Sexually transmitted infections (STIs) are also called sexually transmitted diseases, or STDs. STIs are usually spread by having vaginal, oral, or anal sex. More than 9 million women in the United States are diagnosed with an STI each year. Women often have more serious health problems from STIs than men, including infertility. (OWH, HHS)

Sexually Transmitted Infections/Diseases
CONDITION: Amebiasis
Amebiasis is an infection of the intestines caused by the parasite Entamoeba histolytica.

Causes
Entamoeba histolytica can live in the large intestine (colon) without causing damage to the intestine. In some cases, it invades the colon wall, causing colitis, acute dysentery, or long-term (chronic) diarrhea. The infection can also spread through the blood to the liver. In rare cases, it can spread to the lungs, brain, or other organs.
This condition occurs worldwide. It is most common in tropical areas that have crowded living conditions and poor sanitation. Africa, Mexico, parts of South America, and India have major health problems due to this disease.
Entamoeba histolytica is spread through food or water contaminated with stools. This contamination is common when human waste is used as fertilizer. It can also be spread from person to person, particularly by contact with the mouth or rectal area of an infected person.
Risk factors for severe amebiasis include:
- Alcoholism
- Cancer
- Malnutrition
- Older or younger age
- Pregnancy
- Recent travel to a tropical region
- Use of corticosteroid medication to suppress the immune system
In the United States, amebiasis is most common among those who live in institutions or people who have traveled to an area where amebiasis is common.
Symptoms
Most people with this infection do not have symptoms. If symptoms occur, they are seen 7 to 28 days after being exposed to the parasite.
Mild symptoms:
- Abdominal cramps
- Diarrhea: Passage of 3 to 8 semiformed stools per day, or passage of soft stools with mucus and occasional blood
- Fatigue
- Excessive gas
- Rectal pain while having a bowel movement (tenesmus)
- Unintentional weight loss
Severe symptoms may include:
- Abdominal tenderness
- Bloody stools, including passage of liquid stools with streaks of blood, passage of 10 to 20 stools per day
- Fever
- Vomiting
Exams and Tests
The health care provider will perform a physical exam. You will be asked about your medical history, especially if you have recently traveled overseas.
Examination of the abdomen may show liver enlargement or tenderness in the abdomen.
Tests that may be ordered include:
- Blood test for amebiasis
- Examination of the inside of the lower large bowel (sigmoidoscopy)
- Stool test
- Microscope examination of stool samples, usually with multiple samples over several days
Treatment
Treatment depends on how severe the infection is. Usually, antibiotics are prescribed.
If you are vomiting, you may need to receive medicines through a vein (intravenously) until you can take them by mouth. Medicines to stop diarrhea are usually not prescribed, because they can make the condition worse.
After antibiotic treatment, your stool will likely be rechecked to make sure the infection has been cleared.
Outlook (Prognosis)
Outcome is usually good with treatment. Usually, the illness lasts about 2 weeks, but it can come back if you do not get treated.
Possible Complications
- Liver abscess
- Medication side effects, including nausea
- Spread of the parasite through the blood to the liver, lungs, brain, or other organs
When to Contact a Medical Professional
Call your health care provider if you have diarrhea that does not go away or gets worse.
Prevention
When traveling in countries where sanitation is poor, drink purified or boiled water. Do not eat uncooked vegetables or unpeeled fruit.
Alternative Names
Amebic dysentery; Intestinal amebiasis.
Source: MedlinePlus, NLM,NIH
- What is bacterial vaginosis (BV)?
- What causes BV?
- What are the signs of BV?
- How can I find out if I have BV?
- How is BV treated?
- Is it safe to treat pregnant women who have BV?
- Can BV cause health problems?
- How can I lower my risk of BV?
- More information on bacterial vaginosis

Bacterial vaginosis
Bacterial vaginosis or BV for short is when the natural balance of the friendly bacteria in the vagina is altered and they overgrow. This typically leads to a foul smelling or fishy discharge. Women with BV have higher numbers of undesirable bacteria and correspondingly fewer of other normal protective bacteria. By WomensHealthcare

Bacterial vaginosis

The vagina normally has a balance of mostly "good" bacteria and fewer "harmful" bacteria. Bacterial vaginosis, known as BV, develops when the balance changes. With BV, there is an increase in harmful bacteria and a decrease in good bacteria. BV is the most common vaginal infection in women of childbearing age.
What causes BV?
Not much is known about how women get BV. Any woman can get BV. But there are certain things that can upset the normal balance of bacteria in the vagina, raising your risk of BV:
- Having a new sex partner or multiple sex partners
- Douching
- Using an intrauterine device (IUD) for birth control
- Not using a condom
BV is more common among women who are sexually active, but it is not clear how sex changes the balance of bacteria. You cannot get BV from:
- Toilet seats
- Bedding
- Swimming pools
- Touching objects around you
What are the signs of BV?
Women with BV may have an abnormal vaginal discharge with an unpleasant odor. Some women report a strong fish-like odor, especially after sex. The discharge can be white (milky) or gray. It may also be foamy or watery. Other symptoms may include burning when urinating, itching around the outside of the vagina, and irritation. These symptoms may also be caused by another type of infection, so it is important to see a doctor. Some women with BV have no symptoms at all.
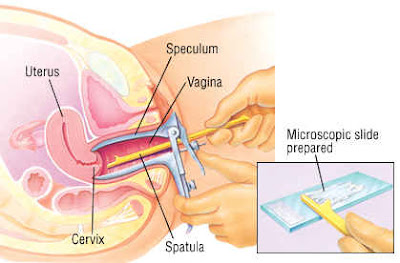
How can I find out if I have BV?
There is a test to find out if you have BV. Your doctor takes a sample of fluid from your vagina and has it tested. Your doctor may also see signs of BV during an examination of the vagina. To help your doctor find the signs of BV or other infections:
- Schedule the exam when you do not have your period.
- Don't douche for at least 24 hours before seeing your doctor. Experts suggest that women do not douche at all.
- Don't use vaginal deodorant sprays. They might cover odors that are important for diagnosis. It may also lead to irritation.
- Don't have sex or put objects, such as a tampon, in your vagina for at least 24 hours before going to the doctor.
How is BV treated?
BV is treated with antibiotic medicines prescribed by your doctor. Your doctor may give you either metronidazole (met-roh-NIH-duh-zohl) or clindamycin (klin-duh-MY-sin). Generally, male sex partners of women with BV don't need to be treated. However, BV can be spread to female partners. If your current partner is female, talk to her about treatment. You can get BV again even after being treated.


Is it safe to treat pregnant women who have BV?
All pregnant women with symptoms of BV should be tested and treated if they have it. This is especially important for pregnant women who have had a premature delivery or low birth weight baby in the past. There are treatments available at any stage of your pregnancy. Be sure to talk to your doctor about what is right for you.
Can BV cause health problems?
In most cases, BV doesn't cause any problems. But some problems can arise if BV is untreated.
- Pregnancy problems. BV can cause premature delivery and low birth weight babies (less than five pounds).
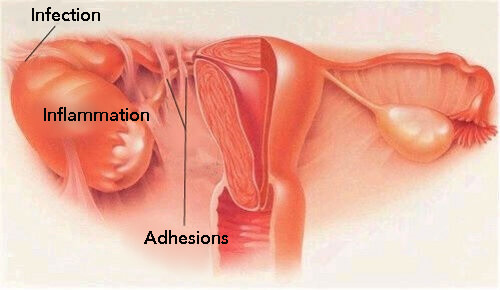
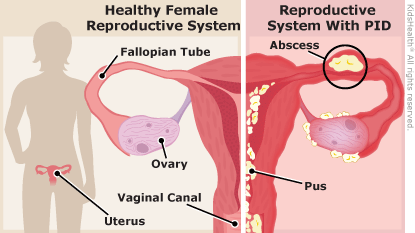
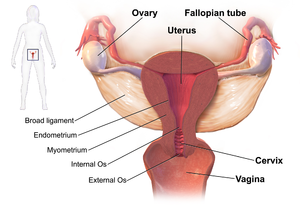
- PID. Pelvic inflammatory disease or PID is an infection that can affect a woman's uterus, ovaries, and fallopian tubes. Having BV increases the risk of getting PID after a surgical procedure, such as a hysterectomy or an abortion.
- Higher risk of getting HIV and other sexually transmitted infections (STIs). Having BV can raise your risk of HIV, chlamydia, and gonorrhea. Women with HIV who get BV are also more likely to pass HIV to a sexual partner.
How can I lower my risk of BV?
Experts are still figuring out the best way to prevent BV. But there are steps you can take to lower your risk.
- Help keep your vaginal bacteria balanced. Wash your vagina and anus every day with mild soap. When you go to the bathroom, wipe from your vagina to your anus. Keep the area cool by wearing cotton or cotton-lined underpants. Avoid tight pants and skip the pantyhose in summer.
- Don't douche. Douching removes some of the normal bacteria in the vagina that protects you from infection. This may raise your risk of BV. It may also make it easier to get BV again after treatment.
- Have regular pelvic exams. Talk with your doctor about how often you need exams, as well as STI tests.
- Finish your medicine. If you have BV, finish all the medicine your doctor gives you to treat it. Even if the symptoms go away, you still need to finish all of the medicine.
Practicing safe sex is also very important. Below are ways to help protect yourself.
- Don't have sex. The best way to prevent any STI is to not have vaginal, oral, or anal sex.
- Be faithful. Having sex with just one partner can also lower your risk. Be faithful to each other. That means that you only have sex with each other and no one else.
- Use condoms. Protect yourself with a condom EVERY time you have vaginal, anal, or oral sex. Condoms should be used for any type of sex with every partner. For vaginal sex, use a latex male condom or a female polyurethane condom. For anal sex, use a latex male condom. For oral sex, use a condom or a dental dam. A dental dam is a rubbery material that can be placed over the anus or the vagina before sexual contact.
- Talk with your sex partner(s) about STIs and using condoms. It's up to you to make sure you are protected. Remember, it's YOUR body! For more information, call the Centers for Disease Control and Prevention at 800-232-4636.
- Talk frankly with your doctor or nurse and your sex partner(s) about any STIs you or your partner(s) have or had. Talk about any discharge in the genital area. Try not to be embarrassed.
More information on bacterial vaginosis
For more information about bacterial vaginosis, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
American College of Obstetricians and Gynecologists
Phone: 202-638-5577
- American Social Health Association
Phone: 919-361-8400
- Association of Reproductive Health Professionals
Phone: 202-466-3825
- CDC National Prevention Information Network (NPIN), CDC, HHS
Phone: 800-458-5231
- National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), CDC, HHS
Phone: 800-232-4636
- Healthy Women
Phone: 877-986-9472
Source: Office on Women's Health, HHS
Any woman can get bacterial vaginosis. Having bacterial vaginosis can increase your chance of getting an STD.
The content here can be syndicated (added to your web site).
Print Version
Commercial Print Version
What is bacterial vaginosis?
Bacterial vaginosis (BV) is an infection caused when too much of certain bacteria change the normal balance of bacteria in the vagina.
How common is bacterial vaginosis?
Bacterial vaginosis is the most common vaginal infection in women ages 15-44.
How is bacterial vaginosis spread?
We do not know about the cause of BV or how some women get it. BV is linked to an imbalance of “good” and “harmful” bacteria that are normally found in a woman's vagina.
We do know that having a new sex partner or multiple sex partners and douching can upset the balance of bacteria in the vagina and put women at increased risk for getting BV.
However, we do not know how sex contributes to BV. BV is not considered an STD, but having BV can increase your chances of getting an STD. BV may also affect women who have never had sex.
You cannot get BV from toilet seats, bedding, or swimming pools.
How can I avoid getting bacterial vaginosis?
Doctors and scientists do not completely understand how BV is spread, and there are no known best ways to prevent it.
The following basic prevention steps may help lower your risk of developing BV:
- Not having sex;
- Limiting your number of sex partners; and
- Not douching.
STDs & Pregnancy
I’m pregnant. How does bacterial vaginosis affect my baby?
Pregnant women can get BV. Pregnant women with BV are more likely to have babies who are born premature (early) or with low birth weight than women who do not have BV while pregnant. Low birth weight means having a baby that weighs less than 5.5 pounds at birth.
Treatment is especially important for pregnant women.
How do I know if I have bacterial vaginosis?
Many women with BV do not have symptoms. If you do have symptoms, you may notice a thin white or gray vaginal discharge, odor, pain, itching, or burning in the vagina. Some women have a strong fish-like odor, especially after sex. You may also have burning when urinating; itching around the outside of the vagina, or both.
How will my doctor know if I have bacterial vaginosis?
A health care provider will look at your vagina for signs of BV and perform laboratory tests on a sample of vaginal fluid to determine if BV is present.
Can bacterial vaginosis be cured?
BV will sometimes go away without treatment. But if you have symptoms of BV you should be checked and treated. It is important that you take all of the medicine prescribed to you, even if your symptoms go away. A health care provider can treat BV with antibiotics, but BV can recur even after treatment. Treatment may also reduce the risk for STDs.
Male sex partners of women diagnosed with BV generally do not need to be treated. However, BV may be transferred between female sex partners.
What happens if I don't get treated?
BV can cause some serious health risks, including
- Increasing your chance of getting HIV if you have sex with someone who is infected with HIV;
- If you are HIV positive, increasing your chance of passing HIV to your sex partner;
- Making it more likely that you will deliver your baby too early if you have BV while pregnant;
- Increasing your chance of getting other STDs, such as chlamydia and gonorrhea. These bacteria can sometimes cause pelvic inflammatory disease (PID), which can make it difficult or impossible for you to have children.
Where can I get more information?
Division of STD Prevention (DSTDP)
Centers for Disease Control and Prevention
www.cdc.gov/std
Order Publication Online at www.cdc.gov/std/pub
CDC-INFO Contact Center
1-800-CDC-INFO (1-800-232-4636)
TTY: (888) 232-6348
Contact CDC-INFO
CDC National Prevention Information Network (NPIN)
P.O. Box 6003
Rockville, MD 20849-6003
E-mail: npin-info@cdc.gov
Sources
Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2010. MMWR 2010;59(No. RR-12)
Hillier S and Holmes K. Bacterial vaginosis. In: K. Holmes, P. Sparling, P. Mardh et al (eds). Sexually Transmitted Diseases, 3rd Edition. New York: McGraw-Hill, 1999, 563-586.
Related Content
- STDs & Pregnancy Fact Sheet
- Pregnancy and HIV, Viral Hepatitis, and STD Prevention
- Pelvic Inflammatory Disease (PID) Fact Sheet
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
CDC: Centers for Disease Control and Prevention
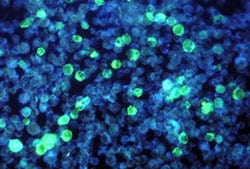
CONDITION: Candidiasis


Photomicrograph of the fungus Candida albicans
Candidiasis is a fungal infection caused by yeasts that belong to the genus Candida. There are over 20 species of Candida yeasts that can cause infection in humans, the most common of which is Candida albicans. Candida yeasts normally reside in the intestinal tract and can be found on mucous membranes and skin without causing infection; however, overgrowth of these organisms can cause symptoms to develop. Symptoms of candidiasis vary depending on the area of the body that is infected.
Candidiasis that develops in the mouth or throat is called “thrush” or oropharyngeal candidiasis. Candidiasis in the vagina is commonly referred to as a “yeast infection.” Invasive candidiasis occurs when Candida species enter the bloodstream and spread throughout the body. Click the links below for more information on the different types of Candida infections.
For other fungal topics, visit the fungal diseases homepage.



Types of Candidiasis
- Oropharyngeal / Esophageal Candidiasis
- Genital / vulvovaginal candidiasis
- Invasive Candidiasis
Global Emergence of Candida auris

Candida auris is an emerging fungus that presents a serious global health threat. Healthcare facilities in several countries have reported that C. auris has caused severe illness in hospitalized patients. C. auris is often resistant to multiple antifungal drugs.
Source: CDC
Oral Candidiasis/mouth thrush
Oral candidiasis (kan-dih-DEYE-uh-suhss), or thrush, is a type of fungal infection inside the mouth. Thrush causes swelling and a thick white coating on your mouth, tongue, throat, and esophagus. (The infection is only called oral candidiasis if it appears in your mouth.) Thrush happens when candida, a fungus that is normally found in the body, grows too much in these areas. It also can overgrow in your vagina. This is called a vaginal yeast infection. Thrush is common in people living with HIV and can be hard to get rid of. Thrush is partly diagnosed by how your mouth looks. A doctor might also take a scraping of the white patches in your mouth that will appear with an infection. Thrush is usually first treated with prescription lozenges and mouth rinses. If this doesn't work or the thrush keeps coming back, antifungal drugs are used. If thrush is not treated, symptoms will last. In very rare cases, untreated thrush may enter the bloodstream and spread throughout the body.

Source: OWH, HHS
CONDITION: Chancroid


Chancroid is a bacterial infection that is spread through sexual contact.
Chancroid (caused by Haemophilus ducreyi, a bacteria):
Sexually Transmitted Disease Facts
NOTE: Chancroid is rare in the U.S. If you have signs or symptoms of any sexually transmitted disease you should see a health care provider for evaluation and possible treatment.
On this page:
Signs and Symptoms
Transmission
Complications
Prevention
Testing and Treatment
For More Information
Signs and Symptoms


Chancroid Symptoms:
- Painful and draining open sores in the genital area
- Painful, swollen lymph nodes in the groin
- Begin 4-10 days after exposure

Transmission
- Vaginal sex
- Oral sex
- Anal sex
- Skin to skin contact with infected lesion or sore
Complications
If left untreated, chancroid:
- Can spread to sex partners
- Makes it easier to transmit or acquire HIV during sex
- Can cause destruction of foreskin tissue on penis
- Sores can become infected with other germs
Prevention
- Avoiding vaginal, oral or anal sex is the best way to prevent STDs.
- Latex condoms, when used consistently and correctly, can reduce the risk of chancroid only when the infected areas are covered or protected by the condom.
- Always use latex condoms during vaginal and anal sex.
- Use a latex condom for oral sex on a penis.
- Use a latex barrier (dental dam or condom cut in half) for oral sex on a vagina or anus.
- Limit the number of sex partners.
- Notify sex partners immediately if infected.
- Infected sex partners should be tested and treated.
Testing and Treatment
- Get a test from a medical provider if infection is suspected.
- Chancroid can be cured using medication prescribed by a medical provider.
- Partners should be treated at the same time.
NOTE: A person can be re-infected after treatment.
For more information, contact:
STD, HIV and TB Section
Minnesota Department of Health
651-201-5414
Minnesota Family Planning and STD Hotline
1-800-783-2287 Voice/TTY; 651-645-9360 (Metro)
American Social Health Association (ASHA)
CDC National STD and AIDS Hotlines
1-800-CDC-INFO; 1-888-232-6348 TTY
1-800-344-7432 (Spanish)
Content Notice: This site contains HIV or STD prevention messages that may not be appropriate for all audiences. Since HIV and other STDs are spread primarily through sexual practices or by sharing needles, prevention messages and programs may address these topics. If you are not seeking such information or may be offended by such materials, please exit this web site.
Additional Information on Chancroid

The prevalence of chancroid has declined in the United States. When infection does occur, it is usually associated with sporadic outbreaks. Worldwide, chancroid appears to have declined as well, although infection might still occur in some regions of Africa and the Caribbean. Like genital herpes and syphilis, chancroid is a risk factor in the transmission and acquisition of HIV infection.
Diagnostic Considerations
A definitive diagnosis of chancroid requires the identification of H. ducreyi on special culture media that is not widely available from commercial sources; even when these media are used, sensitivity is <80%. No FDA-cleared PCR test for H. ducreyi is available in the United States, but such testing can be performed by clinical laboratories that have developed their own PCR test and have conducted CLIA verification studies in genital specimens.
The combination of a painful genital ulcer and tender suppurative inguinal adenopathy suggests the diagnosis of chancroid. For both clinical and surveillance purposes, a probable diagnosis of chancroid can be made if all of the following criteria are met: 1) the patient has one or more painful genital ulcers; 2) the clinical presentation, appearance of genital ulcers and, if present, regional lymphadenopathy are typical for chancroid; 3) the patient has no evidence of T. pallidum infection by darkfield examination of ulcer exudate or by a serologic test for syphilis performed at least 7 days after onset of ulcers; and 4) an HSV PCR test or HSV culture performed on the ulcer exudate is negative.
Treatment
Successful treatment for chancroid cures the infection, resolves the clinical symptoms, and prevents transmission to others. In advanced cases, scarring can result despite successful therapy.
Recommended Regimens
- Azithromycin 1 g orally in a single dose
OR
- Ceftriaxone 250 mg IM in a single dose
OR
- Ciprofloxacin 500 mg orally twice a day for 3 days
OR
- Erythromycin base 500 mg orally three times a day for 7 days
Azithromycin and ceftriaxone offer the advantage of single-dose therapy. Worldwide, several isolates with intermediate resistance to either ciprofloxacin or erythromycin have been reported. However, because cultures are not routinely performed, data are limited regarding the current prevalence of antimicrobial resistance.
Other Management Considerations
Men who are uncircumcised and patients with HIV infection do not respond as well to treatment as persons who are circumcised or HIV-negative. Patients should be tested for HIV infection at the time chancroid is diagnosed. If the initial test results were negative, a serologic test for syphilis and HIV infection should be performed 3 months after the diagnosis of chancroid.
Follow-Up
Patients should be re-examined 3–7 days after initiation of therapy. If treatment is successful, ulcers usually improve symptomatically within 3 days and objectively within 7 days after therapy. If no clinical improvement is evident, the clinician must consider whether 1) the diagnosis is correct, 2) the patient is coinfected with another STD, 3) the patient is infected with HIV, 4) the treatment was not used as instructed, or 5) the H. ducreyi strain causing the infection is resistant to the prescribed antimicrobial. The time required for complete healing depends on the size of the ulcer; large ulcers might require >2 weeks. In addition, healing is slower for some uncircumcised men who have ulcers under the foreskin. Clinical resolution of fluctuant lymphadenopathy is slower than that of ulcers and might require needle aspiration or incision and drainage, despite otherwise successful therapy. Although needle aspiration of buboes is a simpler procedure, incision and drainage might be preferred because of reduced need for subsequent drainage procedures.
Management of Sex Partners
Regardless of whether symptoms of the disease are present, sex partners of patients who have chancroid should be examined and treated if they had sexual contact with the patient during the 10 days preceding the patient’s onset of symptoms.
Special Considerations
Pregnancy
Data suggest ciprofloxacin presents a low risk to the fetus during pregnancy, with a potential for toxicity during breastfeeding. Alternate drugs should be used during pregnancy and lactation. No adverse effects of chancroid on pregnancy outcome have been reported.
HIV Infection
Persons with HIV infection who have chancroid should be monitored closely because they are more likely to experience treatment failure and to have ulcers that heal slowly. Persons with HIV infection might require repeated or longer courses of therapy, and treatment failures can occur with any regimen. Data are limited concerning the therapeutic efficacy of the recommended single-dose azithromycin and ceftriaxone regimens in persons with HIV infection.
CDC:Centers for Disease Control & Prevention
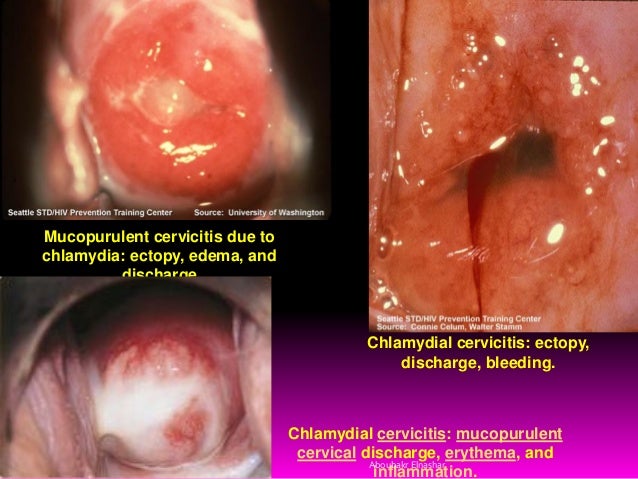
CONDITION: Chlamydia infection

- What is chlamydia and how common is it?
- How do you get chlamydia?
- What are the symptoms of chlamydia?
- How is chlamydia diagnosed?
- Who should get tested for chlamydia?
- What is the treatment for chlamydia?
- What should I do if I have chlamydia?
- What health problems can result from untreated chlamydia?
- How can chlamydia be prevented?
- More information on chlamydia
What is chlamydia and how common is it?

