricting liquid intake. A health care provider can perform two types of fluid deprivation tests:
A short form of the deprivation test. A health care provider instructs the patient to stop drinking all liquids for a specific period of time, usually during dinner. The next morning, the patient will collect a urine sample at home. The patient then returns the urine sample to his or her health care provider or takes it to a lab where a technician measures the concentration of the urine sample.
A formal fluid deprivation test. A health care provider performs this test in a hospital to continuously monitor the patient for signs of dehydration. Patients do not need anesthesia. A health care provider weighs the patient and analyzes a urine sample. The health care provider repeats the tests and measures the patient's blood pressure every 1 to 2 hours until one of the following happens:
The patient's blood pressure drops too low or the patient has a rapid heartbeat when standing.
The patient loses 5 percent or more of his or her initial body weight.
Urine concentration increases only slightly in two to three consecutive measurements.
At the end of the test, a health care provider will compare the patient's blood sodium, vasopressin levels, and urine concentration to determine whether the patient has diabetes insipidus. Sometimes, the health care provider may administer medications during the test to see if they increase a patient's urine concentration. In other cases, the health care provider may give the patient a concentrated sodium solution intravenously at the end of the test to increase the patient's blood sodium level and determine if he or she has diabetes insipidus.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is a test that takes pictures of the body's internal organs and soft tissues without using x-rays. A specially trained technician performs the procedure in an outpatient center or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images. A patient does not need anesthesia, although people with a fear of confined spaces may receive light sedation. An MRI may include an injection of a special dye, called contrast medium. With most MRI machines, the person lies on a table that slides into a tunnel-shaped device that may be open ended or closed at one end. Some MRI machines allow the patient to lie in a more open space. MRIs cannot diagnose diabetes insipidus. Instead, an MRI can show if the patient has problems with his or her hypothalamus or pituitary gland or help the health care provider determine if diabetes insipidus is the possible cause of the patient's symptoms.
How is diabetes insipidus treated?
The primary treatment for diabetes insipidus involves drinking enough liquid to prevent dehydration. A health care provider may refer a person with diabetes insipidus to a nephrologist—a doctor who specializes in treating kidney problems—or to an endocrinologist—a doctor who specializes in treating disorders of the hormone-producing glands. Treatment for frequent urination or constant thirst depends on the patient’s type of diabetes insipidus:
Central diabetes insipidus. A synthetic, or man-made, hormone called desmopressin treats central diabetes insipidus. The medication comes as an injection, a nasal spray, or a pill. The medication works by replacing the vasopressin that a patient’s body normally produces. This treatment helps a patient manage symptoms of central diabetes insipidus; however, it does not cure the disease.
Nephrogenic diabetes insipidus. In some cases, nephrogenic diabetes insipidus goes away after treatment of the cause. For example, switching medications or taking steps to balance the amount of calcium or potassium in the patient’s body may resolve the problem. Medications for nephrogenic diabetes insipidus include diuretics, either alone or combined with aspirin or ibuprofen. Health care providers commonly prescribe diuretics to help patients’ kidneys remove fluid from the body. Paradoxically, in people with nephrogenic diabetes insipidus, a class of diuretics called thiazides reduces urine production and helps patients’ kidneys concentrate urine. Aspirin or ibuprofen also helps reduce urine volume.
Dipsogenic diabetes insipidus. Researchers have not yet found an effective treatment for dipsogenic diabetes insipidus. People can try sucking on ice chips or sour candies to moisten their mouths and increase saliva flow, which may reduce the desire to drink. For a person who wakes multiple times at night to urinate because of dipsogenic diabetes insipidus, taking a small dose of desmopressin at bedtime may help. Initially, the health care provider will monitor the patient’s blood sodium levels to prevent hyponatremia, or low sodium levels in the blood.
Gestational diabetes insipidus. A health care provider can prescribe desmopressin for women with gestational diabetes insipidus. An expecting mother’s placenta does not destroy desmopressin as it does vasopressin. Most women will not need treatment after delivery.
Most people with diabetes insipidus can prevent serious problems and live a normal life if they follow the health care provider’s recommendations and keep their symptoms under control.
Eating, Diet, and Nutrition
Researchers have not found that eating, diet, and nutrition play a role in causing or preventing diabetes insipidus.
Points to Remember
Diabetes insipidus is a rare disorder that occurs when a person’s kidneys pass an abnormally large volume of urine that is insipid—dilute and odorless.
A person’s body regulates fluid by balancing liquid intake and removing extra fluid. Thirst usually controls a person’s rate of liquid intake, while urination removes most fluid, although people also lose fluid through sweating, breathing, or diarrhea. The hormone vasopressin, also called antidiuretic hormone, controls the fluid removal rate through urination.
The types of diabetes insipidus include central, nephrogenic, dipsogenic, and gestational. Each type of diabetes insipidus has a different cause.
The main complication of diabetes insipidus is dehydration if fluid loss is greater than liquid intake.
A health care provider can diagnose a person with diabetes insipidus based on a medical and family history, a physical exam, urinalysis, blood tests, a fluid deprivation test, and magnetic resonance imaging (MRI).
The primary treatment for diabetes insipidus involves drinking enough liquid to prevent dehydration.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov .
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. The NIDDK translates and disseminates research findings through its clearinghouses and education programs to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Bessie Young, M.D., M.P.H., University of Washington; Dr. Joseph Verbalis, M.D, Georgetown University
Source: NIDDK, NIH