Chlamydia (kluh-MID-ee-uh) is a sexually transmitted infection (STI). STIs are also called STDs, or sexually transmitted diseases. Chlamydia is an STI caused by bacteria called chlamydia trachomatis. Chlamydia is the most commonly reported STI in the United States. Women, especially young women, are hit hardest by chlamydia.
Women often get chlamydia more than once, meaning they are "reinfected." This can happen if their sex partners were not treated. Reinfections place women at higher risk for serious reproductive health problems, such as infertility.
How do you get chlamydia?
You get chlamydia from vaginal, anal, or oral sex with an infected person. Chlamydia often has no symptoms. So people who are infected may pass chlamydia to their sex partners without knowing it. The more sex partners you (or your partner) have, the higher your risk of getting this STI.
An infected mother can pass chlamydia to her baby during childbirth. Babies born to infected mothers can get pneumonia (nuh-MOHN-yuh) or infections in their eyes.
What are the symptoms of chlamydia?

Chlamydia is known as a "silent" disease. This is because 75 percent of infected women and at least half of infected men have no symptoms.
If symptoms do occur, they most often appear within 1 to 3 weeks of exposure. The infection first attacks the cervix and urethra. Even if the infection spreads to the uterus and fallopian tubes, some women still have no symptoms. If you do have symptoms, you may have:
- Abnormal vaginal discharge
- Burning when passing urine
- Lower abdominal pain
- Low back pain
- Nausea
- Fever
- Pain during sex
- Bleeding between periods
Men with chlamydia may have:
- Discharge from the penis
- Burning when passing urine
- Burning and itching around the opening of the penis
- Pain and swelling in the testicles
The chlamydia bacteria also can infect your throat if you have oral sex with an infected partner.
Chlamydia is often not diagnosed or treated until problems show up. If you think you may have chlamydia, both you and your sex partner(s) should see a doctor right away — even if you have no symptoms.
Chlamydia can be confused with gonorrhea (gahn-uh-REE-uh), another STI. These STIs have some of the same symptoms and problems if not treated. But they have different treatments.


How is chlamydia diagnosed?
A doctor can diagnose chlamydia through:
- A swab test, where a fluid sample from an infected site (cervix or penis) is tested for the bacteria
- A urine test, where a urine sample is tested for the bacteria
A Pap test is not used to detect chlamydia.
Who should get tested for chlamydia?
You should be tested for chlamydia once a year if you are:
- 25 or younger and have sex
- Older than 25 and:Pregnant
- Have a new sex partner
- Have more than one sex partner
- Have sex with someone who has other sex partners
- Have had chlamydia or another STI in the past
- Have traded sex for money or drugs
- Do not use condoms during sex within a relationship that is not mutually monogamous, meaning you or your partner has sex with other people
You also should be tested if you have any symptoms of chlamydia.
What is the treatment for chlamydia?
Antibiotics are used to treat chlamydia. If treated, chlamydia can be cured.
All sex partners should be treated to keep from getting chlamydia again. Do not have sex until you and your sex partner(s) have ended treatment.
Tell your doctor if you are pregnant! Your doctor can give you an antibiotic that is commonly used during pregnancy.

What should I do if I have chlamydia?
Chlamydia is easy to treat. But you should be tested and treated right away to protect your reproductive health. If you have chlamydia:
- See a doctor right away. Women with chlamydia are 5 times more likely to get HIV, the virus that causes AIDS, from an infected partner.
- Follow your doctor's orders and finish all your antibiotics. Even if symptoms go away, you need to finish all the medicine.
- Don't engage in any sexual activity while being treated for chlamydia.
- Tell your sex partner(s) so they can be treated.
- See your doctor again if your symptoms don't go away within 1 to 2 weeks after finishing the medicine.
- See your doctor again within 3 to 4 months for another chlamydia test. This is most important if your sex partner was not treated or if you have a new sex partner.
Doctors, local health departments, and STI and family planning clinics have information about STIs. And they can all test you for chlamydia. Don't assume your doctor will test you for chlamydia when you have your Pap test. Take care of yourself by asking for a chlamydia test.
The Centers for Disease Control and Prevention (CDC) has free information and offers a list of clinics and doctors who provide treatment for STIs. Call CDC-INFO at 800-CDC-INFO (232-4636), TTY: 888-232-6348. You can call for information without leaving your name.
What health problems can result from untreated chlamydia?
Untreated chlamydia can damage a woman's reproductive organs and cause other health problems. Like the disease itself, the damage chlamydia causes is often "silent."
For women, untreated chlamydia may lead to:
- Pelvic inflammatory disease (PID). PID occurs when chlamydia bacteria infect the cells of the cervix, then spread to the uterus, fallopian tubes, and ovaries. PID occurs in up to 40 percent of women with untreated chlamydia. PID can lead to:Cystitis (siss-TEYE-tuhss), inflammation of the bladder.
- Infertility, meaning you can't get pregnant. The infection scars the fallopian tubes and keeps eggs from being fertilized.
- Ectopic or tubal pregnancy. This happens when a fertilized egg implants outside the uterus. It is a medical emergency.
- Chronic pelvic pain, which is ongoing pain, most often from scar tissue.
-
- HIV/AIDS. Women who have chlamydia are 5 times more likely to get HIV, the virus that causes AIDS, from a partner who is infected with it.
For men, untreated chlamydia may lead to:
- Infection and scarring of the urethra, the tube that carries urine from the body
- Prostatitis (prah-stuh-TEYE-tuhss), swelling of the prostate gland
- Infection in the tube that carries sperm from the testes, causing pain and fever
- Infertility

For women and men, untreated chlamydia may lead to:
- Chlamydia bacteria in the throat, if you have oral sex with an infected partner
- Proctitis (prok-TEYE-tuhss), which is an infection of the lining of the rectum, if you have anal sex with an infected partner
- Reiter's syndrome, which causes arthritis, eye redness, and urinary tract problems
For pregnant women, chlamydia infections may lead to premature delivery. And babies born to infected mothers can get:
- Infections in their eyes, called conjunctivitis (kuhn-junk-tih-VEYE-tuhss) or pinkeye. Symptoms include discharge from the eyes and swollen eyelids. The symptoms most often show up within the first 10 days of life. If left untreated, it can lead to blindness.
- Pneumonia. Symptoms include congestion and a cough that keeps getting worse. Both symptoms most often show up within 3 to 6 weeks of birth.
Both of these infant health problems can be treated with antibiotics.
How can chlamydia be prevented?
You can take steps to lower your risk of getting chlamydia and other STIs. The following steps work best when used together. No single strategy can protect you from every type of STI.
- Don't have sex. The surest way to avoid getting chlamydia or any STI is to practice abstinence. This means not having vaginal, anal, or oral sex.
- Be faithful. Having sex with only one unaffected partner who only has sex with you will keep you safe from chlamydia and other STIs. Both parthers must be faithful all the time to avoid STI exposure. This means you have sex only with each other and no one else. The fewer sex partners you have, the lower your risk of being exposed to chlamydia and other STIs.
- Use condoms correctly and every time you have sex. Use condoms for all types of sexual contact, even if penetration does not take place. Condoms work by keeping blood, a man's semen, and a woman's vaginal fluid — all of which can carry chlamydia — from passing from one person to another. Use protection from the very beginning to the very end of each sex act, and with every sex partner. And be prepared: Don't rely on your partner to have protection.
- Know that most methods of birth control — and other methods — will not protect you from chlamydia and other STIs. Birth control methods including the pill, shots, implants, intrauterine devices (IUDs), diaphragms, and spermicides will not protect you from STIs. If you use one of these birth control methods, make sure to also use a condom with every sex act. You might have heard of other ways to keep from getting STIs — such as washing genitals before sex, passing urine after sex, douching after sex, or washing the genital area with vinegar after sex. These methods do not prevent the spread of STIs.
- Talk with your sex partner(s) about STIs and using condoms before having sex. Make it clear that you will not have any type of sex at any time without a condom. It's up to you to make sure you are protected. Remember, it's your body! For more information, call the CDC at 800-232-4636.
- Get tested for STIs. If either you or your partner has had other sexual partners in the past, get tested for STIs before becoming sexually active. This includes women who have sex with women. Most women who have sex with women have had sex with men, too. So a woman can get an STI, including chlamydia, from a male partner, and then pass it to a female partner. Don't wait for your doctor to ask you about getting tested — ask your doctor! Many tests for STIs can be done at the same time as your regular pelvic exam.
- Learn the symptoms of chlamydia. But remember, chlamydia often has no symptoms. Seek medical help right away if you think you may have chlamydia or another STI.
- Have regular checkups and pelvic exams — even if you think you're healthy. During the checkup, your doctor will ask you a lot of questions about your lifestyle, including your sex life. This might seem too personal to share. But answering honestly is the only way your doctor is sure to give you the care you need.
More information on chlamydia
For more information about chlamydia, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
- CDC National Prevention Information Network (NPIN), CDC, HHS
Phone: 800-458-5231
- Department of Health and Human Services (HHS)
Phone: 800-232-4636
- National Institute of Allergy and Infectious Diseases, NIH, HHS
Phone: 866- 284-4107, or 301-496-5717 (TDD: 800-877-8339)
- Planned Parenthood Federation of America
Phone: 800-230-PLAN
- Sexually Transmitted Diseases (STDs), CDC, HHS
Phone: 800-CDC-INFO (800-232-4636)
Source: Office on Women's Health, HHS
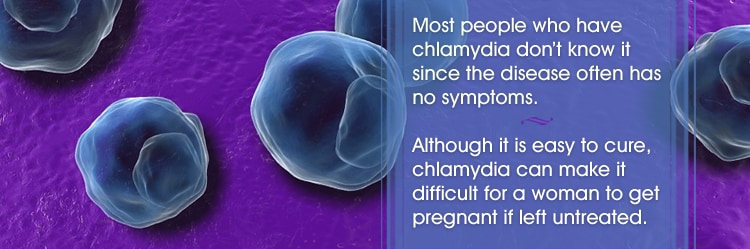
Chlamydia is a common sexually transmitted disease (STD) that can be easily cured. If left untreated, chlamydia can make it difficult for a woman to get pregnant.
What is chlamydia?
Chlamydia is a common STD that can infect both men and women. It can cause serious, permanent damage to a woman's reproductive system, making it difficult or impossible for her to get pregnant later on. Chlamydia can also cause a potentially fatal ectopic pregnancy (pregnancy that occurs outside the womb).
How is chlamydia spread?
You can get chlamydia by having vaginal, anal, or oral sex with someone who has chlamydia.
If your sex partner is male you can still get chlamydia even if he does not ejaculate (cum).
If you’ve had chlamydia and were treated in the past, you can still get infected again if you have unprotected sex with someone who has chlamydia.
If you are pregnant, you can give chlamydia to your baby during childbirth.
How can I reduce my risk of getting chlamydia?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting chlamydia:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
Am I at risk for chlamydia?
Anyone who has sex can get chlamydia through unprotected vaginal, anal, or oral sex. However, sexually active young people are at a higher risk of getting chlamydia. This is due to behaviors and biological factors common among young people. Gay, bisexual, and other men who have sex with men are also at risk since chlamydia can be spread through oral and anal sex.
Have an honest and open talk with your health care provider and ask whether you should be tested for chlamydia or other STDs. If you are a sexually active woman younger than 25 years, or an older woman with risk factors such as new or multiple sex partners, or a sex partner who has a sexually transmitted infection, you should get a test for chlamydia every year. Gay, bisexual, and men who have sex with men; as well as pregnant women should also be tested for chlamydia.
STDs & Pregnancy
I'm pregnant. How does chlamydia affect my baby?
If you are pregnant and have chlamydia, you can pass the infection to your baby during delivery. This could cause an eye infection or pneumonia in your newborn. Having chlamydia may also make it more likely to deliver your baby too early.
If you are pregnant, you should be tested for chlamydia at your first prenatal visit. Testing and treatment are the best ways to prevent health problems.
How do I know if I have chlamydia?
Most people who have chlamydia have no symptoms. If you do have symptoms, they may not appear until several weeks after you have sex with an infected partner. Even when chlamydia causes no symptoms, it can damage your reproductive system.
Women with symptoms may notice
- An abnormal vaginal discharge;
- A burning sensation when urinating.
Symptoms in men can include
- A discharge from their penis;
- A burning sensation when urinating;
- Pain and swelling in one or both testicles (although this is less common).
Men and women can also get infected with chlamydia in their rectum, either by having receptive anal sex, or by spread from another infected site (such as the vagina). While these infections often cause no symptoms, they can cause
- Rectal pain;
- Discharge;
- Bleeding.
You should be examined by your doctor if you notice any of these symptoms or if your partner has an STD or symptoms of an STD, such as an unusual sore, a smelly discharge, burning when urinating, or bleeding between periods.
How will my doctor know if I have chlamydia?
There are laboratory tests to diagnose chlamydia. Your health care provider may ask you to provide a urine sample or may use (or ask you to use) a cotton swab to get a sample from your vagina to test for chlamydia.
Can chlamydia be cured?
Yes, chlamydia can be cured with the right treatment. It is important that you take all of the medication your doctor prescribes to cure your infection. When taken properly it will stop the infection and could decrease your chances of having complications later on. Medication for chlamydia should not be shared with anyone.
Repeat infection with chlamydia is common. You should be tested again about three months after you are treated, even if your sex partner(s) was treated.
I was treated for chlamydia. When can I have sex again?
You should not have sex again until you and your sex partner(s) have completed treatment. If your doctor prescribes a single dose of medication, you should wait seven days after taking the medicine before having sex. If your doctor prescribes a medicine for you to take for seven days, you should wait until you have taken all of the doses before having sex.
STDs & Infertility
What happens if I don't get treated?
The initial damage that chlamydia causes often goes unnoticed. However, chlamydia can lead to serious health problems.
If you are a woman, untreated chlamydia can spread to your uterus and fallopian tubes (tubes that carry fertilized eggs from the ovaries to the uterus), causing pelvic inflammatory disease(PID). PID often has no symptoms, however some women may have abdominal and pelvic pain. Even if it doesn’t cause symptoms initially, PID can cause permanent damage to your reproductive system and lead to long-term pelvic pain, inability to get pregnant, and potentially deadly ectopic pregnancy (pregnancy outside the uterus).
Men rarely have health problems linked to chlamydia. Infection sometimes spreads to the tube that carries sperm from the testicles, causing pain and fever. Rarely, chlamydia can prevent a man from being able to have children.
Untreated chlamydia may also increase your chances of getting or giving HIV – the virus that causes AIDS.
Where can I get more information?
Division of STD Prevention (DSTDP)
Centers for Disease Control and Prevention
www.cdc.gov/std
CDC-INFO Contact Center
1-800-CDC-INFO (1-800-232-4636)
TTY: (888) 232-6348
Contact CDC-INFO
CDC National Prevention Information Network (NPIN)
P.O. Box 6003
Rockville, MD 20849-6003
E-mail: npin-info@cdc.gov
American Sexual Health Association (ASHA)
P.O. Box 13827
Research Triangle Park, NC 27709-3827
1-800-783-9877
Related Content
- STDs & Infertility
- STDs & Pregnancy – CDC fact sheet
- Pelvic Inflammatory Disease (PID) – CDC fact sheet
- Gonorrhea – CDC fact sheet
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
Source: Centers for Disease Control & Prevention, HHS
CONDITION: Congenital Syphilis

CDC Expert Commentary

Sarah Kidd, MD, MPH: “We are calling on clinicians to get back to the basics of syphilis prevention for pregnant women.”
Read More
What is congenital syphilis (CS)?
Congenital syphilis (CS) is a disease that occurs when a mother with syphilis passes the infection on to her baby during pregnancy. Learn more about syphilis.
How can CS affect my baby?
CS can have major health impacts on your baby. How CS affects your baby’s health depends on how long you had syphilis and if — or when — you got treatment for the infection.
CS can cause:
- Miscarriage (losing the baby during pregnancy),
- Stillbirth (a baby born dead),
- Prematurity (a baby born early),
- Low birth weight, or
- Death shortly after birth.


Darkfield micrograph of Treponema pallidum.
Up to 40% of babies born to women with untreated syphilis may be stillborn, or die from the infection as a newborn.
For babies born with CS, CS can cause:
- Deformed bones,
- Severe anemia (low blood count),
- Enlarged liver and spleen,
- Jaundice (yellowing of the skin or eyes),
- Brain and nerve problems, like blindness or deafness,
- Meningitis, and
- Skin rashes.
Do all babies born with CS have signs or symptoms?
No. It is possible that a baby with CS won’t have any symptoms at birth. But without treatment, the baby may develop serious problems. Usually, these health problems develop in the first few weeks after birth, but they can also happen years later.
Babies who do not get treatment for CS and develop symptoms later on can die from the infection. They may also be developmentally delayed or have seizures.
How common is CS?
After a steady decline from 2008–2012, data show a sharp increase in CS rates. In 2015, the number of CS cases was the highest it’s been since 2001.
Public health professionals across the country are very concerned about the growing number of congenital syphilis cases in the United States. It is important to make sure you get tested for syphilis during your pregnancy.
I'm pregnant. Do I need to get tested for syphilis?
Yes. All pregnant women should be tested for syphilis at the first prenatal visit (the first time you see your doctor for health care during pregnancy). If you don’t get tested at your first visit, make sure to ask your doctor about getting tested during a future checkup. Some women should be tested more than once during pregnancy. Talk with your doctor about the number of syphilis cases in your area and your risk for syphilis to determine if you should be tested again at the beginning of the third trimester, and again when your baby is born.
Keep in mind that you can have syphilis and not know it. Many people with syphilis do not have any symptoms. Also, syphilis symptoms may be very mild, or be similar to signs of other health problems. The only way to know for sure if you have syphilis is to get tested.
Is there treatment for syphilis?
Yes. Syphilis can be treated and cured with antibiotics. If you test positive for syphilis during pregnancy, be sure to get treatment right away.
If you are diagnosed with and treated for syphilis, your doctor should do follow-up testing for at least one year to make sure that your treatment is working.
How will my doctor know if my baby has CS?
Your doctor must consider several factors to determine if your baby has CS. These factors will include the results of your syphilis blood test and, if you were diagnosed with syphilis, whether you received treatment for syphilis during your pregnancy. Your doctor may also want to test your baby’s blood, perform a physical exam of your baby, or do other tests, such as a spinal tap or an x-ray, to determine if your baby has CS.
CDC has specific recommendations for your healthcare provider on how to evaluate babies born to women who have positive syphilis tests during pregnancy.
My baby was born with CS. Is there a way to treat the infection?
Yes. There is treatment for CS. Babies who have CS need to be treated right away -- or they can develop serious health problems. Depending on the results of your baby’s medical evaluation, he/she may need antibiotics in a hospital for 10 days. In some cases, only one injection of antibiotic is needed.
It’s also important that babies treated for CS get follow-up care to make sure that the treatment worked.
How can I reduce the risk of my baby getting CS or having health problems associated with CS?
Your baby will not get CS if you do not have syphilis. There are two important things you can do to protect your baby from getting CS and the health problems associated with the infection:
- Get a syphilis test at your first prenatal visit.
- Reduce your risk of getting syphilis before and during your pregnancy.
Talk with your doctor about your risk for syphilis. Have an open and honest conversation about your sexual history and STD testing. Your doctor can give you the best advice on any testing and treatment that you may need.
Get a syphilis test at your first prenatal visit
If you are pregnant, and have syphilis, you can still reduce the risk of CS in your baby. Getting tested and treated for syphilis can prevent serious health complications in both mother and baby.
Prenatal care is essential to the overall health and wellness of you and your unborn child. The sooner you begin receiving medical care during pregnancy, the better the health outcomes will be for you and your unborn baby.
At your first prenatal visit, ask your doctor about getting tested for syphilis. It is important that you have an open and honest conversation with your doctor at this time. Discuss any new or unusual physical symptoms you may be experiencing, as well as any drugs/medicines you are using, and whether you have new or multiple sex partners. This information will allow your doctor to make the appropriate testing recommendations. Even if you have been tested for syphilis in the past, you should be tested again when you become pregnant.
If you test positive for syphilis, you will need to be treated right away. Do not wait for your next prenatal visit. It is also important that your sex partner(s) receive treatment. Having syphilis once does not protect you from getting it again. Even after you’ve been successfully treated, you can still be reinfected. For this reason you must continue to take actions that will reduce your risk of getting a new infection.
Reduce your risk of getting syphilis before and during your pregnancy
Preventing syphilis in women and their sex partners is the best way to prevent CS.
If you are sexually active, the following things can lower your chances of getting syphilis:
- Being in a long-term mutually monogamous relationship with a partner who has been tested for syphilis and does not have syphilis.
- Using latex condoms the right way every time you have sex. Although condoms can prevent transmission of syphilis by preventing contact with a sore, you should know that sometimes syphilis sores occur in areas not covered by a condom, and contact with these sores can still transmit syphilis.
Also, talk with your doctor about your risk for syphilis. Have an open and honest conversation with your doctor about your sexual history and about STD testing. Your doctor can give you the best advice on any testing and treatment that you may need.
Remember that it’s possible to get syphilis and not know it, because sometimes the infection causes no symptoms, only very mild symptoms, or symptoms that mimic other illnesses.
Where can I get more information?
STD information and referrals to STD Clinics
CDC-INFO
1-800-CDC-INFO (800-232-4636)
TTY: 1-888-232-6348
In English, en Español
Resources:
CDC National Prevention Information Network (NPIN)
P.O. Box 6003
Rockville, MD 20849-6003
E-mail: npin-info@cdc.gov
American Sexual Health Association (ASHA)
P. O. Box 13827
Research Triangle Park, NC 27709-3827
1-800-783-9877
Where can I get more information?
Syphilis and MSM – Fact Sheet
Congenital Syphilis – Fact Sheet
STDs during Pregnancy – Fact Sheet
STDs During Pregnancy Fact Sheet
More on Congenital Syphilis

Fig. 1 The syphilis bacterium, treponema pallidum attaching to a testicular cell. Source: The Encyclopedia Britannica, online.
Congenital syphilis
Congenital syphilis is a severe, disabling, and often life-threatening infection seen in infants. A pregnant mother who has syphilis can spread the disease through the placenta to the unborn infant.
Congenital syphilis is caused by the bacteria Treponema pallidum, which is passed from mother to child during fetal development or at birth. Nearly half of all children infected with syphilis while they are in the womb die shortly before or after birth.
Despite the fact that this disease can be cured with antibiotics if caught early, rising rates of syphilis among pregnant women in the United States have increased the number of infants born with congenital syphilis.
Symptoms in newborns may include:
- Failure to gain weight or failure to thrive
- Fever
- Irritability
- No bridge to nose (saddle nose)
- Rash of the mouth, genitals, and anus
- Rash: starting as small blisters on the palms and soles, and later changing to copper-colored, flat or bumpy rash on the face, palms, and soles
- Watery fluid from the nose
Symptoms in older infants and young children may include:
- Abnormal notched and peg-shaped teeth, called Hutchinson teeth
- Bone pain
- Blindness
- Clouding of the cornea
- Decreased hearing or deafness
- Gray, mucus-like patches on the anus and outer vagina
- Joint swelling
- Refusal to move a painful arm or leg
- Saber shins (bone problem of the lower leg)
- Scarring of the skin around the mouth, genitals, and anus
If the disorder is suspected at the time of birth, the placenta will be examined for signs of syphilis. A physical examination of the infant may show signs of liver and spleen swelling and bone inflammation.
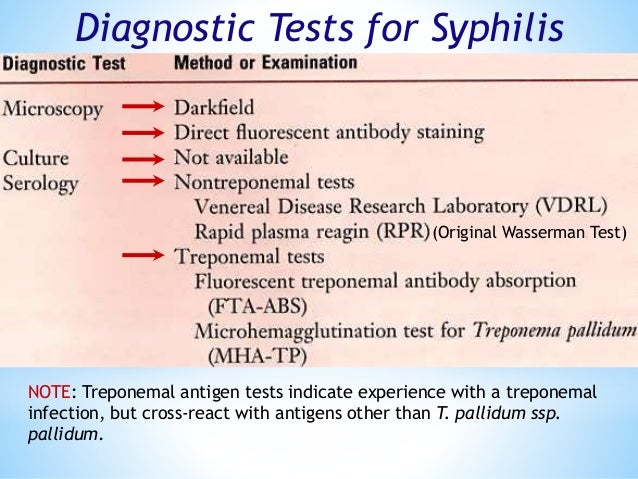
A routine blood test for syphilis is done during pregnancy. The mother may receive the following blood tests:
- Fluorescent treponemal antibody absorbed test (FTA-ABS)
- Rapid plasma reagin (RPR)
- Venereal disease research laboratory test (VDRL)
An infant or child may have the following tests:
- Bone x-ray
- Dark-field examination to detect syphilis bacteria under a microscope
- Eye examination
- Lumbar puncture
Many infants who were infected early in the pregnancy are stillborn. Treatment of the expectant mother lowers the risk of congenital syphilis in the infant. Babies who become infected when passing through the birth canal have a better outlook.
Health problems that can result if the baby isn't treated include:
- Blindness
- Deafness
- Deformity of the face
- Nervous system problems
Call your health care provider if your baby has signs or symptoms of this condition.
If you think that you may have syphilis and are pregnant (or plan to get pregnant), call your provider right away.
Safer sexual practices help prevent the spread of syphilis. If you suspect you have a sexually transmitted disease such as syphilis, seek medical attention right away to avoid complications like infecting your baby during pregnancy or birth.
Prenatal care is very important. A routine blood test for syphilis is done during pregnancy. This identifies infected mothers so they can treated to reduce the risks to the infant and themselves. Infants born to infected mothers who received proper penicillin treatment during pregnancy are at minimal risk for congenital syphilis.
Congenital lues; Fetal syphilis
Source: Medlineplus, NLM, NIH
CDC: Symptoms of Syphilis (Click images to view full size)

Darkfield micrograph of Treponema pallidum.

Primary stage syphilis sore (chancre) on the surface of a tongue.

Lesions of secondary syphilis.
Secondary stage syphilis sores (lesions) on the palms of the hands. Referred to as "palmar lesions."
Secondary stage syphilis sores (lesions) on the bottoms of the feet. Referred to as "plantar lesions."

Secondary syphilis rash on the back.WARNING: the images below depicts the symptoms of STDs and are intended for educational use only. Parental caution is advised.


Primary stage syphilis sore (chancre) inside the vaginal opening.
Source: CDC
CONDITION: Cryptosporidium
Cryptosporidium is a microscopic parasite that causes the diarrheal disease cryptosporidiosis. Both the parasite and the disease are commonly known as "Crypto."
There are many species of Cryptosporidium that infect animals, some of which also infect humans. The parasite is protected by an outer shell that allows it to survive outside the body for long periods of time and makes it very tolerant to chlorine disinfection.
While this parasite can be spread in several different ways, water (drinking water and recreational water) is the most common way to spread the parasite. Cryptosporidium is a leading cause of waterborne disease among humans in the United States.
CDC
Infectious Diseases Related to Travel
Cryptosporidiosis
Michele C. Hlavsa, Lihua Xiao
INFECTIOUS AGENT
Among the many protozoan parasites in the genus Cryptosporidium, Cryptosporidium hominis and C. parvum most frequently cause human infections.
TRANSMISSION
Cryptosporidium is transmitted via the fecal-oral route. Its low infectious dose, prolonged survival in moist environments, protracted communicability, and extreme chlorine tolerance make Cryptosporidium ideally suited for transmission through contaminated drinking or recreational water, such as swimming pools. Transmission can also occur through contaminated food, or contact with infected people, or contaminated surfaces.
EPIDEMIOLOGY
Cryptosporidiosis is endemic worldwide. Of 22 US Peace Corps volunteers, 9 developed anti-Cryptosporidium IgG while serving in Africa. International travel is a risk factor for sporadic cryptosporidiosis in the United States and other industrialized nations; however, few studies have assessed the prevalence of cryptosporidiosis in travelers. One study found 2.9% prevalence of Cryptosporidium infection among those with travel-associated diarrhea; cryptosporidiosis was significantly associated with travel to Asia, particularly India, and Latin America. Another study found a 6.4% prevalence of Cryptosporidium infection among North Americans with diarrhea associated with travel to 2 Mexican cities. This study suggests an association between cryptosporidiosis and length of travel.
CLINICAL PRESENTATIONS
Symptoms begin within 2 weeks (typically 5–7 days) after infection and are generally self-limited. The most common symptom is watery diarrhea. Other symptoms can include urgency, tenesmus, abdominal cramps, flatulence, nausea, vomiting, weight loss, fever, decreased appetite, fatigue, joint pain, and headache. In immunocompetent people, symptoms typically resolve within 2–3 weeks; patients might experience a recurrence of symptoms after a brief period of recovery before complete symptom resolution. Clinical presentation of cryptosporidiosis in HIV-infected patients varies with level of immunosuppression, ranging from no symptoms or transient disease to relapsing or chronic diarrhea or even choleralike diarrhea, which can lead to life-threatening wasting and malabsorption. Extraintestinal cryptosporidiosis (in the biliary or respiratory tract or rarely the pancreas) has been documented in children and immunocompromised people.
DIAGNOSIS
Tests for Cryptosporidium are typically not included in routine ova and parasite testing. Therefore, clinicians should specifically request testing for this parasite, when suspected. Because Cryptosporidium can be excreted intermittently, multiple stool collections (3 stool specimens collected on separate days) increase test sensitivity. Diagnostic techniques include direct fluorescent antibody (considered the gold standard), EIA testing, rapid immunochromatographic cartridge assays, and microscopy with modified acid-fast staining. False-positive results might occur when using rapid immunochromatographic cartridge assays if they are not used according to the manufacturer’s directions. Confirmation by microscopy might be considered.
TREATMENT
Most immunocompetent people will recover without treatment. Nitazoxanide is approved to treat cryptosporidiosis in immunocompetent people aged ≥1 year. Nitazoxanide has not been shown to be an effective treatment of cryptosporidiosis in HIV-infected patients. However, dramatic clinical and parasitologic responses have been reported in these patients after the immune system has been reconstituted with active combination antiretroviral therapy. Protease inhibitors might have direct anti-Cryptosporidium activity.
PREVENTION
Food and water precautions (see Chapter 2, Food & Water Precautions) and handwashing (www.cdc.gov/handwashing). Cryptosporidium is extremely tolerant to halogens (such as chlorine or iodine). Water can be treated effectively by heating it to a rolling boil for 1 minute or filtering with an absolute 1-µm filter. Alcohol-based hand sanitizers are not effective against the parasite. Prevention recommendations can be found at www.cdc.gov/parasites/crypto/prevention-control.html.
CDC website: www.cdc.gov/parasites/crypto
Source: CDC
CONDITION: Cytomegalovirus

Cytomegalovirus (pronounced sy-toe-MEG-a-low-vy-rus), or CMV, is a common virus that infects people of all ages. Over half of adults by age 40 have been infected with CMV. Once CMV is in a person’s body, it stays there for life and can reactivate. Most people infected with CMV show no signs or symptoms. However, CMV infection can cause serious health problems for people with weakened immune systems, as well as babies infected with the virus before they are born (congenital CMV).
About CMV
Cytomegalovirus (pronounced sy-toe-MEG-a-low-vy-rus), or CMV, is a common virus that infects people of all ages. In the United States, nearly one in three children are already infected with CMV by age 5 years. Over half of adults by age 40 have been infected with CMV. Once CMV is in a person's body, it stays there for life and can reactivate. A person can also be reinfected with a different strain (variety) of the virus.
Most people infected with CMV show no signs or symptoms. That’s because a healthy person's immune system usually keeps the virus from causing illness. However, CMV infection can cause serious health problems for people with weakened immune systems, as well as babies infected with the virus before they are born (congenital CMV).
Signs & Symptoms
Most people with CMV infection have no symptoms and aren’t aware that they have been infected. In some cases, infection in healthy people can cause mild illness that may include
- Fever,
- Sore throat,
- Fatigue, and
- Swollen glands.
Occasionally, CMV can cause mononucleosis or hepatitis (liver problem).
People with weakened immune systems who get CMV can have more serious symptoms affecting the eyes, lungs, liver, esophagus, stomach, and intestines. Babies born with CMV can have brain, liver, spleen, lung, and growth problems. Hearing loss is the most common health problem in babies born with congenital CMV infection, which may be detected soon after birth or may develop later in childhood.
Transmission and Prevention
People with CMV may shed (pass) the virus in body fluids, such as urine, saliva, blood, tears, semen, and breast milk. CMV is spread from an infected person in the following ways:
- From direct contact with urine or saliva, especially from babies and young children
- Through sexual contact
- From breast milk
- Through transplanted organs and blood transfusions
- From mother to child during pregnancy (congenital CMV)
Regular hand washing, particularly after changing diapers, is a commonly recommended step to decrease the spread of infections, and may reduce exposures to CMV.
Healthcare providers should follow standard precautions. For more recommendations in healthcare settings, see the Guide to Infection Prevention for Outpatient Settings.
Diagnosis
Blood tests can be used to diagnose CMV infections in people who have symptoms.
Treatment
Healthy people who are infected with CMV usually do not require medical treatment.
Medications are available to treat CMV infection in people who have weakened immune systems and babies who show symptoms of congenital CMV infection.
Babies Born with CMV (Congenital CMV Infection)
When a baby is born with cytomegalovirus (CMV) infection, it is called congenital CMV infection. About one out of every 150 babies are born with congenital CMV infection. However, only about one in five babies with congenital CMV infection will be sick from the virus or will have long-term health problems.
Transmission

Women can pass CMV to their baby during pregnancy. The virus in the woman’s blood can cross through the placenta and infect the baby. This can happen when a pregnant woman experiences a first-time infection, a reinfection with a different CMV strain (variety), or a reactivation of a previous infection during pregnancy.
Signs & Symptoms
Most babies with congenital CMV infection never show signs or have health problems. However, some babies may have health problems that are apparent at birth or may develop later during infancy or childhood. Although not fully understood, it is possible for CMV to cause the death of a baby during pregnancy (pregnancy loss).
Some babies may have signs of congenital CMV infection at birth. These signs include
- Premature birth,
- Liver, lung and spleen problems,
- Small size at birth,
- Small head size, and
- Seizures.
Some babies with signs of congenital CMV infection at birth may have long-term health problems, such as
- Hearing loss,
- Vision loss,
- Intellectual disability[2 pages],
- Small head size,
- Lack of coordination,
- Weakness or problems using muscles, and
- Seizures.
Some babies without signs of congenital CMV infection at birth may have hearing loss. Hearing loss may be present at birth or may develop later in babies who passed their newborn hearing test.
Diagnosis
Congenital CMV infection can be diagnosed by testing a newborn baby’s saliva, urine, or blood. Such specimens must be collected for testing within two to three weeks after the baby is born in order to confirm a diagnosis of congenital CMV infection.
Treatment and Management
Medicines, called antivirals, may decrease the risk of health problems and hearing loss in some infected babies who show signs of congenital CMV infection at birth.
Use of antivirals for treating babies with congenital CMV infection who have no signs at birth is not currently recommended.
Babies with congenital CMV infection, with or without signs at birth, should have regular hearing checks.
Regularly follow-up with your baby’s doctor to discuss the care and additional services your child may need.
Health Professionals & Clinical Overview
For most healthy people who acquire cytomegalovirus (CMV) after birth, there are few symptoms and no long-term health consequences. Some people who acquire CMV infection may experience a mononucleosis-like syndrome with prolonged fever and hepatitis. Once a person becomes infected, the virus establishes lifelong latency and may reactivate intermittently. Disease from reactivation of CMV infection rarely occurs unless the person's immune system is suppressed due to therapeutic drugs or disease.
For most people, CMV infection is not a serious health problem. However, certain groups are at high risk for serious complications from CMV infection:
- Infants infected in utero (congenital CMV infection)
- Very low birth weight and premature infants
- People with compromised immune systems, such as from organ and bone marrow transplants, and people infected with human immunodeficiency virus (HIV)
Characteristics of the Virus
CMV is a herpesvirus. This group of viruses include herpes simplex virus types 1 and 2, varicella-zoster virus, and Epstein-Barr virus. These viruses share a characteristic ability to establish lifelong latency. After initial infection, which may cause few symptoms, CMV becomes latent, residing in cells without causing detectable damage or clinical illness.
People who are infected with CMV sometimes shed the virus in body fluids, such as urine, saliva, blood, tears, semen, and breast milk. The shedding of virus may occur intermittently, without any detectable signs, and without causing symptoms. However, in people who are severely immunocompromised by medication or disease, viral reactivation may lead to symptomatic disease.
Transmission
CMV is transmitted by direct contact with infectious body fluids, such as urine or saliva. CMV can be transmitted sexually and through transplanted organs and blood transfusions.
CMV can be transmitted to infants through contact with maternal genital secretions during delivery or through breast milk. Healthy infants and children who acquire CMV after birth generally have few, if any, symptoms or complications from the infection. Women who are infected with CMV can still breastfeed infants born full-term.
Although the virus is not highly contagious, it has been shown to spread among household members and young children in daycare centers.
Risk of CMV Infection
CMV infects people of all ages. In the United States; nearly one in three children are already infected with CMV by age 5 years. By 40 years, over half of adults have been infected with CMV.
Childcare workers
People who care for or work closely with young children may be at greater risk of CMV infection than other people because CMV infection is common among young children. By age 5 years, one in three children have been infected with CMV, usually from breastfeeding or contact with other young children. Although young children with CMV infection generally have no symptoms, CMV can be present in their body fluids for months after they first become infected. Regular hand washing, especially after contact with body fluids of young children, is commonly recommended to avoid spread of infections, including CMV.
Pregnant women
In the United States, nearly half of women have already been infected with CMV before their first pregnancy. Of women who have never had a CMV infection, it is estimated that 1-4% of them will have a primary infection during pregnancy.
A woman who has a primary CMV infection during pregnancy is more likely to pass CMV to her fetus than a women who is reinfected or has a reactivation of the latent virus during pregnancy. However, in the United States, 50-75% of congenital CMV infections occur among infants born to mothers already infected with CMV, who either had a reinfection or a reactivation during pregnancy.
Routine screening for primary CMV infection during pregnancy is not recommended in the United States. Most laboratory tests currently available cannot conclusively detect if a primary CMV infection occurred during pregnancy. This makes it difficult to counsel pregnant women about the risk to their fetuses. The lack of a proven treatment to prevent or treat infection of the fetus reduces the potential benefits of prenatal screening.
Very low birth weight and premature infants
There are no recommendations against breastfeeding by mothers who are CMV-seropositive. However, premature infants (born
Diagnosing CMV
Primary CMV infections usually go unrecognized because most people are asymptomatic or do not have specific symptoms. Primary CMV infection should be suspected if a woman
- Has symptoms of infectious mononucleosis but has negative test results for Epstein-Barr virus, or
- Shows signs of hepatitis, but has negative test results for hepatitis A, B, and C.
CMV may be detected by viral culture or polymerase chain reaction (PCR) of infected blood, urine, saliva, cervical secretions, or breast milk.
CMV infection is usually diagnosed using serologic testing. Serum samples collected one to three months apart can be used to diagnose primary infection. Seroconversion (1st sample IgG negative, 2nd sample IgG positive) is clear evidence for recent primary infection. However, diagnosis of CMV infection between birth and one year can be complicated by the presence of maternal CMV IgG. For more information, see Interpretation of Laboratory Tests.
Treatment and Management
- No treatment is currently indicated for CMV infection in healthy people.
- Antiviral treatment is used for people with compromised immune systems who have either sight-related or life-threatening illnesses due to CMV infection.
- For congenital CMV treatment options, see Congenital CMV Infection.
Prevention
Regular handwashing, especially after contact with body fluids of young children, is commonly recommended to avoid spread of infections, including CMV.
Healthcare providers should follow standard precautions.
Vaccines are still in the research and development stage.
Congenital CMV Infection
About one out of every 150 infants are born with congenital cytomegalovirus (CMV) infection. However, only about one in five infants with congenital CMV infection will have long-term health problems.
Transmission
A pregnant woman can pass CMV to her fetus following primary infection, reinfection with a different CMV strain, or reactivation of a previous infection during pregnancy. The risk of transmission is greatest in the third trimester whereas risk of complications to the infant is greatest if infection occurs during the first trimester. Risk of transmission for primary infection is 30-40% in the first and second trimesters, and 40–70% in the third trimester.
Signs & Symptoms
Most infants with congenital CMV infection never have health problems. About 10% of infants with congenital CMV infection will have health problems that are apparent at birth, which include
- Premature birth,
- Liver, lung and spleen problems,
- Low birth weight,
- Microcephaly, and
- Seizures.
About 40-60% of infants born with signs of congenital CMV infection at birth will have long-term health problems, such as
- Hearing loss.
- Vision loss.
- Intellectual disability,
- Microcephaly,
- Lack of coordination,
- Weakness or problems using muscles, and
- Seizures.
Some infants without signs of congenital CMV infection at birth may later have hearing loss, but do not appear to have other long-term health problems. Hearing loss may be present at birth or may develop later in infants who passed their newborn hearing test. About 10-20% of infants with congenital CMV infection who have no signs at birth will have, or later develop, hearing loss.
Diagnosing Congenital CMV Infection
Congenital CMV infection is diagnosed by detection of CMV in the urine, saliva, blood, or other tissues within two to three weeks after birth. Only tests that detect CMV live virus (through viral culture) or CMV DNA (through polymerase chain reaction (PCR)) can be used to diagnose congenital CMV infection. Congenital CMV infection cannot be diagnosed using samples collected more than two to three weeks after birth because testing after this time cannot distinguish between congenital infection and an infection acquired during and after delivery.
Serological tests are not recommended for diagnosing congenital CMV infection. Maternal IgG antibodies pass through the placenta during pregnancy; thus, CMV IgG testing of infants may reflect maternal antibody status, and does not necessarily indicate infection in the infant. Maternal IgM antibodies do not cross the placenta and, thus, CMV IgM in the newborn would indicate congenital infection, but is only present in 25-40% of newborns with congenital infection.
For diagnosis of acquired CMV infection see Interpretation of Laboratory Tests.
Treatment and Management
- Antiviral medications, such as ganciclovir or valganciclovir, may improve hearing and developmental outcomes in infants with symptoms of congenital CMV disease. Ganciclovir can have serious side effects, and has only been studied in infants with symptomatic congenital CMV disease. There is limited data on the effectiveness of ganciclovir or valganciclovir to treat infants with isolated hearing loss.
- Any infant diagnosed with congenital CMV infection should have his or her hearing and vision tested regularly. Most infants with congenital CMV grow up healthy. However, if the child has delayed onset of hearing or vision problems, early detection may improve outcomes. To learn more, see this CDC website about hearing loss in children.
Source: CDC
CONDITION: Donovanosis (Granuloma Inguinale)
![Granuloma inguinale (klik op foto voor vergroting) [bron: Wikipedia] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-1z.jpg) |
![Granuloma inguinale (klik op foto voor vergroting) [bron: www.tuasaude.com] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-2z.jpg) |
![Granuloma inguinale (klik op foto voor vergroting) [bron: www.genitaldischarge.com] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-3z.jpg) |
| granuloma inguinale |
granuloma inguinale |
granuloma inguinale |
Granuloma inguinale is a genital ulcerative disease caused by the intracellular gram-negative bacterium Klebsiella granulomatis (formerly known as Calymmatobacterium granulomatis). The disease occurs rarely in the United States, although it is endemic in some tropical and developing areas, including India; Papua, New Guinea; the Caribbean; central Australia; and southern Africa. Clinically, the disease is commonly characterized as painless, slowly progressive ulcerative lesions on the genitals or perineum without regional lymphadenopathy; subcutaneous granulomas (pseudobuboes) also might occur. The lesions are highly vascular (i.e., beefy red appearance) and bleed. Extragenital infection can occur with extension of infection to the pelvis, or it can disseminate to intra-abdominal organs, bones, or the mouth. The lesions also can develop secondary bacterial infection and can coexist with other sexually transmitted pathogens.
Diagnostic Considerations

![Granuloma inguinale (klik op foto voor vergroting) [bron: www.studyblue.com] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-4z.jpg) |
| Donovan bodies |
The causative organism of granuloma inguinale is difficult to culture, and diagnosis requires visualization of dark-staining Donovan bodies on tissue crush preparation or biopsy. No FDA-cleared molecular tests for the detection of K. granulomatis DNA exist, but such an assay might be useful when undertaken by laboratories that have conducted a CLIA verification study.
Treatment
Several antimicrobial regimens have been effective, but only a limited number of controlled trials have been published. Treatment has been shown to halt progression of lesions, and healing typically proceeds inward from the ulcer margins; prolonged therapy is usually required to permit granulation and re-epithelialization of the ulcers. Relapse can occur 6–18 months after apparently effective therapy.
Recommended Regimen
- Azithromycin 1 g orally once per week or 500 mg daily for at least 3 weeks and until all lesions have completely healed
Alternative Regimens
- Doxycycline 100 mg orally twice a day for at least 3 weeks and until all lesions have completely healed
OR
- Ciprofloxacin 750 mg orally twice a day for at least 3 weeks and until all lesions have completely healed
OR
- Erythromycin base 500 mg orally four times a day for at least 3 weeks and until all lesions have completely healed
OR
- Trimethoprim-sulfamethoxazole one double-strength (160 mg/800 mg) tablet orally twice a day for at least 3 weeks and until all lesions have completely healed
The addition of another antibiotic to these regimens can be considered if improvement is not evident within the first few days of therapy. Addition of an aminoglycoside to these regimens is an option (gentamicin 1 mg/kg IV every 8 hours).
Other Management Considerations
Persons should be followed clinically until signs and symptoms have resolved. All persons who receive a diagnosis of granuloma inguinale should be tested for HIV.
Follow-up
Patients should be followed clinically until signs and symptoms resolve.
Management of Sex Partners
Persons who have had sexual contact with a patient who has granuloma inguinale within the 60 days before onset of the patient’s symptoms should be examined and offered therapy. However, the value of empiric therapy in the absence of clinical signs and symptoms has not been established.
Special Considerations
Pregnancy
Doxycycline should be avoided in the second and third trimester of pregnancy because of the risk for discoloration of teeth and bones, but is compatible with breastfeeding. Data suggest that ciprofloxacin presents a low risk to the fetus during pregnancy. Sulfonamides are associated with rare but serious kernicterus in those with G6PD deficiency and should be avoided in third trimester and during breastfeeding. For these reasons, pregnant and lactating women should be treated with a macrolide regimen (erythromycin or azithromycin). The addition of an aminoglycoside (gentamicin 1 mg/kg IV every 8 hours) can be considered if improvement is not evident within the first few days of therapy.
HIV Infection
Persons with both granuloma inguinale and HIV infection should receive the same regimens as those who do not have HIV infection. The addition of an aminoglycoside (gentamicin 1 mg/kg IV every 8 hours) can be considered if improvement is not evident within the first few days of therapy.
Source: CDC
CONDITION: Epstein-Barr virus (EBV)

Epstein-Barr virus, or EBV, is one of the most common human viruses in the world. It spreads primarily through saliva. EBV can cause infectious mononucleosis, also called mono, and other illnesses. Most people will get infected with EBV in their lifetime and will not have any symptoms. Mono caused by EBV is most common among teens and adults…
Infectious mononucleosis, also called “mono,” is a contagious disease. Epstein-Barr virus (EBV) is the most common cause of infectious mononucleosis, but other viruses can also cause this disease. It is common among teenagers and young adults, especially college students. At least 25% of teenagers and young adults who get infected with EBV will develop infectious mononucleosis.
Symptoms

Typical symptoms of infectious mononucleosis usually appear 4 to 6 weeks after you get infected with EBV. Symptoms may develop slowly and may not all occur at the same time.
These symptoms include—
- extreme fatigue
- fever
- sore throat
- head and body aches
- swollen lymph nodes in the neck and armpits
- swollen liver or spleen or both
- rash
Enlarged spleen and a swollen liver are less common symptoms. For some people, their liver or spleen or both may remain enlarged even after their fatigue ends.
Most people get better in 2 to 4 weeks; however, some people may feel fatigued for several more weeks. Occasionally, the symptoms of infectious mononucleosis can last for 6 months or longer.
Transmission


EBV is the most common cause of infectious mononucleosis, but other viruses can cause this disease. Typically, these viruses spread most commonly through bodily fluids, especially saliva. However, these viruses can also spread through blood and semen during sexual contact, blood transfusions, and organ transplantations.
Other infections that can cause infectious mononucleosis:
- Cytomegalovirus (CMV)
- Toxoplasmosis
- HIV
- Rubella
- Hepatitis A, B, or C
- Streptococcal pharyngitis
Prevention & Treatment
There is no vaccine to protect against infectious mononucleosis. You can help protect yourself by not kissing or sharing drinks, food, or personal items, like toothbrushes, with people who have infectious mononucleosis.
You can help relieve symptoms of infectious mononucleosis by—
- drinking fluids to stay hydrated
- getting plenty of rest
- taking over-the-counter medications for pain and fever
If you have infectious mononucleosis, you should not take ampicillin or amoxicillin. Based on the severity of the symptoms, a healthcare provider may recommend treatment of specific organ systems affected by infectious mononucleosis.
Because your spleen may become enlarged as a result of infectious mononucleosis, you should avoid contact sports until you fully recover. Participating in contact sports can be strenuous and may cause the spleen to rupture.
Diagnosing Infectious Mononucleosis
Healthcare providers typically diagnose infectious mononucleosis based on symptoms.
Laboratory tests are not usually needed to diagnose infectious mononucleosis. However, specific antibody tests may be needed to identify the cause of illness in people who do not have a typical case of infectious mononucleosis.
The blood work of patients who have infectious mononucleosis due to EBV infection may show—
- more white blood cells (lymphocytes) than normal
- unusual looking white blood cells (atypical lymphocytes)
- fewer than normal neutrophils or platelets
- abnormal liver function
CDC: Centers for Disease Control and Prevention
More on Epstein-Barr Virus (EBV)

Content:
- Symptoms
- Transmission
- Diagnosis
- Prevention & Treatment
Epstein-Barr virus (EBV), also known as human herpesvirus 4, is a member of the herpes virus family. It is one of the most common human viruses. EBV is found all over the world. Most people get infected with EBV at some point in their lives. EBV spreads most commonly through bodily fluids, primarily saliva. EBV can cause infectious mononucleosis(http://www.cdc.gov/epstein-barr/about-mono.html), also called mono, and other illnesses.
Symptoms
Symptoms of EBV infection can include
- fatigue
- fever
- inflamed throat
- swollen lymph nodes in the neck
- enlarged spleen
- swollen liver
- rash
Many people become infected with EBV in childhood. EBV infections in children usually do not cause symptoms, or the symptoms are not distinguishable from other mild, brief childhood illnesses. People who get symptoms from EBV infection, usually teenagers or adults, get better in 2 to 4 weeks. However, some people may feel fatigued for several weeks or even months.
After you get an EBV infection, the virus becomes latent (inactive) in your body. In some cases, the virus may reactivate. This does not always cause symptoms, but people with compromised immune systems are more likely to develop symptoms if EBV reactivates.
EBV Spreads Easily
EBV is spread by saliva through
- kissing
- sharing drinks and food
- using the same cups, eating utensils, or toothbrushes
- having contact with toys that children have drooled on
Transmission
EBV spreads most commonly through bodily fluids, especially saliva. However, EBV can also spread through blood and semen during sexual contact, blood transfusions, and organ transplantations.
EBV can be spread by using objects, such as a toothbrush or drinking glass, that an infected person recently used. The virus probably survives on an object at least as long as the object remains moist. There is no evidence that disinfecting the objects will prevent EBV from spreading.
The first time you get infected with EBV (primary EBV infection) you can spread the virus for weeks and even before you have symptoms. Once the virus is in your body, it stays there in a latent (inactive) state. If the virus reactivates, you can potentially spread EBV to others no matter how much time has passed since the initial infection.
Diagnosis
Diagnosing EBV infection can be challenging since symptoms(http://www.cdc.gov/epstein-barr/about-ebv.html#symptoms) are similar to other illnesses. EBV infection can be confirmed with a blood test that detects antibodies. About 90% of adults have antibodies that show that they have a current or past EBV infection.
For more information, see Laboratory Testing(http://www.cdc.gov/epstein-barr/laboratory-testing.html).
Prevention & Treatment
There is no vaccine to protect against EBV infection. You can help protect yourself by not kissing or sharing drinks, food, or personal items, like toothbrushes, with people who have EBV infection.
There is no specific treatment for EBV. However, some things can be done to help relieve symptoms, including
- drinking fluids to stay hydrated
- getting plenty of rest
- taking over-the-counter medications for pain and fever
For Healthcare Providers
Epstein-Barr virus (EBV) can cause illnesses and complications aside from infectious mononucleosis(http://www.cdc.gov/epstein-barr/about-mono.html). People with compromised immune systems may develop more symptoms from EBV infection. They may also have more severe illness caused by EBV infection.
Nervous System
EBV infection can affect a person’s brain, spinal cord, and nerves.
It can cause conditions such as—
- Viral meningitis (swelling of the tissues that cover the brain and spinal cord)
- Encephalitis (swelling of the brain)
- Optic neuritis (swelling of the eye nerve)
- Transverse myelitis (swelling of the spinal cord)
- Facial nerve palsies (paralysis of facial muscles)
- Guillain-Barré syndrome (an immune system disease)
- Acute cerebellar ataxia (sudden uncoordinated muscle movement)
- Hemiplegia (paralysis on one side of the body)
- Sleep disorders
- Psychoses
Hematological System
EBV infection can affect a person’s blood and bone marrow. The virus can cause the body to produce an excessive number of white blood cells called lymphocytes (lymphocytosis).
It can also weaken the immune system, making it more difficult for the body to fight infection.
Examples of some of these conditions include—
- Neutropenia with secondary infections
- Hemophagocytic syndrome (hemophagocytic lymphohistiocytosis)
- Acquired hypogammaglobulinemia
- X-linked lymphoproliferative disease
Other Conditions
EBV infection can also cause—
- Pneumonia (injury of the lungs)
- Interstitial lung disease (a large group of disorders, most of which cause scarring of lung tissue)
- Pancreatitis (swelling of the pancreas)
- Myocarditis (swelling of the heart muscle)
- Oral cavity-oral hairy leukoplakia (raised, white patches on the tongue), which is usually seen in people infected with HIV
Cancers associated with EBV infection include—
- Burkitt’s lymphoma (cancer of the lymphatic system)
- Nasopharyngeal carcinoma (cancer of the upper throat)
- Hodgkin’s disease and non-Hodgkin’s lymphoma (cancers of the lymphatic system)
- Post-transplant lymphoproliferative disorder (white blood cells are produced in excess)
- Other tumors including leiomyosarcomas (cancer in the soft tissue) and T-cell lymphomas
Complications of EBV infection include—
- Peritonsillar abscesses (pus-filled tissue near the tonsils)
- Acute bacterial sinusitis (bacterial infection of the sinus cavities)
- Suppurative lymph nodes (swelling of lymph nodes)
- Mastoiditis (bacterial infection of the mastoid bone of the skull)
- Sialadenitis (swelling and injury of salivary glands)
- Blockage of the air passages in the nose and throat
Epstein-Barr virus (EBV), also known as human herpesvirus 4, is a gamma herpes virus that occurs only in humans. Laboratory testing can help distinguish whether someone is susceptible to EBV infection or has a recent or past infection.
Healthcare providers can test for antibodies to the following EBV-associated antigens:
This photomicrograph depicts leukemia cells that contain Epstein-Barr virus using a FA staining technique.
- Viral capsid antigen (VCA)Early antigen (EA)
- Anti-VCA IgM appears early in EBV infection and usually disappears within 4 to 6 weeks.
- Anti-VCA IgG appears in the acute phase of EBV infection, peaks at 2 to 4 weeks after onset, declines slightly then persists for the rest of a person’s life.
- Anti-EA IgG appears in the acute phase of illness and generally falls to undetectable levels after 3 to 6 months. In many people, detection of antibody to EA is a sign of active infection. However, 20% of healthy people may have antibodies against EA for years.
- EBV nuclear antigen (EBNA)
Antibody to EBNA, determined by the standard immunofluorescent test, is not seen in the acute phase of EBV infection but slowly appears 2 to 4 months after onset of symptoms and persists for the rest of a person’s life. Other EBNA enzyme immunoassays may report false positive results.
- Monospot test
The Monospot test is not recommended for general use. The antibodies detected by Monospot can be caused by conditions other than infectious mononucleosis. Moreover, studies have shown that the Monospot produces both false positive and false negative results. For example, the heterophile antibodies detected by Monospot are often not present in children with infectious mononucleosis. At best, the Monospot test may indicate that a person has a typical case of infectious mononucleosis, but does not confirm the presence of EBV infection.
Interpretation of EBV Antibody Tests
EBV antibody tests are not usually needed to diagnose infectious mononucleosis. However, specific antibody tests may be needed to identify the cause of illness in people who do not have a typical case of infectious mononucleosis or have other illnesses that can be caused by EBV infection. Symptoms of infectious mononucleosis generally resolve within 4 weeks. If a person is ill for more than 6 months and does not have a laboratory-confirmed diagnosis of EBV infection, other causes of chronic illness or chronic fatigue syndrome should be considered.
The interpretation of EBV antibody tests requires familiarity with these tests and access to the patient’s clinical information.
Interpretation of EBV antibody tests and diagnosis of EBV infection is summarized as follows:
- Susceptibility to infection
People are considered susceptible to EBV infection if they do not have antibodies to the VCA.
- Primary (new or recent) infection
People are considered to have a primary EBV infection if they have anti-VCA IgM but do not have antibody to EBNA. Other results that strongly suggest a primary infection are a high or rising level of anti-VCA IgG and no antibody to EBNA after at least 4 weeks of illness. Resolution of the illness may occur before the diagnostic antibody levels appear. In rare cases, people with active EBV infections may not have detectable EBV-specific antibodies.
- Past infection
The presence of antibodies to both VCA and EBNA suggests past infection (from several months to years earlier). Since over 90% of adults have been infected with EBV, most adults will show antibodies to EBV from infection years earlier. High or elevated antibody levels may be present for years and are not diagnostic of recent infection.
Testing paired acute- and convalescent-phase serum samples is not useful to distinguish between recent and past EBV infections. In most cases, the antibody response occurs rapidly during primary EBV infection. The clinical findings of infectious mononucleosis occur in conjunction with the appearance of IgG and IgM anti-VCA antibodies. However, the antibody pattern is not stable before symptoms appear.
CDC: Centers for Disease Control and Prevention
CONDITION: Giardiasis

Giardia is a microscopic parasite that causes the diarrheal illness known as giardiasis. Giardia (also known as Giardia intestinalis, Giardia lamblia, or Giardia duodenalis) is found on surfaces or in soil, food, or water that has been contaminated with feces (poop) from infected humans or animals.

Giardia is protected by an outer shell that allows it to survive outside the body for long periods of time and makes it tolerant to chlorine disinfection. While the parasite can be spread in different ways, water (drinking water and recreational water) is the most common mode of transmission.
Giardiasis (beaver fever)
Last Reviewed: September 2016

What is giardiasis?
Giardiasis is an intestinal (bowel) illness caused by a microscopic parasite called Giardia lamblia. It is a common illness that causes diarrhea (loose stool/poop). Over 2,000 cases occur in New York State each year.
Who gets giardiasis?
Giardiasis occurs more often in children and staff in daycare centers, foreign travelers, and people who drink improperly treated surface water. Men who have sex with men may also be at increased risk of getting giardiasis.
How is this parasite spread?
Giardia can infect people and wild and domestic animals. It is passed in the feces (poop) of an infected person or animal and may contaminate water or food. The beaver has gained attention as a potential source of Giardia contamination of lakes, reservoirs, and streams, but human fecal wastes are also play an important role in spreading the parasite. People become infected by accidently swallowing Giardia and can carry the parasite in their bodies from a few weeks to a few months. Spread of the parasite directly from one person to another may occur in daycare centers or other settings where handwashing practices are poor or through anal sex.
What are the symptoms of giardiasis and how soon do they appear?

People exposed to Giardia may experience mild or severe diarrhea (loose stool/poop), gas, stomach cramps, nausea (a feeling of upset in the stomach), or dehydration (loss of water in the body causing weakness of dizziness). Some people experience no symptoms at all. Fever is rarely present. Occasionally, some people will have chronic diarrhea over several weeks or months, with significant weight loss. The symptoms may appear from 3 to 25 days after exposure but usually within 10 days.
How is giardiasis diagnosed?
Giardiasis is diagnosed by testing samples of your stool (poop). Sometimes, several stool samples must be obtained because the number of Giardia being passed in the stool, which varies from day to day, may be too low to detect from any single sample.
What is the treatment for giardiasis?
Doctors commonly treat giardiasis by prescribing antibiotics such as metronidazole, tinidazole, or nitazoxanide. However, some individuals may recover on their own in a few weeks without medication.
What can be done to prevent the spread of giardiasis?

Three important preventive measures are:
- Carefully wash hands thoroughly with soap and water after toilet visits and handling soiled diapers.
- Carefully dispose of sewage wastes so as not to contaminate surface water or groundwater.
- Avoid consuming untreated water from springs, streams, or lakes.
Should an infected person be excluded from work or school?
People with active diarrhea (loose stool/poop) who are unable to control their bowel movements (infants and young children for example) may need to be excluded from settings such as daycare or group activities where they may present a risk to others. After they have been treated and have recovered, they may be permitted to return. Food handlers may not work while ill with Giardia. In addition, some local health departments may require follow-up stool (poop) testing to confirm that the person is no longer contagious. Individuals who are not in high-risk settings may return to their routine activities when they have recovered, if they carefully wash their hands with soap and water after each toilet visit.
NYS. Health Dept.
CONDITION: Genital herpes
What is genital herpes?

Genital herpes is a sexually transmitted infection (STI) caused by the herpes simplex viruses type 1 (HSV-1) or type 2 (HSV-2). Most genital herpes is caused by HSV-2. HSV-1 can cause genital herpes. But it more commonly causes infections of the mouth and lips, called “fever blisters.”
Most people have no or few symptoms from herpes infection. When symptoms do occur, they usually appear as 1 or more blisters on or around the genitals or rectum. The blisters break, leaving tender sores that may take up to 4 weeks to heal. Another outbreak can appear weeks or months later. But it almost always is less severe and shorter than the first outbreak.
Although the infection can stay in the body forever, the outbreaks tend to become less severe and occur less often over time. You can pass genital herpes to someone else even when you have no symptoms.
How common is genital herpes?

Genital herpes is common. At least 45 million Americans age 12 and older have genital herpes. Genital HSV-2 infection is more common in women than men. About 1 in 4 women have HSV-2 infection compared to almost 1 in 8 men. This is due to the fact that women can get genital herpes and some other STIs more easily than men.
How is genital herpes spread?

You can get genital herpes through genital-genital contact or genital-oral contact with someone who has herpes infection. The virus is most easily spread through contact with open sores. But you also can get the virus from skin that does not appear to have a sore. You can become infected with the herpes virus without having intercourse.
What are the symptoms of genital herpes?

Did you know?
If you have herpes, do not have any sexual activity with an uninfected partner when you have sores or other symptoms of herpes. Even if you don't have symptoms, you can still pass the virus to others.
The symptoms of genital herpes vary from person to person. Most people with genital herpes are not aware they are infected. But, if symptoms do occur with the first outbreak, they can be severe. Genital herpes infection also can be severe and long-lasting in people whose immune systems don't work properly, such as people with HIV.
The first outbreak usually happens within 2 weeks of having sexual contact with an infected person, and symptoms can last from 2 to 3 weeks. Early symptoms of the first outbreak can include:
- Itching or burning feeling in the genital or anal area
- Flu-like symptoms, including fever
- Swollen glands
- Pain in the legs, buttocks, or genital area
- Vaginal discharge
- A feeling of pressure in the area below the stomach
Within a few days, sores show up where the virus has entered the body, such as on the mouth, penis, or vagina. Sores can also show up on a woman's cervix or in the urinary passage in men. The sores are small red bumps that may turn into blisters or painful open sores. Over a period of days, the sores become crusted and then heal without scarring. Sometimes with the first outbreak, a second crop of sores appear and flu-like symptoms occur again.
Some people have no symptoms. Or they might mistaken mild sores for insect bites or something else. Yet even without symptoms, a person can still pass the herpes virus to others. So, if you have signs of herpes, see your doctor to find out if you are infected.
Can genital herpes come back?
Yes. Herpes symptoms can come and go, but the virus stays inside your body even after all signs of the infection have gone away. In most people, the virus becomes “active” from time to time, creating an outbreak. Some people have herpes virus outbreaks only once or twice. People who have a first outbreak can expect to have 4 or 5 outbreaks within a year. Over time, the outbreaks tend to occur less often and be less severe. Experts don't know what causes the virus to become active. Some women say the virus comes back when they are sick, under stress, out in the sun, or during their period.
How do I know for sure if I have genital herpes?
Doctors can diagnose genital herpes by looking at visible sores if the outbreak is typical and by taking a sample from the sore for testing in a lab. Some cases of herpes are harder to diagnose, especially between outbreaks. Blood tests that look for antibodies to HSV-1 or HSV-2 can help to detect herpes infection in people without symptoms or between outbreaks.
What is the treatment for genital herpes?
Genital herpes cannot be cured; the virus will always be in your body. But the antiviral drugs acyclovir, valacyclovir, and famciclovir can shorten outbreaks and make them less severe, or stop them from happening. Valacyclovir (brand name Valtrex) also can lower your risk of passing the infection to someone else.
Depending on your needs, your doctor can give you drugs to take right after getting outbreak symptoms or drugs to take on a regular basis to try to stop outbreaks from happening. Talk to your doctor about treatment options.
During outbreaks, these steps can speed healing and help keep the infection from spreading to other sites of the body or to other people:
- Keep the infected area clean and dry.
- Try not to touch the sores.
- Wash hands after contact.
- Avoid sexual contact from the time you first notice symptoms until the sores have healed.
Is there a cure for genital herpes?
No. Once you have the virus, it stays in your body and there is a chance that you will have outbreaks. Medicine can shorten and stop outbreaks from happening.
Research is underway to develop new ways to protect women from the herpes virus and prevent its spread. One large study is testing a herpes vaccine for women. Researchers are also working to make gels or creams that would kill the virus before it could infect someone.
Can genital herpes cause problems during pregnancy?
Yes. If the mother is having her first outbreak near the time of delivery, she is much more likely to pass the virus to her baby. If the outbreak is not the first one, the baby's risk of getting the virus is very low. Babies born with herpes may be premature or may die, or they may have brain damage, severe rashes, or eye problems. Doctors may do a cesarean delivery if the mother has herpes sores near the birth canal to lower the risk of passing the virus. Fortunately, most women with genital herpes have healthy babies. Also, medicines can help babies born with herpes if they are treated right away.
It is not yet known if all genital herpes drugs are safe for pregnant women to take. Some doctors may recommend acyclovir be taken either as a pill or through an IV (a needle into a vein) during pregnancy. Let your doctor know if you have genital herpes, even if you are not having an outbreak. He or she will help you manage it safely during pregnancy.
Can I breastfeed if I have genital herpes?
If you have genital herpes, you can keep breastfeeding as long as the sores are covered. Herpes is spread through contact with sores and can be dangerous to a newborn. If you have sores on your nipple or areola, the darker skin around the nipple, you should stop breastfeeding on that breast. Pump or hand express your milk from that breast until the sore clears. Pumping will help keep up your milk supply and prevent your breast from getting overly full. You can store your milk to give to your baby in a bottle at another feeding. If the parts of your breast pump that contact the milk also touch the sore(s) while pumping, you should throw the milk away.
Can genital herpes cause other problems?
Genital herpes infection usually does not cause serious health problems in healthy adults. People whose immune systems don't work properly, such as people with HIV, can have severe outbreaks that are long-lasting. Sometimes, people with normal immune systems can get herpes infection in the eye. But this is less common with HSV-2 infection.
Herpes may play a role in the spread of HIV, the virus that causes AIDS. Herpes sores can make it easier for HIV to get into your body. Also, herpes can make people who are HIV-positive more infectious.
Living with herpes can be hard to cope with even if you have no symptoms. At first, you might feel embarrassed or ashamed. You might worry whether having herpes will affect your relationship with your sexual partner or keep you from having meaningful relationships in the future. Keep in mind that millions of people have herpes. And not unlike many other health issues, treatment can help you manage the infection. After a little time, most people with herpes are able to adjust to the diagnosis and move on. Let your doctor know if you're having a hard time adjusting. Talking to someone about your feelings may help.
What can I do to keep from getting genital herpes?
There are things you can do to lower your risk of getting genital herpes:
- Don't have sex. The surest way to prevent any STI, including genital herpes, is to practice abstinence, or not having vaginal, oral, or anal sex. Keep in mind, you can get genital herpes from close contact other than sexual intercourse.
- Be faithful. Having a sexual relationship with one partner who has been tested for herpes and is not infected is another way to lower your risk of getting infected. Be faithful to each other, meaning that you only have sex with each other and no one else.
- Use condoms. Use condoms correctly and every time you have any type of sex. For vaginal sex, use a latex male condom or a female polyurethane condom. For anal sex, use a latex male condom. For oral sex, use a dental dam. Keep in mind that condoms may not cover all infected areas, so you can still get herpes even if you use a condom.
- Know that some methods of birth control, like birth control pills, shots, implants, or diaphragms, will not protect you from STIs. If you use one of these methods, be sure to also use a latex condom or dental dam correctly and every time you have sex.
- Talk with your sex partner(s) about STIs and using condoms. It's up to you to make sure you are protected. Remember, it's your body! For more information, call the Centers for Disease Control and Prevention at 800-232-4636. If your partner is infected, take steps to lower your risk of getting herpes from your partner.
- Talk frankly with your doctor and your sex partner(s) about any STIs you or your partner has or has had. If you feel embarrassed, try to put this aside. Your doctor is there to help you with any and all health problems. Also, being open with your partners can help you protect your health and the health of others.
- Know the symptoms. Learn the common symptoms of genital herpes and other STIs. Do not have oral-genital contact if you or your partner has any signs of oral herpes, such as a fever blister. Seek medical help right away if you think you may have genital herpes or another STI. Don't have sexual contact until you have seen your doctor.
What should I do if I have genital herpes?
- See your doctor for testing and treatment right away.
- Follow your doctor's orders and finish all the medicine that you are given. Even if the symptoms go away, you still need to finish all of the medicine.
- Avoid having any sexual activity while you are being treated for genital herpes and while you have any symptoms of an outbreak.
- Be sure to tell your sexual partners, so they can be tested.
- Remember that genital herpes is a life-long disease. Even though you may have long periods with no symptoms, you can still pass the virus to another person. Talk with your doctor about what you can do to have fewer future outbreaks, and how to prevent passing the virus to another person.
What should I do if my partner has genital herpes?
- Get tested to find out if you also are infected with the herpes virus.
- Avoid having any sexual activity while your partner is being treated for a genital herpes outbreak or if your partner has symptoms of an outbreak, such as open sores.
- Use condoms correctly and every time you have sex to lower your risk of becoming infected. Keep in mind that you can become infected with the herpes virus since condoms do not always cover all infected areas. Also, the virus can spread even if no symptoms are present.
- Talk to your partner about using daily suppressive therapy to reduce the number of outbreaks and lower the risk of infecting you with the virus.
More information on genital herpes
Genital herpes fact sheet (PDF, 129 KB)
For more information about genital herpes, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
- Herpes Resource Center, ASHA
Phone: 800-230-6039
- National Institute of Allergy and Infectious Diseases, NIH, HHS
Phone: 866-284-4107
- Sexually Transmitted Diseases (STDs), CDC, HHS
Phone: 800-CDC-INFO (232-6348
Source: Office of Women's Health, HHS
Genital Herpes - CDC Fact Sheet

Herpes is a common sexually transmitted disease (STD) that any sexually active person can get. Most people with the virus don’t have symptoms. It is important to know that even without signs of the disease, it can still spread to sexual partners.
What is genital herpes?
Genital herpes is an STD caused by two types of viruses. The viruses are called herpes simplex type 1 and herpes simplex type 2.
How common is genital herpes?
Genital herpes is common in the United States. In the United States, about one out of every six people aged 14 to 49 years have genital herpes.
How is genital herpes spread?
You can get herpes by having vaginal, anal, or oral sex with someone who has the disease.
Fluids found in a herpes sore carry the virus, and contact with those fluids can cause infection. You can also get herpes from an infected sex partner who does not have a visible sore or who may not know he or she is infected because the virus can be released through your skin and spread the infection to your sex partner(s).
How can I reduce my risk of getting herpes?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting herpes:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
Herpes symptoms can occur in both male and female genital areas that are covered by a latex condom. However, outbreaks can also occur in areas that are not covered by a condom so condoms may not fully protect you from getting herpes.
I'm pregnant. How could genital herpes affect my baby?
If you are pregnant and have genital herpes, it is even more important for you to go to prenatal care visits. You need to tell your doctor if you have ever had symptoms of, been exposed to, or been diagnosed with genital herpes. Sometimes genital herpes infection can lead to miscarriage. It can also make it more likely for you to deliver your baby too early. Herpes infection can be passed from you to your unborn child and cause a potentially deadly infection (neonatal herpes). It is important that you avoid getting herpes during pregnancy.
If you are pregnant and have genital herpes, you may be offered herpes medicine towards the end of your pregnancy to reduce the risk of having any symptoms and passing the disease to your baby. At the time of delivery your doctor should carefully examine you for symptoms. If you have herpes symptoms at delivery, a ‘C-section’ is usually performed.
How do I know if I have genital herpes?
Most people who have herpes have no, or very mild symptoms. You may not notice mild symptoms or you may mistake them for another skin condition, such as a pimple or ingrown hair. Because of this, most people who have herpes do not know it.
Genital herpes sores usually appear as one or more blisters on or around the genitals, rectum or mouth. The blisters break and leave painful sores that may take weeks to heal. These symptoms are sometimes called “having an outbreak.” The first time someone has an outbreak they may also have flu-like symptoms such as fever, body aches, or swollen glands.
Repeat outbreaks of genital herpes are common, especially during the first year after infection. Repeat outbreaks are usually shorter and less severe than the first outbreak. Although the infection can stay in the body for the rest of your life, the number of outbreaks tends to decrease over a period of years.
You should be examined by your doctor if you notice any of these symptoms or if your partner has an STD or symptoms of an STD, such as an unusual sore, a smelly discharge, burning when urinating, or, for women specifically, bleeding between periods.
How will my doctor know if I have herpes?
Often times, your healthcare provider can diagnose genital herpes by simply looking at your symptoms. Providers can also take a sample from the sore(s) and test it. Have an honest and open talk with your health care provider and ask whether you should be tested for herpes or other STDs.
Can herpes be cured?
There is no cure for herpes. However, there are medicines that can prevent or shorten outbreaks. One of these herpes medicines can be taken daily, and makes it less likely that you will pass the infection on to your sex partner(s).
What happens if I don't get treated?
Genital herpes can cause painful genital sores and can be severe in people with suppressed immune systems. If you touch your sores or the fluids from the sores, you may transfer herpes to another part of your body, such as your eyes. Do not touch the sores or fluids to avoid spreading herpes to another part of your body. If you touch the sores or fluids, immediately wash your hands thoroughly to help avoid spreading your infection.
Some people who get genital herpes have concerns about how it will impact their overall health, sex life, and relationships. It is best for you to talk to a health care provider about those concerns, but it also is important to recognize that while herpes is not curable, it can be managed. Since a genital herpes diagnosis may affect how you will feel about current or future sexual relationships, it is important to understand how to talk to sexual partners about STDs. You can find one resource here: GYT Campaign.
If you are pregnant, there can be problems for you and your unborn child. See “I’m pregnant. How could genital herpes affect my baby?” above for information about this.
Can I still have sex if I have herpes?
If you have herpes, you should tell your sex partner(s) and let him or her know that you do and the risk involved. Using condoms may help lower this risk but it will not get rid of the risk completely. Having sores or other symptoms of herpes can increase your risk of spreading the disease. Even if you do not have any symptoms, you can still infect your sex partners.
What is the link between genital herpes and HIV?
Genital herpes can cause sores or breaks in the skin or lining of the mouth, vagina, and rectum. The genital sores caused by herpes can bleed easily. When the sores come into contact with the mouth, vagina, or rectum during sex, they increase the risk of giving or getting HIV if you or your partner has HIV.
What is the link between genital herpes and oral herpes (cold sores on the mouth)?
Oral herpes (such as cold sores or fever blisters on or around the mouth) is usually caused by HSV-1. Most people are infected with HSV-1 during childhood from non-sexual contact. For example, people can get infected from a kiss from a relative or friend with oral herpes. More than half of the population in the U.S. has HSV-1, even if they don’t show any signs or symptoms. HSV-1 can also be spread from the mouth to the genitals through oral sex. This is why some cases of genital herpes are caused by HSV-1.
Resources:
CDC National Prevention Information Network (NPIN)
P.O. Box 6003
Rockville, MD 20849-6003
E-mail: npin-info@cdc.gov
American Sexual Health Association (ASHA)
P. O. Box 13827
Research Triangle Park, NC 27709-3827
1-800-783-9877
Source: CDC
CONDITION: Human Papillomavirus & Genital Warts
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States. Some health effects caused by HPV can be prevented with vaccines.

What is HPV?
HPV is the most common sexually transmitted infection (STI). HPV is a different virus than HIV and HSV (herpes). HPV is so common that nearly all sexually active men and women get it at some point in their lives. There are many different types of HPV. Some types can cause health problems including genital warts and cancers. But there are vaccines that can stop these health problems from happening.
How is HPV spread?
You can get HPV by having vaginal, anal, or oral sex with someone who has the virus. It is most commonly spread during vaginal or anal sex. HPV can be passed even when an infected person has no signs or symptoms.
Anyone who is sexually active can get HPV, even if you have had sex with only one person. You also can develop symptoms years after you have sex with someone who is infected making it hard to know when you first became infected.
Does HPV cause health problems?
In most cases, HPV goes away on its own and does not cause any health problems. But when HPV does not go away, it can cause health problems like genital warts and cancer.
Genital warts usually appear as a small bump or group of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower. A healthcare provider can usually diagnose warts by looking at the genital area.
Does HPV cause cancer?
HPV can cause cervical and other cancers including cancer of the vulva, vagina, penis, or anus. It can also cause cancer in the back of the throat, including the base of the tongue and tonsils (called oropharyngeal cancer).
Cancer often takes years, even decades, to develop after a person gets HPV. The types of HPV that can cause genital warts are not the same as the types of HPV that can cause cancers.
There is no way to know which people who have HPV will develop cancer or other health problems. People with weak immune systems (including individuals with HIV/AIDS) may be less able to fight off HPV and more likely to develop health problems from it.
How can I avoid HPV and the health problems it can cause?
You can do several things to lower your chances of getting HPV.
Get vaccinated. HPV vaccines are safe and effective. They can protect males and females against diseases (including cancers) caused by HPV when given in the recommended age groups (see “Who should get vaccinated?” below). HPV vaccines are given in three shots over six months; it is important to get all three doses.
Get screened for cervical cancer. Routine screening for women aged 21 to 65 years old can prevent cervical cancer.
If you are sexually active
- Use latex condoms the right way every time you have sex. This can lower your chances of getting HPV. But HPV can infect areas that are not covered by a condom - so condoms may not give full protection against getting HPV;
- Be in a mutually monogamous relationship – or have sex only with someone who only has sex with you.
Who should get vaccinated?
All boys and girls ages 11 or 12 years should get vaccinated.
Catch-up vaccines are recommended for males through age 21 and for females through age 26, if they did not get vaccinated when they were younger.
The vaccine is also recommended for gay and bisexual men (or any man who has sex with a man) through age 26. It is also recommended for men and women with compromised immune systems (including people living with HIV/AIDS) through age 26, if they did not get fully vaccinated when they were younger.
How do I know if I have HPV?
There is no test to find out a person’s “HPV status.” Also, there is no approved HPV test to find HPV in the mouth or throat.
There are HPV tests that can be used to screen for cervical cancer. These tests are recommended for screening only in women aged 30 years and older. They are not recommended to screen men, adolescents, or women under the age of 30 years.
Most people with HPV do not know they are infected and never develop symptoms or health problems from it. Some people find out they have HPV when they get genital warts. Women may find out they have HPV when they get an abnormal Pap test result (during cervical cancer screening). Others may only find out once they’ve developed more serious problems from HPV, such as cancers.
How common is HPV and the health problems caused by HPV?
HPV (the virus): About 79 million Americans are currently infected with HPV. About 14 million people become newly infected each year. HPV is so common that most sexually-active men and women will get at least one type of HPV at some point in their lives.
Health problems related to HPV include genital warts and cervical cancer.
Genital warts: About 360,000 people in the United States get genital warts each year.
Cervical cancer: More than 11,000 women in the United States get cervical cancer each year.
There are other conditions and cancers caused by HPV that occur in persons living in the United States.
I'm pregnant. Will having HPV affect my pregnancy?
If you are pregnant and have HPV, you can get genital warts or develop abnormal cell changes on your cervix. Abnormal cell changes can be found with routine cervical cancer screening. You should get routine cervical cancer screening even when you are pregnant.
Can I be treated for HPV or health problems caused by HPV
There is no treatment for the virus itself. However, there are treatments for the health problems that HPV can cause:
- Genital warts can be treated by you or your physician. If left untreated, genital warts may go away, stay the same, or grow in size or number.
- Cervical precancer can be treated. Women who get routine Pap tests and follow up as needed can identify problems before cancer develops. Prevention is always better than treatment. For more information visit www.cancer.org.
- Other HPV-related cancers are also more treatable when diagnosed and treated early. For more information visit www.cancer.org.
Source: CDC
CONDITION: Genital Warts (Venereal warts, HPV)
What are genital warts?
This sexually transmitted disease (STD) infects the skin. Genital warts are also called venereal warts or HPV.
What causes genital warts?

Genital warts are caused by one of the most common viruses in the United States - the human papillomavirus (HPV). There are more than 100 types of HPV. Over 40 types can infect the genital area, mouth or throat.

How is HPV spread?
HPV is spread when infected skin touches an area of uninfected skin (called skin-to-skin contact). You can get HPV from someone who has warts on his or her mouth, skin or genitals. The virus can still rub off a person's skin even when he or she has no warts that you can see. Remember: You can get or give warts even when both of you have no signs or symptoms.
HPV cannot be spread by touching hard surfaces, like a doorknob or toilet seat. It also cannot be passed by sharing clothes or towels.
What problems can HPV cause?

Certain types of HPV can lead to cervical cancer (the cervix is the narrow, open end of the uterus) in females, or cancer of the penis in males. Some types of HPV may also lead to anal cancer.
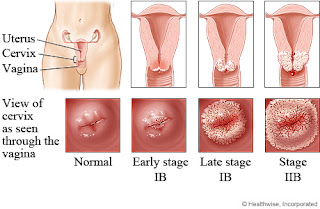
More commonly, HPV causes genital warts, which are soft, fleshy bumps that vary in size and shape. They can appear on or around the penis or the scrotum (the pouch of skin that contains the testicles). They can also appear on or around the vagina, anus, mouth or inside the body where they cannot easily be seen. The warts will be the color of your skin and cauliflower-shaped. Most people with genital warts do not have warts that can be seen with the naked eye.
In some pregnant females, or people with HIV, warts can become quite large. Some pregnant females with large warts may need a Cesarean delivery (C-section).
If a pregnant female has genital warts when she gives birth, the virus can sometimes infect the infant. It is very rare, but the infant may get warts inside their mouth or throat a few weeks after birth. This is most common in infants of young females who get HPV for the first time late in their pregnancies.
What are the signs and symptoms?
Most people with the genital wart virus (HPV) have no signs or symptoms of infection. When someone does have signs of infection, the warts:
- Usually appear 1 to 3 months after someone is exposed, but it may take longer.
- Begin as small red bumps that may grow larger.
- Can appear on any damp or moist areas of the body. This includes the vagina or vulva, penis, and anus.
- Are usually painless, but if the warts are injured, they may become painful or tender when touched.
Sometimes the virus may cause an unusual fluid (discharge) from the vagina or an itchy vulva. The vulva is the outer part of a female's genitals.
How will I know if I have genital warts?
If you have warts or red bumps on your genitals, you should visit your health care provider for a checkup. Your provider can usually look at the area and tell you if they are genital warts. Your provider may do additional tests based on your age.
How can I prevent HPV?
Not having sex (abstinence) is the only sure way to avoid infection. If you are sexually active, you can lower your chances of giving or getting genital warts by limiting the number of people you have sex with. Latex or polyurethane condoms should be used each time you have oral, vaginal or anal sex. Another option is using a female condom during vaginal sex or dental dams during oral sex. You should not use a male and a female condom at the same time.
Using condoms will not totally stop the risk of giving or getting genital warts because HPV may appear on parts of the body not covered by the condom. Condoms also help prevent the spread of other STDs including HIV, the virus that causes AIDS.
There is currently a vaccine (Gardasil®) that protects against genital warts. This vaccine protects against 2 types of HPV that cause most genital warts. It also protects against the 2 types of HPV that cause most cervical cancers in females. The vaccine is given in 3 doses. It is available for males and females age 9 through 26 years. Doctors recommend that the vaccine be given before someone becomes sexually active (before they can be exposed to HPV).The vaccine does not prevent or treat genital warts or cervical cancer if someone is already infected.
Another vaccine (Cervarix®) protects against the 2 types of HPV that cause most cervical cancers in females. This vaccine does not protect against genital warts. It is recommended for females age 9 through 26 years. It is not currently available for boys and young men.
Is there a cure?
No. HPV is a chronic, lifelong infection. However, as many as 1 out of every 3 people with genital warts find that they go away on their own - usually within 2 years. If you want your warts removed, do not do it yourself. A health care provider may be able to:
- Freeze the warts with liquid nitrogen, or
- Use laser surgery, or
- Destroy the warts with a chemical or acid medicine.
Your provider may prescribe a medicine that you can apply yourself. It is called imiquimod (I mi kwi' mod) or Aldara™ cream. Aldara™ helps your body to destroy the virus. You can apply the medicine directly to the warts. However, you should not use Aldara™ for warts on the cervix or inside the vagina or anus.
These options only treat the warts. They do not destroy the virus or the infection. Even if your warts disappear, they may return because the virus may be hidden in nearby, normal looking skin.
What about my partner(s)?
HPV is an STD. Because of this, your sex partner(s) should be checked for symptoms. Even though your partner(s) may not have symptoms that can be seen, he or she still needs to be checked for HPV and other STDs.
When can I have sex again?
You should wait to have sex for 2 weeks after the warts have gone away and the area has healed. You should also tell your current and future sex partner(s) that you have genital warts. Remember: you can spread HPV even when you do not have any symptoms or cannot see any warts.
Am I at risk for other STDs including HIV?
You may be at risk for other STDs, including HIV, because they can all be passed from person to person during sex. If you are sexually active, you and your partner(s) should get a full physical checkup. This includes a complete sexual history and testing for common STDs. You should be checked for gonorrhea, Chlamydia, syphilis, genital herpes, genital warts, trichomoniasis, viral hepatitis and HIV.
The test results and any treatment will be kept absolutely confidential. No one can find out your results, except you. If you are under 18, you can be checked and treated without getting your parent's permission.
To learn more
If you have any more questions about genital warts, or you want to know how to get tested, call your local health department or family planning program.
You can also find a testing center near you at www.findSTDtest.org or by calling 1-800-541-2437.
For more information on HPV and men, visit the CDC's "HPV for Men" fact sheet.
NYS Health Dept
CONDITION: The Human papillomavirus & Genital Warts
What is human papillomavirus (HPV)?
Human papillomavirus (pap-uh-LOH-muh-veye-ruhss), or HPV, is the name for a group of viruses that includes more than 100 types. More than 40 types of HPV can be passed through sexual contact.
The types of HPV that infect the genital area are called genital HPV. Over half of sexually active people will have HPV at some point in their lives. But most people never know it. This is because HPV most often has no symptoms and goes away on its own.
How many people have HPV?
Genital HPV is the most common sexually transmitted infection (STI) in the United States. About 20 million Americans ages 15 to 49 currently have HPV. And at least half of all sexually active men and women get genital HPV at some time in their lives.
What is the difference between the high-risk and low-risk types of HPV?
Some types of HPV can cause cervical cancer. These types of HPV are called high-risk. Having high-risk HPV is not the same as having cervical cancer. But high-risk HPV can lead to cancer. Most often, high-risk HPV causes no health problems and goes away on its own. High-risk HPV cases that don’t go away are the biggest risk factor for cervical cancer. If you have high-risk HPV, your doctor can look for changes on your cervix during Pap tests. Changes can be treated to try to prevent cervical cancer. Be sure to have regular Pap tests so changes can be found early.
Low-risk HPV can cause genital warts. Warts can form weeks, months, or years after sexual contact with an infected person. In women genital warts can grow:
- Inside and around the outside of the vagina
- On the vulva ("lips" or opening to the vagina), cervix, or groin
- In or around the anus
In men, genital warts can grow:
- On the penis
- On the scrotum, thigh, or groin
- In or around the anus
Rarely, genital warts grow in the mouth or throat of a person who had oral sex with an infected person.
The size of genital warts varies. Some are so small you can't see them. They can be flat and flesh-colored or look bumpy like cauliflower. They often form in clusters or groups. They may itch, burn, or cause discomfort.
Low-risk HPV doesn’t always cause warts. In fact, most people with low-risk HPV never know they are infected. This is because they don't get warts or any other symptoms.
How do women get HPV?
Genital HPV is passed by skin-to-skin and genital contact. It is most often passed during vaginal and anal sex. Although much less common, it is possible to pass HPV during oral sex or hand to genital contact.
Should I get the HPV vaccine?
It depends on your age and whether or not you already have had sex.
Two vaccines (Cervarix and Gardasil) can protect girls and young women against the types of HPV that cause most cervical cancers. The vaccines work best when given before a person's first sexual contact, when she could be exposed to HPV. Both vaccines are recommended for 11 and 12 year-old girls. But the vaccines also can be used in girls as young as 9 and in women through age 26 who did not get any or all of the shots when they were younger. These vaccines are given in a series of 3 shots. It is best to use the same vaccine brand for all 3 doses. Ask your doctor which brand vaccine is best for you. The vaccine does not replace the need to wear condoms to lower your risk of getting other types of HPV and other sexually transmitted infections. Women who have had the HPV vaccine still need to have regular Pap tests.
Studies are also being done on HPV vaccines for males.
How do I know if I have an HPV infection?
Most women who have HPV infections never know it. This is one reason why you need regular Pap tests. A Pap test is when a cell sample is taken from your cervix and looked at with a microscope.
A Pap test can find changes on the cervix caused by HPV. To do a Pap test, your doctor will use a small brush to take cells from your cervix. It’s simple, fast, and the best way to find out if your cervix is healthy.
If you are age 30 or older, your doctor may also do an HPV test with your Pap test. This is a DNA test that detects most of the high-risk types of HPV. It helps with cervical cancer screening. If you’re younger than 30 years old and have had an abnormal Pap test result, your doctor may give you an HPV test. This test will show if HPV caused the abnormal cells on your cervix.
One other way to tell if you have an HPV infection is if you have genital warts. (See What is the difference between the high-risk and low-risk types of HPV? for more details.)
Do I still need a Pap test if I got the HPV vaccine?
Yes. There are three reasons why:
- The vaccine does not protect against all HPV types that cause cancer.
- Women who don’t get all the vaccine doses (or at the right time) might not be fully protected.
- Women may not fully benefit from the vaccine if they got it after getting one or more of the four HPV types.
How often should I get a Pap test?
Follow these guidelines:
- Have a Pap test every 2 years starting at age 21. Women 30 and older who have had three normal Pap tests in a row can now have one every 3 years.
- If you are older than 65, you may be able to stop having Pap tests. Discuss your needs with your doctor.
- If you had your cervix taken out as part of a hysterectomy, you do not need further Pap tests if the surgery was not due to cancer.
- Talk with your doctor or nurse about when to begin testing, how often you should be tested, and when you can stop.
What happens if I have an abnormal Pap test?
An abnormal result does not mean you have HPV or cervical cancer. Other reasons for an abnormal Pap test result include:
- Yeast infections
- Irritation
- Hormone changes
If your Pap test is abnormal, your doctor may do the test again. You may also have an HPV test or these tests:
- Colposcopy. A device is used to look closely at your cervix. It lets the doctor look at any abnormal areas.
- Schiller test. The test involves coating the cervix with an iodine solution. Healthy cells turn brown and abnormal cells turn white or yellow.
- Biopsy. A small amount of cervical tissue is taken out and looked at under a microscope. This way the doctor can tell if the abnormal cells are cancer.
Could I have HPV even if my Pap test was normal?
Yes. You can have HPV but still have a normal Pap test. Changes on your cervix may not show up right away; or they may never appear. For women older than 30 who get an HPV test and a Pap test, a negative result on both the Pap and HPV tests means no cervical changes or HPV were found on the cervix. This means you have a very low chance of getting cervical cancer in the next few years.
Can HPV be cured?
No. There is no cure for the virus HPV. But there are treatments for the changes HPV can cause on the cervix. Genital warts can also be treated. Sometimes, the virus goes away on its own.
What treatments are used to get rid of abnormal cells on the cervix?
If you have abnormal cells on the cervix, follow up with your doctor. If the problem is mild, your doctor may wait to see if the cells heal on their own. Or your doctor may suggest taking out the abnormal tissue. Treatment options include:
- Cryosurgery, when abnormal tissue is frozen off.
- Loop electrosurgical excision procedure (LEEP), where tissue is removed using a hot wire loop.
- Laser treatment, which uses a beam of light to destroy abnormal tissue.
- Cone biopsy, where a cone-shaped sample of abnormal tissue is removed from the cervix and looked at under the microscope for signs of cancer. This biopsy also can serve as a treatment if all the abnormal tissue is removed.
After these treatments, you may have:
- Vaginal bleeding
- Cramping
- Brownish-black discharge
- Watery discharge
After treatment, follow up with your doctor to see if any abnormal cells come back.
How are genital warts treated?
Genital warts can be treated or not treated.
Some people may want warts taken off if they cause itching, burning, and discomfort. Others may want to clear up warts you can see with the eye.
If you decide to have warts removed, do not use over-the-counter medicines meant for other kinds of warts. There are special treatments for genital warts. Your doctor may treat the warts by putting on a chemical in the office. Or your doctor may prescribe a cream you can apply at home. Surgery is also an option. Your doctor may:
- Use an electric current to burn off the warts
- Use a light/laser to destroy warts
- Freeze off the warts
- Cut the warts out
Even when warts are treated, the HPV virus may remain. This is why warts can come back after treatment. It isn’t clear if treating genital warts lowers a person's chance of giving HPV to a sex partner. It is not fully known why low-risk HPV causes genital warts in some cases and not in others.
If left untreated, genital warts may:
- Go away
- Remain unchanged
- Increase in size or number
The warts will not turn into cancer.
What about HPV in men?
HPV is as common in men as in women. HPV rarely causes severe health problems in men. But it can lead to anal cancer in men who have sex with men. There is no test for HPV in men.
How do I protect myself from HPV?
Using condoms may reduce the risk of getting genital warts and cervical cancer. But condoms don’t always protect you from HPV. The best ways to protect yourself from HPV are to:
- Not have sex
- Be faithful, meaning you and your partner only have sex with each other and no one else
If I had HPV that went away on its own, can I get it again?
Yes. There are many types of HPV, so you can get HPV again.
How do I protect my partner from HPV after my warts have gone away?
Even if you think the warts have gone away, there may be some you can’t see. And even after the warts are treated, the HPV virus may remain. Using condoms may reduce your risk of passing on genital warts.
How does HPV affect a pregnancy?
Most women who had genital warts, but no longer have them, do not have problems during pregnancy or birth. For women who have genital warts during pregnancy, the warts may grow or become larger and bleed. In rare cases, a pregnant woman can pass HPV to her baby during vaginal delivery. Rarely, a baby who is exposed to HPV gets warts in the throat or voice box.
If the warts block the birth canal, a woman may need to have a cesarean section (C-section) delivery. But HPV infection or genital warts are not sole reasons for a C-section.
How can I be sure I don’t get cervical cancer?
While there are no sure ways to prevent cervical cancer, you can lower your risk by:
- Getting regular Pap tests. The best time to get a Pap test is 10 to 20 days after the first day of your last period. Don’t have the test done during your period. Also, for 2 days before your Pap test don’t have sex or use douches, vaginal medicines (unless your doctor tells you to), or spermicides. Talk to your doctor about how often to get Pap tests.
- Not smoking. Smoking can raise your risk of cervical cancer.
- Being faithful. This means you and your partner only have sex with each other and no one else.
- Using a condom EVERY time you have vaginal, anal, or oral sex. Condoms don’t always protect you from HPV. But they may reduce your risk of getting genital warts and cervical cancer.
More information on human papillomavirus (HPV) and genital warts
For more information about human papillomavirus (HPV) and genital warts, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
- CDC National Breast and Cervical Cancer Early Detection Program, HHS
Phone: 800-323-4636 (TDD: 888-232-6348)
- National Cancer Institute, NIH, HHS
Phone: 800-422-6237
- National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC
Phone: 800-232-4636 (TDD: 888-232-6348)
- National Institute of Allergy and Infectious Diseases, NIH, HHS
Phone: 866-284-4107 or 301-496-5717 (TDD: 800-877-8339)
Source: Office on Women's Health
Questions and Answers: Q&A About the Health Effects of HPV
Q: How common are HPV infections?
A: HPV infections are so common that nearly all men and women will get at least one type of HPV at some point in their lives. Most people never know that they have been infected and may give HPV to a sex partner without knowing it. About 79 million Americans are currently infected with some type of HPV. About 14 million people in the United States become newly infected each year.
Q: What kinds of problems does HPV infection cause?
A: Most people with HPV never develop symptoms or health problems. Most HPV infections (9 out of 10) go away by themselves within two years. But, sometimes, HPV infections will last longer, and can cause certain cancers and other diseases. HPV infections can cause:
- cancers of the cervix, vagina, and vulva in women;
- cancers of the penis in men; and
- cancers of the anus and back of the throat, including the base of the tongue and tonsils (oropharynx), in both women and men. Every year in the United States, HPV causes 30,700 cancers in men and women.
Q: How do people get an HPV infection?
A: People get HPV from another person during intimate sexual contact. Most of the time, people get HPV from having vaginal and/or anal sex. Men and women can also get HPV from having oral sex or other sex play. A person can get HPV even if their partner doesn’t have any signs or symptoms of HPV infection. A person can have HPV even if years have passed since he or she had sexual contact with an infected person. Most people do not realize they are infected. They also don’t know that they may be passing HPV to their sex partner(s). It is possible for someone to get more than one type of HPV.
It's not very common, but sometimes a pregnant woman with HPV can pass it to her baby during delivery. The child might develop recurrent respiratory papillomatosis (RRP), a rare but dangerous condition where warts caused by HPV (similar to genital warts) grow inside the throat.
There haven’t been any documented cases of people getting HPV from surfaces in the environment, such as toilet seats. However, someone could be exposed to HPV from objects (toys) shared during sexual activity if the object has been used by an infected person.
Q: Who should get HPV vaccine?
A: All girls and boys who are 11 or 12 years old should get the recommended series of HPV vaccine. The vaccination series can be started at age 9 years. Teen boys and girls who did not get vaccinated when they were younger should get it now. HPV vaccine is recommended for young women through age 26, and young men through age 21. HPV vaccine is also recommended for the following people, if they did not get vaccinated when they were younger:
- young men who have sex with men, including young men who identify as gay or bisexual or who intend to have sex with men through age 26;
- young adults who are transgender through age 26; and
- young adults with certain immunocompromising conditions (including HIV) through age 26.
Q: Why are two doses recommended for 9–14 year olds, while older adolescents need three doses?
A: Since 2006, HPV vaccines have been recommended in a three-dose series given over six months. In 2016, CDC changed the recommendation to two doses for persons starting the series before their 15th birthday. The second dose of HPV vaccine should be given six to twelve months after the first dose. Adolescents who receive their two doses less than five months apart will require a third dose of HPV vaccine.
Teens and young adults who start the series at ages 15 through 26 years still need three doses of HPV vaccine Also, three doses are still recommended for people with certain immunocompromising conditions aged 9 through 26 years.
CDC makes recommendations based on the best available scientific evidence. Studies have shown that two doses of HPV vaccine given at least six months apart to adolescents at age 9–14 years worked as well or better than three doses given to older adolescents and young adults. Studies have not been done to show this for adolescents starting the series at age 15 years or older.
Q: Why is HPV vaccine recommended at age 11 or 12 years?
A: For HPV vaccine to be most effective, the series should be given prior to exposure to HPV. There is no reason to wait to vaccinate until teens reach puberty or start having sex. Preteens should receive all recommended doses of the HPV vaccine series long before they begin any type of sexual activity.
Q: How well does HPV vaccine work?
A: HPV vaccines work extremely well. Clinical trials showed HPV vaccines provide close to 100% protection against cervical precancers and genital warts. Since the first HPV vaccine was recommended in 2006, there has been a 64% reduction in vaccine-type HPV infections among teen girls in the United States. Studies have shown that fewer teens are getting genital warts and cervical precancers are decreasing. In other countries, such as Australia, where HPV vaccination coverage is higher than in the United States, large decreases have been observed in these HPV-associated outcomes. HPV vaccines offer long-lasting protection against HPV infection and HPV disease. There has been no evidence to suggest that HPV vaccine loses any ability to provide protection over time. Data are available for about 10 years of follow-up after vaccination.
Like all vaccines, HPV vaccine is monitored on an ongoing basis to make sure it remains safe and effective. If it turns out that protection from HPV vaccine is not long-lasting, then the Advisory Committee on Immunization Practices would review the data and determine whether a booster dose would be recommended.
Even if it has been months or years since the last shot, the HPV vaccine series should be completed—but they do not need to restart the series.
HPV vaccine is recommended based on age, not sexual experience. Even if someone has already had sex, they should still get HPV vaccine. Even though a person’s first HPV infection usually happens during one of the first few sexual experiences, a person might not be exposed to all of the HPV types that are covered by HPV vaccines.
Q: Does HPV vaccination offer similar protection from cervical cancer in all racial/ethnic groups?
A: Yes. Several different HPV types cause cervical cancer. HPV vaccines are designed to prevent the HPV types that cause most cervical cancers, so HPV vaccination will provide high protection for all racial/ethnic groups.
All three licensed HPV vaccines protect against types 16 and 18, which cause the majority of cervical cancers across racial/ethnic groups (67% of the cervical cancers among whites, 68% among blacks, and 64% among Hispanics). The 9-valent HPV vaccine protects against seven HPV types that cause about 80% of cervical cancer among all racial/ethnic groups in the United States.
Teens and young adults who haven’t completed the HPV vaccine series should make an appointment today to get vaccinated. To protect against cervical cancer, women age 21–65 years should get screened for cervical cancer at regular intervals and get follow-up care as recommended by their doctor or nurse.
Q: How do we know that the HPV vaccine is safe?
A: The United States currently has the safest, most effective vaccine supply in history. Years of testing are required by law to ensure the safety of vaccines before they are made available for use in the United States. This process can take ten years or longer. Once a vaccine is in use, CDC and the Food and Drug Administration (FDA) monitor any associated side effects or possible side effects (adverse events) through the Vaccine Adverse Event Reporting System and other vaccine safety systems.
All three HPV vaccines—Cervarix®, Gardasil®, and Gardasil® 9—went through years of extensive safety testing before they were licensed by FDA. Cervarix® was studied in clinical trials with more than 30,000 females. Gardasil® trials included more than 29,000 females and males, and Gardasil® 9 trials included more than 15,000 females and males. No serious safety concerns were identified in these clinical trials. FDA only licenses a vaccine if it is safe, effective, and the benefits outweigh the risks. CDC and FDA continue to monitor HPV vaccines to make sure they are safe and beneficial for the public.
Q: What are the possible side effects of HPV vaccination?
A: Vaccines, like any medicine, can have side effects. Many people who get HPV vaccine have no side effects at all. Some people report having very mild side effects, like a sore arm. The most common side effects are usually mild. Common side effects of HPV vaccine include:
- Pain, redness, or swelling in the arm where the shot was given
- Fever
- Headache or feeling tired
- Nausea
- Muscle or joint pain
Brief fainting spells and related symptoms (such as jerking movements) can happen after any medical procedure, including vaccination. Sitting or lying down while getting a shot and then staying that way for about 15 minutes can help prevent fainting and injuries caused by falls that could occur from fainting.
On very rare occasions, severe (anaphylactic) allergic reactions may occur after vaccination. People with severe allergies to any component of a vaccine should not receive that vaccine.
HPV vaccine does not cause HPV infection or cancer. HPV vaccine is made from one protein from the virus, and is not infectious, meaning that it cannot cause HPV infection or cancer. Not receiving HPV vaccine at the recommended ages can leave one vulnerable to cancers caused by HPV.
There are no data that suggest getting HPV vaccine will have an effect on future fertility for women. In fact, getting vaccinated and protecting against HPV-related cancers can help women and families have healthy pregnancies and healthy babies.
Not getting HPV vaccine leaves people vulnerable to HPV infection and related cancers. Treatments for cancers and precancers might include surgery, chemotherapy, and/or radiation, which might cause pregnancy complications or leave someone unable to have children.
Q: Why is this vaccine not mandatory for school entry?
A: Each state determines which vaccines are required for school entry. Many factors are taken into consideration before requiring any vaccine for school entry, including: community support for the requirement, financial resources needed to implement the requirement, burden on school personnel for enforcing the requirement, vaccine supply, and current vaccination coverage levels.
Since almost every state requires Tdap (tetanus, diphtheria, and acellular pertussis vaccine) for middle school entry, parents can use this visit to the doctor to get the first HPV and quadrivalent meningococcal conjugate vaccines for their preteen at the same time.
Q: How can someone get help paying for HPV vaccine?
A: The Vaccines for Children (VFC) program helps families of eligible children who might not otherwise have access to vaccines. The program provides vaccines at no cost to children ages 18 years and younger who are uninsured, Medicaid-eligible, or American Indian/Alaska Native. To learn more, see VFC program.
Human Papillomavirus (HPV) and Cancer

Human papillomavirus (HPV) causes most cervical cancers, as well as some cancers of the vagina, vulva, penis, anus, rectum, and oropharynx (cancers of the back of the throat, including the base of the tongue and tonsils).
HPV vaccines are recommended for preteen girls and boys to protect against HPV infection. All kids who are 11 or 12 years old should get the HPV vaccine. Teens who did not get the vaccine or did not get all doses when they were younger should get it now.
Two screening tests can help prevent cervical cancer or find it early. The Pap test is recommended for women between ages 21 and 65. If you are 30 years old or older, you may choose to have an HPV test along with the Pap test.
Gynecologic Cancers

Five main types of cancer affect a woman’s reproductive organs: cervical, ovarian, uterine, vaginal, and vulvar. As a group, they are referred to as gynecologic cancers. Each gynecologic cancer is unique, with different signs, symptoms, and risk factors (things that may increase your chance of getting cancer).
All women are at risk for gynecologic cancers, and risk increases with age. You can lower your risk for some of these cancers. When gynecologic cancers are found early, treatment works best.
CDC promotes awareness of gynecologic cancers through its national awareness campaign, Inside Knowledge: Get the Facts About Gynecologic Cancer.
CDC’s National Breast and Cervical Cancer Early Detection Program provides breast and cervical cancer screenings and diagnostic services to low-income, uninsured, and underinsured women across the United States. Find out if you qualify.
Source: CDC
CONDITION: Human T-cell Lymphotropic Virus

Background
Human T-cell lymphotropic virus (HTLV) was the first human retrovirus discovered. HTLV belongs to the Retroviridae family in the genus Deltaretrovirus. Retroviruses are RNA viruses that use an enzyme called reverse transcriptase to produce DNA from RNA. The DNA is subsequently incorporated into the host’s genome. HTLV predominantly affects T lymphocytes.
Prior to 1979, the isolation of retroviruses was possible only in nonhuman primates; in fact, it was believed that human retroviruses did not exist. In 2005 in Retrovirology, Gallo reflected about earlier concepts that supported this belief. First, if human retroviruses did in fact exist, then why had they not yet been discovered? Second, the virus was easily detected in animals, and therefore should have also been easily detectable in humans. Third, technical difficulties hampered efforts to grow primary human cells in the laboratory. Finally, it was shown that the human complement lyses animal retroviruses in vitro, suggesting erroneously that humans were intrinsically protected from these viruses.
In 1979, T-cell lymphotropic virus was isolated in a patient with cutaneous T-cell lymphoma. This led to the discovery of the first HTLV and marked the beginning of the human retrovirus era. Two years later, HTLV-2 was documented in a patient who had been diagnosed with hairy cell leukemia, although subsequent studies showed no affiliation between the two processes.
In 1983, the third and most important retrovirus was discovered. At the time of its discovery, this virus was classified in the HTLV genus. However, upon further research, it was reclassified into the Lentivirus genus and given the name human immunodeficiency virus (HIV). In 2005, two novel viruses, HTLV-3 and HTLV-4, were discovered. Little is known about these viruses, as only a few cases have been reported.
Now, 30 years later after the initial discovery, 4 HTLVs are well established. HTLV-1 and HTLV-2 are both involved in actively spreading epidemics, affecting 15-20 million people worldwide. In the United States, the overall prevalence is 22 per 100,000 population, with HTLV-2 more common than HTLV-1. Data collection performed from 2000-2009 among US blood donors has shown a general decline since the 1990s.
HTLV-1 is the more clinically significant of the two, as it has been proven to be the etiologic agent of multiple disorders. At least 500,000 of the individuals infected with HTLV-1 eventually develop an often rapidly fatal leukemia, while others will develop a debilitative myelopathy, and yet others will experience uveitis, infectious dermatitis, or another inflammatory disorder. HTLV-2 is associated with milder neurologic disorders and chronic pulmonary infections. The novel HTLV-3 and HTLV-4 have been isolated only in a few cases; no specific illnesses have yet been associated with these viruses.
Pathophysiology
HTLVs are intracellular proviruses that pass through formation of a "virological synapse", allowing the viral genome to be passed from one cell to another. Once infection has occurred, little replication takes place. Infection affects the expression of T-lymphocyte gene expression, leading to increased proliferation of affected T lymphocytes. HTLV primarily affects T lymphocytes: specifically, HTLV-1 predominantly affects CD4 lymphocytes, while HTLV-2 predominantly affects CD8 lymphocytes. In vitro, HTLV-1 is also capable of infecting other cell types, possibly accounting for the diverse pathogenesis of HTLV-1. Recently, GLUT-1, a ubiquitous glucose transporter, has been identified as a receptor for HTLV-1; this may explain its ability to infect various cell types.
Acute HTLV infection is rarely seen or diagnosed, as most infections are latent and asymptomatic. Infection might be diagnosed after an attempted blood donation or through workup of a disease caused by the virus. For example, HTLV-1 is associated primarily with two diseases, adult T-cell leukemia (ATL) and HTLV-1–associated myelopathy/tropical spastic paraparesis (HAM/TSP).
HTLV-1 and HTLV-2 have similar transmission patterns, although the transmission efficiency of HTLV-2 is uncertain because of a lack of unbiased data gathering. Both can be transmitted via breast milk, sexual contact, and intravenous drug use, and both can be introduced directly into the vascular system. HTLV-3 and HTLV-4 seem to be transmitted through direct human contact with primates (eg, through hunting, butchering, keeping them as pets), but data are lacking.
On the molecular level, as with all retroviruses, HTLV has a gag-pol-env motif with flanking long terminal repeat sequences. Unique to the Deltraviruses, however, it includes a fourth sequence named Px, which participates in open-reading–frame transcription, in turn encoding for regulatory proteins Tax, Rex, p12, p13, and p30. All these proteins are important for the infectivity of cells, as well as in stimulating replication. In ATL, the main pathogenic protein, Tax, leads to leukogenesis and immortalization of T lymphocytes in vitro. This is achieved by stimulation of interleukin-15 (IL-15) and interleukin-2 (IL-2), in turn leading to T-cell growth and transformation. Research on this subject is ongoing, and the expression of this gene is not always found in ATL cells. Furthermore, Tax is inherent to both HTLV-1 and HTLV-2, although HTLV-1 is more pathogenic.
Recently, the HTLV-1 basic zipper factor gene (HBZ) has been found to be consistently expressed in ATL cells, suggesting a role in cellular transformation and leukemogenesis. This might correlate with the increased pathogenesis of HTLV-1. The expression of the HBZ gene also correlates with the provirus load of HTLV-1.
Epidemiology
Because of the low replicating nature of HTLV, the virus develops little genetic sequence variation. Therefore, most epidemiologic data are based on serologic studies rather than on molecular typing. Variations exist in the env gene for each HTLV; they define the HTLV subtypes. The distribution of HTLV-1 and HTLV-2 subtypes is quite distinct and can probably be explained by differing evolutionary trends. HTLV-1 subtypes are associated with specific regions of the globe, while HTLV-2 subtypes are related to highly specific subpopulations (eg, Brazilian Indians) and behaviors such as injection drug use.
Transmission of HTLV-1 and HTLV-2
See the list below:
- Breastfeeding
- HTLV-infected T cells in breast milk pass from mother to child. The risk of HTLV-1 transmission reaches 20% and is affected by the duration of breastfeeding, the proviral load, and the quantity of maternal antibodies. Intrauterine infection is less common, about 5%.
- For HTLV-2, the quantitative risk remains uncertain for both breastfeeding and intrauterine transmission.
- Sexual: Increased exposure and increased proviral load increase the risk of sexual transmission of both HTLV-1 and HTLV-2.
- Transfusion: The risk of seroconversion due to contaminated blood transfusion has been reported to be 40%-60% and increases in immunosuppressed recipients.
- Transplant: Reports have documented kidney, liver, and lung transplant transmission of HTLV-1.
- Intravenous drug use: This mode of transmission is mostly linked to HTLV-2. The prevalence of HTLV-2 infection in North American injection drug users ranges from 8%-17%.
HTLV-1
Six different HTLV-1 subclasses exist, and each subtype is endemic to a particular region. HTLV-1 clustering occurs, as evidenced by a high prevalence in southwestern Japan despite a low prevalence in neighboring regions (eg, Korea, China, eastern Russia), although the cause of this is unknown.
- Subtype A (cosmopolitan subtype) - Japan
- Subtypes B, D, and F - Central Africa
- Subtype C - Melanesia
- Subtype E - South and Central Africa
HTLV-1 is associated with the below diseases. Note that ATL and HAM/TSP are generally mutually exclusive, and only a few cases with both disorders have been described.
- ATL develops in 2%-4% of individuals with HTLV-1 infection. Four clinical subtypes of ATL have been described.
- The acute form comprises 55%-75% of all ATL cases. It is characterized by a significantly increased white blood cell count that is mostly made up of leukemic T cells. It also features generalized lymphadenopathy.
- The chronic form is characterized by absolute lymphocytosis (4 × 109/L or more), with T lymphocytosis comprising more than 3.5 × 109/L. These laboratory findings persist for months to years in most patients with chronic ATL. The lymphatic system may become involved.
- Smoldering ATL is characterized by 5% or more abnormal T lymphocytes in peripheral blood, with a normal total lymphocyte count.
- The lymphoma type involves generalized lymphadenopathy and an absence of peripheral blood involvement.
- HAM/TSP develops in 1%-2% of individuals with HTLV-1 infection.
- The pathophysiology of HAM/TSP remains unclear, but, clinically, it can be defined as a slowly progressive degenerative disease that primarily affects the corticospinal tracts of the thoracic cord.
- Major pathologic findings of HAM/TSP may include inflammatory perivascular and parenchymal infiltration by T-lymphocyte cells, leading to degeneration and fibrosis in the spinal cord. The degree of infiltration is less than in other retroviral infections (eg, HIV infection), perhaps because of the slow pathogenesis of the virus.
- Immunologic mechanisms may be involved in the development of HAM/TSP. This is likely mediated through autoimmune processes or cytotoxic attack on the HTLV-1–infected cells.
- A higher provirus load increases not only the overall risk of HAM/TSP but also the likelihood that the disease will progress more quickly.
- HTLV-1 is also associated with a broader spectrum of neurologic abnormalities that are not as severe as HAM/TSP. It is not clearly established if individuals with the other neurologic abnormalities will eventually develop HAM/TSP or will remain stable.
- HTLV-1–associated uveitis/ocular manifestations
- This is defined as the presence of HTLV viral sequences and HTLV-infected lymphocytes in the vitreous fluid.
- Additional ocular manifestations in individuals with HTLV-1 infection include retinal vasculitis, choroidopathy, and keratopathy.
- In 2013, a case report described unilateral intraocular invasion of ATL cells without systemic symptoms following cataract surgery. Antibodies to HTLV-1 were positive, and the vitreous specimen revealed flower cell infiltration with HTLV-1 DNA detected via polymerase chain reaction (PCR).
- HTLV-1–associated infective dermatitis
- HTLV-1–associated infective dermatitis (IDH) is a chronic and severe dermatitis that mainly affects children who have been infected with HTLV via vertical transmission.
- There is an association between IDH and onset of HAM/TSP; 30% of Brazilian children with IDH develop HAM/TSP in adolescence.
- Patients with IDH have a higher proviral load than asymptomatic carriers of HTLV-1. Primo et al (2009) reported that the proviral load was not associated with age, duration of infection, duration of breastfeeding, or severity of skin infection.
- Additional cutaneous diseases, which are found more frequently in HTLV-1 carriers than in noncarriers, include aphthous stomatitis, eczema, and nongenital warts.
- Other diseases associated with HTLV-1 include Sjögren syndrome, polymyositis, and chronic inflammatory arthropathy.
- HTLV-1–associated oral manifestations
- In addition to Sjögren syndrome, other oral manifestations are becoming apparent. A study of Brazilians with HTLV-1 infection showed the most common manifestations were xerostomia (26.8%), candidiasis (20.8%), fissured tongue (17.9%), and loss of tongue papillae (17.9%). Patients with HAM/TSP were 3 times more likely to have xerostomia than patients without HAM/TSP. Similar results were described by Lins et al.
- Garlet et al suggested an association between periodontitis and HTLV-1 in which HTLV plays a direct role in deregulation of cytokines, resulting in an exaggerated immune response against the bacteria causing periodontitis.
HTLV-2
HTLV-2 is classified into 4 molecular subtypes. Each has a characteristic geographic association.
- Subtypes A and B - Present throughout Western Hemisphere and Europe; sporadic distribution in Asia and Africa
- Subtype C - Kayapo indigenous people of the Amazon and urban Brazilian populations
- Subtype D - Discovered in an African pygmy tribe
To date, no conclusive evidence has proven that HTLV-2 is an etiologic agent in any specific disease. However, the following links have been suggested:
- HTLV-2 infection may result in neurologic manifestations similar to the non-HAM complications of HTLV-1 infection. Recent data suggest that HTLV-1 and HTLV-2 carry similar risks in terms of resulting in non-HAM neurological illness.
- Case reports have linked HTLV-2 infection with pneumonia, bronchitis, arthritis, asthma, and dermatitis.
HTLV-3 and HTLV-4
These HTLV subtypes were first isolated in 2005. HTLV-3 was initially isolated from a 62-year-old male pygmy in southern Cameroon. Now, with the aid of advancing laboratory technology, new strains are quickly being identified. Individuals infected with HTLV-3 have all been asymptomatic, with a low proviral load. HTLV-4 has been described in African bush meat hunters. In 2010, no evidence of HTLV-3 and HTLV-4 infection was found in a sample of 1200 New York State subjects (human and simian subject types) at risk for retroviral infection.
Neither HTLV-3 nor HTLV-4 has been associated with specific diseases thus far, and further research is ongoing. Given the ongoing discovery of subtypes and strains, it is not surprising that 28% of certain populations in central Africa have been reported to have indeterminate HTLV serology results.
The HTLV-3 label was initially applied to the virus that causes AIDS. However, further research found that the pathogenesis and genetic makeup of the AIDS virus differed from HTLV-1 and HTLV-2. Subsequently, the name was formally changed to HIV.
Epidemiology & Frequency
United States
HTLV-1
HTLV-1 infection is linked to immigrants, children of immigrants, sex workers, and injection drug users.
Based on transfusion data from 2000-2009 among first-time donors, the prevalence of HTLV-1 was 5.1 cases per 100,000 population and was associated with female sex, older age, and black and Asian race/ethnicity.
HTLV-2
Based on transfusion data from 2000-2009 among first-time donors, the prevalence of HTLV-2 was 14.7 cases per 100,000 population and was associated with female sex, older age, nonwhite race/ethnicity, lower educational level, and residence in the western and southwestern United States.
In the United States, HTLV-2 infection affects Native American Indians. Some tribes have seroprevalence rates as high as 13%.
Intravenous drug users, in whom the seroprevalence is estimated to be about 20%, with a disproportionate share occurring in African American injection drug users.
International
Areas and small population clusters with high concentrations of HTLV-1 include the following:
- Southwest Japan: Japan has both low and high endemic microregions, with an estimated total 1.2 million HTLV-1 carriers.
- Caribbean basin (Jamaica and Trinidad): This region has a prevalence of up to 6%.
- Sub-Saharan African countries (Benin, Cameroon, Guinea-Bissau): These countries have a prevalence of up to 5%.
- South America
- The Mashadi Jewish people of northern Iran and various immigrant populations from endemic areas
Areas and populations with high concentrations of HTLV-2 include the following:
- Central and South America
- North America and Europe, mainly among intravenous drug users
Mortality/Morbidity
Mortality and morbidity due to HTLV infections are primarily associated with diseases caused by HTLV-1, namely ATL or HAM/TSP.
Infected individuals have a cumulative lifetime risk of 1%-4% of developing ATL or HAM/TSP. The latency period for ATL is typically 30-50 years. ATL is usually rapidly progressive and fatal, with a median survival time of 2 years.
HAM/TSP can occur as early as 3 months after blood transfusion–related HTLV-1 infection. Three years of latency is more typical, and 20-30 years is possible.
Biswas et al (2009) found that patients infected with HTLV - 2 missed more work days than patients with HTLV-1, possibly because of isolated neurological manifestations and the increased rate of upper respiratory infections and arthritis associated with HTLV-2.
Sex
In endemic areas, HTLV-1 seropositivity is clustered in families, especially among women, suggesting that transmission occurs more easily from men to women than from women to children. Determining the sexual predominance of HTLV-2 infection is complicated by intravenous drug use in the study population.
Findings suggest that vertical transmission has a male predisposition, accounting for the predominance of male HTLV-1 seropositivity in childhood. This, in turn, may explain the increased prevalence of ATL in males because of a longer carrier state.
HAM/TSP disproportionately affects females (with a female-to-male ratio as high as 2:1).
Age
The prevalence of HTLV-1 and HTLV-2 infections increases with advancing age. The onset of ATL or HAM/TSP is often delayed until later in life because of the prolonged latency state; vertical transmission is associated with an elevated risk of ATL or HAM/TSP.
Source: Emedicine
CONDITION: Lymphogranuloma Venereum (LGV)

What is lymphogranuloma venereum (LGV)?

Lymphogranuloma Venereum (caused by 3 subtypes of Chlamydia trachomatis, a bacteria)
NOTE: LGV is rare in the U.S. If you have signs or symptoms of any sexually transmitted disease you should see a health care provider for evaluation and possible treatment. Suspect cases of LGV should be coordinated by the MDH Public Health Laboratory to facilitate submission of diagnostic specimens. Please contact (651) 201-5257 for further information.
Lymphogranuloma venereum (LGV) is a sexually transmitted disease (STD) caused by a type of chlamydia trachomatis (serovars L1, L2, or L3) that rarely occurs in the United States and other industrialized countries. However, recent outbreaks of LGV have been reported among men who have sex with men (MSM) in Europe and other U.S. cities. If you have signs or symptoms of any sexually transmitted disease you should see a health care provider for evaluation and possible treatment.

Signs and Symptoms
Early stage LGV symptoms:
- Begin 3–12 days or longer after exposure
- Early symptoms often go unnoticed or never occur
- Soft red, painless sore or lesion that forms on or near the genitals or anus
- Sores can also occur in the throat or mouth from oral sex
- The sore heals rapidly in a few days
Later stage LGV symptoms:
- Begin 2–6 weeks or longer after primary lesion
- Swollen lymph glands on one or both sides of the groin
- Pain during urination or when passing stools
- Constipation
- Rectal bleeding
- Pain in lower abdomen or back
- Pus-filled or bloody diarrhea
- Fever, chills, joint pain, decreased appetite and tiredness

Transmission
LGV is spread by:
- Vaginal sex
- Oral sex
- Anal sex


Complications
If left untreated, LGV can:
- Spread to sex partners.
- Cause severe scarring and deformed genitals.
- Cause scarring of rectum causing narrowing.
- In women, create an opening between the vagina and anus (fistula).
- Cause brain inflammation (very rare).


Prevention
- Avoiding vaginal, oral or anal sex is the best way to prevent STDs.
- Latex condoms, when used consistently and correctly, can reduce the risk of transmission of LGV.
- Always use latex condoms during vaginal and anal sex.
- Use a latex condom for oral sex on a penis.
- Use a latex barrier (dental dam or condom cut in half) for oral sex on a vagina or anus.
- Limit the number of sex partners.
- Notify sex partners immediately if infected.
- Make sure partners are tested and treated.
Testing and Treatment
- Get a test from a medical provider if infection is suspected.
- LGV can be cured using medication prescribed by medical provider.
- Partners should be treated at same time.
NOTE: A person can be re-infected after treatment.
For More Information, Contact:
For more information, contact:
STD, HIV and TB Section
Minnesota Department of Health
(651) 201-5414
Minnesota Family Planning and STD Hotline
1-800-783-2287 Voice/TTY; (651) 645-9360 (Metro)
American Social Health Association (ASHA)
CDC National STD and AIDS Hotlines
1-800-CDC-INFO; 1-888-232-6348 TTY
1-800-344-7432 (Spanish)
Content Notice: This site contains HIV or STD prevention messages that may not be appropriate for all audiences. Since HIV and other STDs are spread primarily through sexual practices or by sharing needles, prevention messages and programs may address these topics. If you are not seeking such information or may be offended by such materials, please exit this web site.
About Lymphogranuloma Venereum (LGV)
LGV is a sexually transmitted disease (STD) or infection involving the lymph glands in the genital area. It is caused by a specific strain of Chlamydia.
Who gets LGV?
The incidence is highest among sexually active people living in tropical or subtropical climates. It has also occurred in some areas of the southern United States.
How is LGV spread?
The infection is spread by sexual contact.
What are the symptoms of LGV?
The first symptom may be a small, painless pimple or lesion occurring on the penis or vagina. It is often unnoticed. The infection then spreads to the lymph nodes in the groin area and from there to the surrounding tissue. Complications may include inflamed and swollen lymph glands which may drain and bleed.
How soon do symptoms appear?
The onset of symptoms varies widely. The initial lesion may appear from three to 30 days after exposure.
When and for how long is a person able to spread LGV?
An individual remains infectious as long as there are active lesions.
What is the treatment for LGV?
Treatment involves the use of certain antibiotics, specifically tetracycline or sulfamethoxazole.
What can be done to prevent the spread of LGV?
There are a number of ways to prevent the spread of LGV:
- Limit your number of sex partners.
- Use a male or female condom.
- Carefully wash genitals after sexual relations.
- If you think you are infected, avoid any sexual contact and visit your local STD clinic, a hospital or your doctor.
- Notify all sexual contacts immediately so they can obtain examination and treatment.
NYS Health Dept.
CONDITION: Molluscum contagiosum (Water Warts)
A viral skin infection that results in round, firm, painless bumps.
Mycoplasma genitalium infection - including symptoms, treatment and prevention
This is an infection caused by Mycoplasma genitalium bacteria.
How Mycoplasma genitalium infection is spread
Mycoplasma genitalium (M. genitalium) is transmitted sexually.


Signs and symptoms
Men
In men M. genitalium infection causes urethritis (infection of the urethra, the urinary canal leading from the bladder to exit at the tip of the penis). Symptoms may include:
- watery discharge from the penis
- burning sensation in the penis when urinating.
Women
In women M. genitalium infection causes infection of the cervix (opening of the uterus (womb) at the top of the vagina). Symptoms are usually absent but may include:
- abnormal discharge from the vagina
- discomfort on urination
- bleeding between periods, often after sex.

Without adequate treatment, infection of the cervix may spread to the Fallopian tubes (tubes leading from the ovary to the uterus) and cause pelvic inflammatory disease (PID). This may be without symptoms, but there may be:
- fever
- low abdominal pain
- pain on intercourse.
If untreated, PID may lead to scarring of the Fallopian tubes and ectopic or tubal pregnancy (in the Fallopian tubes) or eventual infertility.
Diagnosis
PCR (polymerase chain reaction) test in a pathology laboratory on urine or a sample of discharge from the cervix or urethra. However, a PCR test for M. genitalium is not readily available and many infections in men will be labelled as non-specific urethritis.
The diagnosis is usually made when symptoms are present and tests for gonorrhoea and chlamydia are negative and further testing for M. genitalium is undertaken.
Incubation period
(time between becoming infected and developing symptoms)
Variable, usually 2 to 35 days.
Infectious period
(time during which an infected person can infect others)
Until appropriate antibiotic treatment has been completed.
Treatment
Effective antibiotic treatment is available on prescription from a doctor.
Continued or recurring symptoms may require referral for specialist treatment.

Prevention
- No sex until antibiotic treatment is completed and your usual sexual partner has completed treatment.
- A follow-up test must be done to make sure that treatment has cleared the infection.
- All sexual partners need to be contacted, tested and, if indicated, treated. Even if partners have no symptoms they may be able to transmit infection to other sexual partners.
- Testing to exclude other sexually transmitted infections is advisable.
Source: SAHealth.Ca.Gov
CONDITION: Mycoplasma genitalium

Mycoplasma genitalium
M. genitalium was first identified in the early 1980s and has become recognized as a cause of male urethritis, responsible for approximately 15%–20% of nongonococcal urethritis (NGU) cases, 20%–25% of nonchlamydial NGU, and approximately 30% of persistent or recurrent urethritis. In most settings, it is more common than N. gonorrhoeae but less common than C. trachomatis. While M. genitalium is often the sole pathogen detected, coinfection with C. trachomatis is not uncommon in selected areas.
Although strong and consistent evidence has linked M. genitalium to urethritis in men, it remains unknown whether this infection can cause male infertility or other male anogenital tract disease syndromes. The organism has been detected in men with epididymitis in a limited number of cases, but this has not been extensively investigated. Similarly, M. genitalium has been found in the rectum, but detection is infrequently accompanied by rectal symptoms, and its presence does not appear to cause a syndrome of clinical proctitis.
The pathogenic role of M. genitalium is less definitive in women than it is in men. M. genitalium can be found in the vagina, cervix, and endometrium and, like chlamydial and gonococcal infections, M. genitalium infections in women are commonly asymptomatic. M. genitalium can be detected in 10%–30% of women with clinical cervicitis, and most studies have found that this organism is more common among women with cervicitis than those without this syndrome
M. genitalium is found in the cervix and/or endometrium of women with PID more often than in women without PID, and endosalpingitis develops in nonhuman primates after inoculation with M. genitalium, suggesting that this organism can cause PID. M. genitalium has been detected in 2%–22% of PID cases (median: 10%) depending on the setting, but the frequency with which M. genitalium-infected women experience PID has been under studied. Although one study in Sweden reported a substantial increase in risk for postabortal PID among women with M. genitalium, the proportion of M. genitalium-positive women who subsequently experienced PID in two other studies was relatively low (<5%), and evidence from serologic studies assessing the association of PID with antibody to M. genitalium is inconsistent. Overall, evidence suggests that M. genitalium can cause PID, but that this occurs less frequently than it does with C. trachomatis).
A few seroepidemologic studies have found that women with tubal factor infertility are more likely to have antibodies to M. genitalium than fertile women, suggesting that this organism might cause female infertility. However, more research is needed. On the basis of certain reports, M. genitalium was uncommonly identified in women who experience adverse pregnancy outcomes, but was associated with increased risk for preterm delivery in one U.S. and another Peruvian study. Data are scarce regarding M. genitalium and ectopic pregnancy.

Diagnostic Considerations
M. genitalium is a slow-growing organism. Culture can take up to 6 months, and only a few laboratories in the world are able to recover clinical isolates. Therefore, NAAT is the preferred method for M. genitalium detection. In research settings, M. genitalium is diagnosed by NAAT testing of urine, urethral, vaginal, and cervical swabs and through endometrial biopsies, typically using in-house PCR or assays intended for research use only. NAAT tests (polymerase chain reaction or transcription mediated amplification) for M. genitalium are available in some large medical centers and commercial laboratories, but there is no diagnostic test for M. genitalium that is cleared by the FDA for use in the United States. In the absence of validated tests, M. genitalium should be suspected in cases of persistent or recurrent urethritis and may be considered in persistent or recurrent cases of cervicitis and PID.

Treatment
M. genitalium lacks a cell wall, and thus antibiotics targeting cell-wall biosynthesis (e.g., beta-lactams including penicillins and cephalosporins) are ineffective against this organism. Given the diagnostic challenges, treatment of most M. genitalium infections will occur in the context of syndromic management for urethritis, cervicitis, and PID.
Urethritis and cervicitis
The 7-day doxycycline regimen recommended for treatment of urethritis is largely ineffective against M. genitalium with a median cure rate of approximately 31%. The 1-g single dose of azithromycin was significantly more effective against M. genitalium than doxycycline in two randomized urethritis treatment trials and is preferred over doxycycline. However, resistance to azithromycin appears to be rapidly emerging. The median cure rate for both men and women is approximately 85%, but was only 40% in the most recent trial. Persons with treatment failures after the 1-g azithromycin regimen frequently have macrolide-resistant strains, suggesting that single-dose azithromycin therapy might select for resistance. A longer course of azithromycin (an initial 500-mg dose followed by 250 mg daily for 4 days) might be marginally superior to the single dose regimen. However, in some settings, approximately 50% of all M. genitalium infections are caused by organisms that are already resistant to azithromycin (282), and persons who do not respond to the 1-g azithromycin regimen generally do not benefit from retreatment with the extended dose regimen.
Moxifloxacin (400 mg daily x 7, 10 or 14 days) has been successfully used to treat M. genitalium in men and women with previous treatment failures, with cure rates of 100% in initial report. However, moxifloxacin has been used in only a few cases, and the drug has not been tested in clinical trials. Although generally considered effective, studies in Japan, Australia, and the United States have reported moxifloxacin treatment failures after the 7 day regimen.
Source: Centers for Disease Control and Prevention
Nongonococcal Urethritis (NSU, NGU)

What is nongonococcal urethritis (NGU)?
NGU refers to an infection of the urethra (the tube running from the bladder through the penis in men or the labia in women through which urine passes) caused by some agent other than gonorrhea. This infection can be caused by any of several different organisms, although the most frequent cause of NGU is a germ called Chlamydia, and is a sexually transmitted disease (STD).
Who gets NGU?
NGU is most often found in men since the organisms causing this infection are sexually transmitted and the female urethra is seldom infected during intercourse. Men between the ages of 15 and 30 having multiple sex partners are most at risk for this infection.
How is NGU spread?
NGU is spread almost exclusively through sexual contact involving penis to vagina or penis to rectum contact.
What are the symptoms of NGU?
The symptoms of NGU involve a slight burning or tingling during urination that is sometimes accompanied by a slight (usually clear) discharge (drip) from the urethra.
How soon do symptoms appear?
The symptoms associated with NGU usually appear from one to five weeks after infection. Some people never develop obvious symptoms throughout their infection.
When and for how long is a person able to spread NGU?
A person can spread NGU from the time they are infected until they are cured.
Does past infection with NGU make a person immune?
No. Past infection with NGU does not protect a person from contracting the disease again.
What is the treatment for NGU?
NGU is treated through the use of antibiotics such as tetracycline.
What can be the effect of not being treated for NGU?
If not treated for NGU, a person may experience swelling of the testicles (epididymitis) and infection of the prostate gland. More importantly, they may infect sexual partners.
What can be done to prevent the spread of NGU?
There are a number of ways to prevent the spread of NGU:
-
Limit your number of sex partners.
-
Use a condom.
-
Carefully wash genitals after sexual relations.
-
If you think you are infected, avoid any sexual contact and visit your local STD clinic, a hospital or your doctor.
-
Notify all sexual contacts immediately so they can obtain examination and treatment.
Last Reviewed: November 2006
Source: NY Departmetnof Health
CONDITION: Mucopurulent Cervicitis (MPC)
What is MPC?
MPC is a sexually transmitted infection (STI) of the cervix. It can be caused by chlamydia and/or gonorrhea or other germs (bacteria or viruses) that aren’t known. Some of the germs that cause MPC can be in your body for a long time before you have symptoms.
How do I get MPC?
Females get MPC through unprotected sexual contact (oral, vaginal, or anal) with a partner infected with germs that can cause MPC. You can infect others right after you come in contact with the germs that cause MPC. You can pass on the germs to others without knowing it.

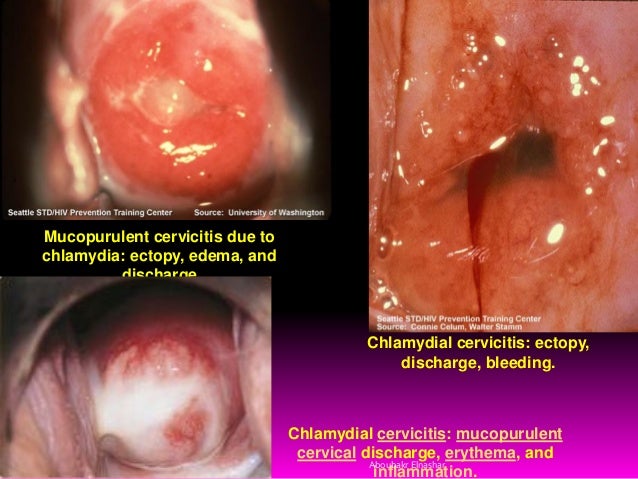
How do I prevent MPC?
When you are sexually active, the best way to prevent MPC is to use condoms for oral, vaginal, and anal sex. Don’t have any sexual contact if you or your partner(s) have symptoms or may have been exposed to an STI. See a doctor or go to an STI Clinic for testing. Get STI testing regularly every 3 to 6 months and when you have symptoms.
How do I know I have MPC?
Some females with MPC don’t have any symptoms, while others may have:
- vaginal discharge
- bleeding between periods or after sex
- pain in the abdomen
- pain during or after vaginal sex
The best way to find out if you have MPC is to see your nurse or doctor and get tested. You will have a pelvic exam and be tested for STIs.
Is MPC harmful?
If MPC isn’t treated, it can spread up into the uterus, fallopian tubes, and ovaries. This can cause a serious infection called pelvic inflammatory disease (PID). PID can cause pain in the lower abdomen, infertility, and increase your risk of tubal pregnancies. These effects can be prevented if you get early STI testing and treatment.
How is MPC treated?
MPC is treated with antibiotics. Your partner(s) also needs to be tested and treated, even if there are no symptoms. You can get re-infected if you have unprotected sex (oral, vaginal, or anal without a condom) before your partner(s) is treated. If you still have symptoms 3 to 4 weeks after taking antibiotics, see your nurse or doctor.
When can I have sex again?
It will take 1 week for the antibiotic to get rid of the infection. Don’t have unprotected sex (oral, vaginal, anal without a condom) for 7 days after you and your partner(s) have completed treatment. The best protection is not to have sex (oral, vaginal, anal) for at least 7 days. If you still have symptoms, don’t have any sexual contact.
For more information on Sexually Transmitted Infections (STI’s) see:
Current as of: June 29, 2016
Author: Sexual and Reproductive Health, Alberta Health Services
CONDITION: Nongonococcal Urethritis (NSU, NGU)
What is nongonococcal urethritis (NGU)?
NGU refers to an infection of the urethra (the tube running from the bladder through the penis in men or the labia in women through which urine passes) caused by some agent other than gonorrhea. This infection can be caused by any of several different organisms, although the most frequent cause of NGU is a germ called Chlamydia, and is a sexually transmitted disease (STD).
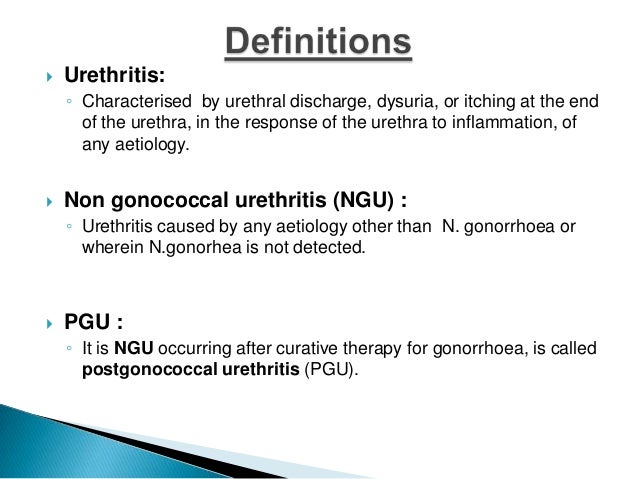


Who gets NGU?
NGU is most often found in men since the organisms causing this infection are sexually transmitted and the female urethra is seldom infected during intercourse. Men between the ages of 15 and 30 having multiple sex partners are most at risk for this infection.
How is NGU spread?
NGU is spread almost exclusively through sexual contact involving penis to vagina or penis to rectum contact.
What are the symptoms of NGU?
The symptoms of NGU involve a slight burning or tingling during urination that is sometimes accompanied by a slight (usually clear) discharge (drip) from the urethra.
How soon do symptoms appear?
The symptoms associated with NGU usually appear from one to five weeks after infection. Some people never develop obvious symptoms throughout their infection.
When and for how long is a person able to spread NGU?
A person can spread NGU from the time they are infected until they are cured.
Does past infection with NGU make a person immune?
No. Past infection with NGU does not protect a person from contracting the disease again.
What is the treatment for NGU?
NGU is treated through the use of antibiotics such as tetracycline.
What can be the effect of not being treated for NGU?
If not treated for NGU, a person may experience swelling of the testicles (epididymitis) and infection of the prostate gland. More importantly, they may infect sexual partners.
What can be done to prevent the spread of NGU?
There are a number of ways to prevent the spread of NGU:
- Limit your number of sex partners.
- Use a condom.
- Carefully wash genitals after sexual relations.
- If you think you are infected, avoid any sexual contact and visit your local STD clinic, a hospital or your doctor.
- Notify all sexual contacts immediately so they can obtain examination and treatment.
NYS Health Dept.
CONDITION:HPV, Genital warts, and Cancers

HPV is short for human papillomavirus.
HPV is a group of more than 150 related viruses. Each HPV virus in this large group is given a number which is called its HPV type. HPV is named for the warts (papillomas) some HPV types can cause. Some other HPV types can lead to cancer. Men and women can get cancer of mouth/ throat, and anus/rectum caused by HPV infections. Men can also get penile HPV cancer. In women, HPV infection can also cause cervical, vaginal, and vulvar HPV cancers. But there are vaccines that can prevent infection with the types of HPV that most commonly cause cancer.
How do people get HPV?
HPV is transmitted through intimate skin-to-skin contact. You can get HPV by having vaginal, anal, or oral sex with someone who has the virus. It is most commonly spread during vaginal or anal sex. HPV is so common that nearly all men and women get it at some point in their lives. HPV can be passed even when an infected person has no signs or symptoms. You can develop symptoms years after being infected, making it hard to know when you first became infected.
In most cases, HPV goes away on its own and does not cause any health problems. But when HPV does not go away, it can cause health problems like genital warts and cancer.
Genital warts usually appear as a small bump or groups of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower. A healthcare provider can usually diagnose warts by looking at the genital area.
HPV cancers include cancer of the cervix, vulva, vagina, penis, or anus. HPV infection can also cause cancer in the back of the throat, including the base of the tongue and tonsils.
More Q&A about the Health Effects of HPV
On this Page
- How common are HPV infections?
- What kinds of problems does HPV infection cause?
- How do people get an HPV infection?
- Who should get HPV vaccine?
- Why are two doses recommended for 9–14 year olds, while older adolescents need three doses?
- Why is HPV vaccine recommended at age 11 or 12 years?
- How well does HPV vaccine work?
- Does HPV vaccination offer similar protection from cervical cancer in all racial/ethnic groups?
- How do we know that the HPV vaccine is safe?
- What are the possible side effects of HPV vaccination?
- Why is this vaccine not mandatory for school entry?
- How can someone get help paying for HPV vaccine?
Q: How common are HPV infections?
A: HPV infections are so common that nearly all men and women will get at least one type of HPV at some point in their lives. Most people never know that they have been infected and may give HPV to a sex partner without knowing it. About 79 million Americans are currently infected with some type of HPV. About 14 million people in the United States become newly infected each year.
Q: What kinds of problems does HPV infection cause?
A: Most people with HPV never develop symptoms or health problems. Most HPV infections (9 out of 10) go away by themselves within two years. But, sometimes, HPV infections will last longer, and can cause certain cancers and other diseases. HPV infections can cause:
- cancers of the cervix, vagina, and vulva in women;
- cancers of the penis in men; and
- cancers of the anus and back of the throat, including the base of the tongue and tonsils (oropharynx), in both women and men. Every year in the United States, HPV causes 30,700 cancers in men and women.
Q: How do people get an HPV infection?
A: People get HPV from another person during intimate sexual contact. Most of the time, people get HPV from having vaginal and/or anal sex. Men and women can also get HPV from having oral sex or other sex play. A person can get HPV even if their partner doesn’t have any signs or symptoms of HPV infection. A person can have HPV even if years have passed since he or she had sexual contact with an infected person. Most people do not realize they are infected. They also don’t know that they may be passing HPV to their sex partner(s). It is possible for someone to get more than one type of HPV.
It's not very common, but sometimes a pregnant woman with HPV can pass it to her baby during delivery. The child might develop recurrent respiratory papillomatosis (RRP), a rare but dangerous condition where warts caused by HPV (similar to genital warts) grow inside the throat.
There haven’t been any documented cases of people getting HPV from surfaces in the environment, such as toilet seats. However, someone could be exposed to HPV from objects (toys) shared during sexual activity if the object has been used by an infected person.
Q: Who should get HPV vaccine?
A: All girls and boys who are 11 or 12 years old should get the recommended series of HPV vaccine. The vaccination series can be started at age 9 years. Teen boys and girls who did not get vaccinated when they were younger should get it now. HPV vaccine is recommended for young women through age 26, and young men through age 21. HPV vaccine is also recommended for the following people, if they did not get vaccinated when they were younger:
- young men who have sex with men, including young men who identify as gay or bisexual or who intend to have sex with men through age 26;
- young adults who are transgender through age 26; and
- young adults with certain immunocompromising conditions (including HIV) through age 26.
Q: Why are two doses recommended for 9–14 year olds, while older adolescents need three doses?
A: Since 2006, HPV vaccines have been recommended in a three-dose series given over six months. In 2016, CDC changed the recommendation to two doses for persons starting the series before their 15th birthday. The second dose of HPV vaccine should be given six to twelve months after the first dose. Adolescents who receive their two doses less than five months apart will require a third dose of HPV vaccine.
Teens and young adults who start the series at ages 15 through 26 years still need three doses of HPV vaccine Also, three doses are still recommended for people with certain immunocompromising conditions aged 9 through 26 years.
CDC makes recommendations based on the best available scientific evidence. Studies have shown that two doses of HPV vaccine given at least six months apart to adolescents at age 9–14 years worked as well or better than three doses given to older adolescents and young adults. Studies have not been done to show this for adolescents starting the series at age 15 years or older.
Q: Why is HPV vaccine recommended at age 11 or 12 years?
A: For HPV vaccine to be most effective, the series should be given prior to exposure to HPV. There is no reason to wait to vaccinate until teens reach puberty or start having sex. Preteens should receive all recommended doses of the HPV vaccine series long before they begin any type of sexual activity.
Q: How well does HPV vaccine work?
A: HPV vaccines work extremely well. Clinical trials showed HPV vaccines provide close to 100% protection against cervical precancers and genital warts. Since the first HPV vaccine was recommended in 2006, there has been a 64% reduction in vaccine-type HPV infections among teen girls in the United States. Studies have shown that fewer teens are getting genital warts and cervical precancers are decreasing. In other countries, such as Australia, where HPV vaccination coverage is higher than in the United States, large decreases have been observed in these HPV-associated outcomes. HPV vaccines offer long-lasting protection against HPV infection and HPV disease. There has been no evidence to suggest that HPV vaccine loses any ability to provide protection over time. Data are available for about 10 years of follow-up after vaccination.
Like all vaccines, HPV vaccine is monitored on an ongoing basis to make sure it remains safe and effective. If it turns out that protection from HPV vaccine is not long-lasting, then the Advisory Committee on Immunization Practices would review the data and determine whether a booster dose would be recommended.
Even if it has been months or years since the last shot, the HPV vaccine series should be completed—but they do not need to restart the series.
HPV vaccine is recommended based on age, not sexual experience. Even if someone has already had sex, they should still get HPV vaccine. Even though a person’s first HPV infection usually happens during one of the first few sexual experiences, a person might not be exposed to all of the HPV types that are covered by HPV vaccines.
Q: Does HPV vaccination offer similar protection from cervical cancer in all racial/ethnic groups?
A: Yes. Several different HPV types cause cervical cancer. HPV vaccines are designed to prevent the HPV types that cause most cervical cancers, so HPV vaccination will provide high protection for all racial/ethnic groups.
All three licensed HPV vaccines protect against types 16 and 18, which cause the majority of cervical cancers across racial/ethnic groups (67% of the cervical cancers among whites, 68% among blacks, and 64% among Hispanics). The 9-valent HPV vaccine protects against seven HPV types that cause about 80% of cervical cancer among all racial/ethnic groups in the United States.
Teens and young adults who haven’t completed the HPV vaccine series should make an appointment today to get vaccinated. To protect against cervical cancer, women age 21–65 years should get screened for cervical cancer at regular intervals and get follow-up care as recommended by their doctor or nurse.
Q: How do we know that the HPV vaccine is safe?
A: The United States currently has the safest, most effective vaccine supply in history. Years of testing are required by law to ensure the safety of vaccines before they are made available for use in the United States. This process can take ten years or longer. Once a vaccine is in use, CDC and the Food and Drug Administration (FDA) monitor any associated side effects or possible side effects (adverse events) through the Vaccine Adverse Event Reporting System and other vaccine safety systems.
All three HPV vaccines—Cervarix®, Gardasil®, and Gardasil® 9—went through years of extensive safety testing before they were licensed by FDA. Cervarix® was studied in clinical trials with more than 30,000 females. Gardasil® trials included more than 29,000 females and males, and Gardasil® 9 trials included more than 15,000 females and males. No serious safety concerns were identified in these clinical trials. FDA only licenses a vaccine if it is safe, effective, and the benefits outweigh the risks. CDC and FDA continue to monitor HPV vaccines to make sure they are safe and beneficial for the public.
Q: What are the possible side effects of HPV vaccination?
A: Vaccines, like any medicine, can have side effects. Many people who get HPV vaccine have no side effects at all. Some people report having very mild side effects, like a sore arm. The most common side effects are usually mild. Common side effects of HPV vaccine include:
- Pain, redness, or swelling in the arm where the shot was given
- Fever
- Headache or feeling tired
- Nausea
- Muscle or joint pain
Brief fainting spells and related symptoms (such as jerking movements) can happen after any medical procedure, including vaccination. Sitting or lying down while getting a shot and then staying that way for about 15 minutes can help prevent fainting and injuries caused by falls that could occur from fainting.
On very rare occasions, severe (anaphylactic) allergic reactions may occur after vaccination. People with severe allergies to any component of a vaccine should not receive that vaccine.
HPV vaccine does not cause HPV infection or cancer. HPV vaccine is made from one protein from the virus, and is not infectious, meaning that it cannot cause HPV infection or cancer. Not receiving HPV vaccine at the recommended ages can leave one vulnerable to cancers caused by HPV.
There are no data that suggest getting HPV vaccine will have an effect on future fertility for women. In fact, getting vaccinated and protecting against HPV-related cancers can help women and families have healthy pregnancies and healthy babies.
Not getting HPV vaccine leaves people vulnerable to HPV infection and related cancers. Treatments for cancers and precancers might include surgery, chemotherapy, and/or radiation, which might cause pregnancy complications or leave someone unable to have children.
Q: Why is this vaccine not mandatory for school entry?
A: Each state determines which vaccines are required for school entry. Many factors are taken into consideration before requiring any vaccine for school entry, including: community support for the requirement, financial resources needed to implement the requirement, burden on school personnel for enforcing the requirement, vaccine supply, and current vaccination coverage levels.
Since almost every state requires Tdap (tetanus, diphtheria, and acellular pertussis vaccine) for middle school entry, parents can use this visit to the doctor to get the first HPV and quadrivalent meningococcal conjugate vaccines for their preteen at the same time.
Q: How can someone get help paying for HPV vaccine?
A: The Vaccines for Children (VFC) program helps families of eligible children who might not otherwise have access to vaccines. The program provides vaccines at no cost to children ages 18 years and younger who are uninsured, Medicaid-eligible, or American Indian/Alaska Native. To learn more, see VFC program.
Human Papillomavirus (HPV) and Cancer

Human papillomavirus (HPV) causes most cervical cancers, as well as some cancers of the vagina, vulva, penis, anus, rectum, and oropharynx (cancers of the back of the throat, including the base of the tongue and tonsils).
HPV vaccines are recommended for preteen girls and boys to protect against HPV infection. All kids who are 11 or 12 years old should get the HPV vaccine. Teens who did not get the vaccine or did not get all doses when they were younger should get it now.
Two screening tests can help prevent cervical cancer or find it early. The Pap test is recommended for women between ages 21 and 65. If you are 30 years old or older, you may choose to have an HPV test along with the Pap test.
Gynecologic Cancers

Five main types of cancer affect a woman’s reproductive organs: cervical, ovarian, uterine, vaginal, and vulvar. As a group, they are referred to as gynecologic cancers. Each gynecologic cancer is unique, with different signs, symptoms, and risk factors (things that may increase your chance of getting cancer).
All women are at risk for gynecologic cancers, and risk increases with age. You can lower your risk for some of these cancers. When gynecologic cancers are found early, treatment works best.
CDC promotes awareness of gynecologic cancers through its national awareness campaign, Inside Knowledge: Get the Facts About Gynecologic Cancer.
CDC’s National Breast and Cervical Cancer Early Detection Program provides breast and cervical cancer screenings and diagnostic services to low-income, uninsured, and underinsured women across the United States. Find out if you qualify.
Source: CDC

What are venereal warts?
Venereal warts, also called condyloma, are a common sexually transmitted disease (STD) caused by the human papillomavirus (HPV) that affects the skin or mucous membranes. The virus may cause cauliflower-like fleshy growths in moist areas in and around the sex organs. In many cases, warts are not visible to the naked eye.
Who gets venereal warts?
Any sexually active person can be infected with venereal warts. Most often, venereal warts are found in young (age 15 to 30 years) people who have multiple sex partners. Those whose immune systems are compromised are more likely to become infected and to have a more serious infection than others.
How are venereal warts spread?
Venereal warts are generally spread through direct skin-to-skin contact during vaginal, anal and oral sex with someone who is infected. HPV can also be spread from mother to child (usually found in the child's throat or mouth) during birth.
What are the symptoms of venereal warts?
Venereal warts appear as soft, fleshy growths that vary in size, are frequently painless and can be raised, pointed or flat. The warts may appear singly or in clusters
How soon do symptoms appear?
The average incubation period, which begins immediately after the initial sexual contact with an infected person, is usually two to three months but can range from one to 20 months. However, when HPV is transmitted from one person to another, the virus infects the top layers of the skin and can remain inactive or latent for months or possibly years before warts or other signs of HPV infection appear. In couples that have not had sex partners for many years, the woman may develop an abnormal Pap smear because of previous contact.
When and for how long is a person able to spread venereal warts?
HPV cannot be cured; therefore, the infected person is essentially contagious for life. Approximately two-thirds of the people who have sexual contact with a partner with genital warts will develop this disease. HPV infection can also be transmitted by people who have no visible lesions, but some researchers believe this condition is less contagious than overt genital warts.
Does past infection make a person immune?
No, previous infection with warts does not make a person immune from repeat infection.
What is the treatment for venereal warts?
Genital wart therapies can be administered by the patient or health provider. Providers can treat with a chemical called podophyllin, surgical removal or, in some cases, warts may be "frozen" and removed by a process called cryosurgery. In other cases, providers can order podofilox solution and gel, or imiquimid cream, that the patient applies as prescribed. Several treatment sessions are usually required.
What can be the effect of not being treated for venereal warts?
If a person is not treated, the warts will, in some cases, continue to grow and spread. There may be an increased risk of cancer of the cervix, vulva, penis or anus among people who are infected with particular strains of HPV in those areas.
What can be done to prevent the spread of venereal warts?
There are a number of ways to prevent the spread of venereal warts:
- limit your number of sex partners;
- use a male or female condom**;
- carefully wash genitals after sexual relations;
- if you think you are infected, avoid sexual contact and visit your local STD clinic, a hospital or your doctor;
- notify all sexual contacts immediately so they can obtain examination and treatment.
** Remember that use of condoms may prevent the virus from coming in contact with susceptible skin areas. However, since HPV can infect the scrotum and vulva, transmission can occur outside condom-covered areas.
NYS. Dept of Health
CONDITION: Gonorrhea (Clap)
What is gonorrhea?
Gonorrhea (gon-uh-REE-uh) is a common sexually transmitted infection (STI). It’s caused by a type of bacteria that can grow in warm, moist areas of the reproductive tract, like the cervix, uterus, and fallopian tubes in women. It can grow in the urethra in men and women. It can also grow in the mouth, throat, eyes, and anus.

How do you get gonorrhea?
You can get gonorrhea during vaginal, oral, or anal sex with an infected partner. A man does not need to ejaculate to pass the infection or to become infected. Touching infected sex organs, like the vagina or penis, and then touching your eyes can cause an eye infection. Gonorrhea is not spread by shaking hands or sitting on toilet seats.
Gonorrhea also can be passed from a pregnant woman to her baby during delivery. In babies, gonorrhea infection can cause blindness, joint infection, or a life-threatening blood infection.
Who is at risk for gonorrhea?
- People who have had gonorrhea or other STIs in the past
- Anyone who has a new or multiple sexual partners
- Anyone who doesn't use a male condom correctly
- Sex workers
- Drug users
What are the symptoms of gonorrhea?
Many women who have gonorrhea do not have symptoms. When a woman does have symptoms, they often appear within 10 days of getting the STI. But symptoms can be so mild or general that they are overlooked or mistaken for something else.


A woman may have some of these symptoms:
- Pain or burning when passing urine
- Vaginal discharge that is yellow or sometimes bloody
- Bleeding between menstrual periods
- Heavy bleeding with periods
- Pain during sex
If you have any of these symptoms, stop having sex and see a doctor right away. Women with gonorrhea are at risk of developing serious health problems, whether or not there are symptoms.
For women and men, symptoms of an anal infection can include discharge, soreness, bleeding, or itching of the anus, and painful bowel movements. Infections in the throat may cause a sore throat but usually cause no symptoms. With an eye infection, symptoms may include redness, itching, or discharge from the eye.
For men, symptoms can include:
- Discharge from or pain inside the penis
- Pain or burning while passing urine
- Painful or swollen testicles
If your partner has any of these symptoms, stop having sex and ask your doctor about testing for both of you.
Are there tests for gonorrhea?
Yes. There are 3 types of tests for gonorrhea:
- Swab sample. A swab sample from the part of the body likely to be infected (cervix, urethra, penis, rectum, or throat) can be sent to a lab for testing.
- Urine test. Gonorrhea in the cervix or urethra can be diagnosed with a urine sample sent to a lab.
- Gram stain. This is done right in a clinic or doctor's office. A sample from the urethra or a cervix is placed on a slide and stained with dye. It allows the doctor to see the bacteria under a microscope. This test works better for men than for women.
Talk to your doctor about getting tested if you have any symptoms of gonorrhea, if you think you or your partner could have it, or if you know your partner has it. If you are tested for gonorrhea, you also should be tested for other STIs, including chlamydia, syphilis, and HIV.
How is gonorrhea treated?
Antibiotics are used to cure gonorrhea. But more and more people are becoming infected with types of gonorrhea that do not respond well to drugs. This problem is making it harder to treat gonorrhea. Many people who have gonorrhea also have chlamydia. So, doctors often give medicine to treat both STIs at the same time. For treatment to work, you must finish all the medicine that your doctor gives you, even if the symptoms go away. If symptoms don’t go away after treatment, see your doctor. Although treatment can cure the infection, it cannot fix any permanent damage done by the infection. Also, you can get gonorrhea again if you have sex with an infected person.
What happens if gonorrhea isn't treated?
Gonorrhea that is not treated can cause these serious problems in women:
- Pelvic inflammatory disease (PID). PID is an infection of a woman's reproductive organs above the cervix, such as the fallopian tubes and ovaries. Untreated gonorrhea is a common cause of PID. PID can lead to infertility, pregnancy problems, and pelvic pain. Some women have no symptoms of PID, and the damage caused by PID cannot be fixed. This is why finding out about and treating gonorrhea is so important.
- Widespread infection to other parts of the body, like the blood, joints, or heart.
- Increased risk of getting HIV or spreading HIV.
Can gonorrhea cause problems during pregnancy?
Yes. A pregnant woman with untreated gonorrhea has a higher risk of miscarriage, preterm birth, or having her water break too early. Also, her baby could get the infection while passing through the birth canal during delivery. This can cause blindness, joint infection, or a life-threatening blood infection in the baby. Treating the newborn’s eyes with medicine right after birth can prevent eye infection. Treatment of gonorrhea as soon as it is found in pregnant women will lower the risk of these problems. All sex partners of pregnant women with gonorrhea must also be treated. If you are pregnant, ask your doctor about testing for STIs, including gonorrhea. Testing is simple, and treatment usually cures the infection and prevents problems for the baby.

How can I keep from getting gonorrhea?
There are steps you can take to lower your risk of getting gonorrhea:
- Don’t have sex. The surest way to keep from getting gonorrhea is to practice abstinence. This means not having vaginal, oral, or anal sex.
- Be faithful. Having a sexual relationship with one partner who has been tested for gonorrhea and is not infected is another way to lower your risk of getting infected. Be faithful to each other. This means you only have sex with each other and no one else.
- Use condoms. Use condoms the right way and every time you have vaginal, anal, or oral sex. Because a man does not need to ejaculate to give or get gonorrhea, make sure to put on the condom before the penis touches the vagina, mouth, or anus. Use a new condom if you want to have sex again or in a different way. For vaginal sex, use a latex male condom or a female polyurethane condom. For anal sex, use a latex male condom. For oral sex use a male latex condom. A dental dam might offer some protection during oral sex (mouth to vagina/anus).
- Know that some methods of birth control, like birth control pills, shots, implants, or diaphragms, will not protect you from STIs, including gonorrhea. If you use one of these methods, be sure to also use a condom correctly every time you have sex.
- Talk with your sex partner(s) about STIs and using condoms. It’s up to you to make sure you are protected. Remember, it’s your body! For more information, call the Centers for Disease Control and Prevention at 800-CDC-INFO (232-6348).
- Talk frankly with your doctor and your sex partner(s) about any STIs you or your partner has or has had. Talk about symptoms, such as sores or discharge. Try not to be embarrassed. Being honest could prevent serious health problems.
- Have a yearly pelvic exam. Ask your doctor if you should be tested for gonorrhea or other STIs, and how often you should be retested. Testing for many STIs is simple and often can be done during your checkup. The sooner gonorrhea is found, the more likely it can be cured before permanent damage is done.
- If you are pregnant, get tested for gonorrhea. Get tested as soon as you think you may be pregnant.

I just found out I have gonorrhea. What should I do?
- Finish all the medicine that your doctor gives you. Even if the symptoms go away, you still need to finish treatment. If symptoms continue after treatment, see your doctor.
- Talk with your sex partner(s). Your sex partner(s) should get tested and treated for gonorrhea, even if they don’t have any symptoms.
- Avoid sexual contact until you and your partner(s) have been treated and cured. People who have had gonorrhea and were treated can get infected again if they have sexual contact with a person who has gonorrhea.
- Once you have been treated and cured, take steps to lower your risk from getting gonorrhea again.
More information on gonorrhea
For more information about gonorrhea, call womenshealth.gov at 800-994-9662 (TDD: 888-220-5446) or contact the following organizations:
- Sexually Transmitted Diseases (STDs) CDC, HHS
Phone: 800-CDC-INFO (232-6348)
Source: Office on Women's Health, HHS
CONDITION: Hepatitis A
The A, B, Cs of Viral Hepatitis

The A, B, Cs of Viral Hepatitis

Dr T.V.Rao, MD
Viral hepatitis is an infection that affects the liver. There are at least six different types of hepatitis (A-G), with the three most common types being hepatitis A, hepatitis B and hepatitis C. Hepatitis A is an acute infection and people usually improve without treatment. Hepatitis B and hepatitis C can cause a chronic, persistent infection, which can lead to chronic liver disease. There is a vaccine to prevent hepatitis A and B, however there is not one for hepatitis C.
The New York State Department of Health, along with the New York State County Health Departments, offer ways to control and prevent the spread of hepatitis infection. Public health clinics, located in each county, may offer testing and vaccination (hepatitis A, hepatitis B) to those at risk for hepatitis. In addition, hepatitis counseling and educational information is offered to individuals who may have been exposed to hepatitis, engage in behaviors putting them at risk for developing infection, and to those who may already know they are infected and want to learn about how they can protect others from becoming infected.
For more information about hepatitis testing, counseling and education in your county, please contact your county health department.
Hepatitis A


Hepatitis A is caused by the hepatitis A virus (HAV). The virus is found in the stool (feces) of HAV-infected people. Hepatitis A can easily spread from one person to another by putting something in the mouth (even though it may look clean) that has been contaminated with the stool of a person with hepatitis A. This can happen when people do not wash their hands after using the toilet and then touch or prepare other people’s food.
- Are you at risk for hepatitis A?
- Learn more about hepatitis A...
Hepatitis B
Hepatitis B is caused by the hepatitis B virus (HBV). The virus is found in blood and certain body fluids. Hepatitis B is spread when a person who is not immune comes in contact with blood or body fluid from an infected person. Hepatitis B is spread by having sex with an infected person without a condom, sharing needles or "works" when "shooting" drugs, needlesticks or sharps exposures in a health care setting, or from an infected mother to her baby during vaginal birth. Exposure to blood in ANY situation can be a risk for transmission.
- Are you at risk for hepatitis B?
- Learn more about hepatitis B...
Hepatitis C
Hepatitis C is caused by the hepatitis C virus (HCV). The virus is found in blood and certain body fluids. It is spread when a person who is not immune comes in contact with blood or body fluids from an infected person. Hepatitis C is spread through sharing needles or "works" when "shooting" drugs, through needlestick or sharps exposures in a health care setting, or sometimes from an infected mother to her baby during vaginal birth. It is possible to get hepatitis C from sex, but it is uncommon
NYS Health Dept.
What is hepatitis?
“Hepatitis” means inflammation of the liver. Toxins, certain drugs, some diseases, heavy alcohol use, and bacterial and viral infections can all cause hepatitis. Hepatitis is also the name of a family of viral infections that affect the liver; the most common types are Hepatitis A, Hepatitis B, and Hepatitis C.
What is the difference between Hepatitis A, Hepatitis B, and Hepatitis C?
Hepatitis A, Hepatitis B, and Hepatitis C are diseases caused by three different viruses. Although each can cause similar symptoms, they have different modes of transmission and can affect the liver differently. Hepatitis A appears only as an acute or newly occurring infection and does not become chronic. People with Hepatitis A usually improve without treatment. Hepatitis B and Hepatitis C can also begin as acute infections, but in some people, the virus remains in the body, resulting in chronic disease and long term liver problems. There are vaccines to prevent Hepatitis A and B; however, there is not one for Hepatitis C. If a person has had one type of viral hepatitis in the past, it is still possible to get the other types.
What is Hepatitis A?
Hepatitis A is a contagious liver disease that results from infection with the Hepatitis A virus. It can range in severity from a mild illness lasting a few weeks to a severe illness lasting several months. Hepatitis A is usually spread when a person ingests fecal matter — even in microscopic amounts — from contact with objects, food, or drinks contaminated by the feces, or stool, of an infected person.
Statistics
How common is Hepatitis A in the United States?
In the United States, there were an estimated 25,000 new Hepatitis A virus infections in 2007. (However, the official number of reported Hepatitis A cases is much lower since many people who are infected never have symptoms and are never reported to public health officials.)
Is Hepatitis A decreasing in the United States?
Yes. Rates of Hepatitis A in the United States are the lowest they have been in 40 years. The Hepatitis A vaccine was introduced in 1995 and health professionals now routinely vaccinate all children, travelers to certain countries, and persons at risk for the disease. Many experts believe Hepatitis A vaccination has dramatically affected rates of the disease in the United States.
Transmission / Exposure
How is Hepatitis A spread?
Hepatitis A is usually spread when the Hepatitis A virus is taken in by mouth from contact with objects, food, or drinks contaminated by the feces (or stool) of an infected person. A person can get Hepatitis A through:
- Person to person contact
- when an infected person does not wash his or her hands properly after going to the bathroom and touches other objects or food
- when a parent or caregiver does not properly wash his or her hands after changing diapers or cleaning up the stool of an infected person
- when someone has sex or sexual contact with an infected person. (not limited to anal-oral contact)
- Contaminated food or water
- Hepatitis A can be spread by eating or drinking food or water contaminated with the virus. (This can include frozen or undercooked food.) This is more likely to occur in countries where Hepatitis A is common and in areas where there are poor sanitary conditions or poor personal hygiene. The food and drinks most likely to be contaminated are fruits, vegetables, shellfish, ice, and water. In the United States, chlorination of water kills Hepatitis A virus that enters the water supply.
Who is at risk for Hepatitis A?
Although anyone can get Hepatitis A, in the United States, certain groups of people are at higher risk, such as those who:
- Travel to or live in countries where Hepatitis A is common
- Are men who have sexual contact with other men
- Use illegal drugs, whether injected or not
- Have clotting-factor disorders, such as hemophilia
- Live with someone who has Hepatitis A
- Have oral-anal sexual contact with someone who has Hepatitis A
I think I have been exposed to Hepatitis A. What should I do?
If you have any questions about potential exposure to Hepatitis A, call your health professional or your local or state health department.
If you were recently exposed to Hepatitis A virus and have not been vaccinated against Hepatitis A, you might benefit from an injection of either immune globulin or Hepatitis A vaccine. However, the vaccine or immune globulin must be given within the first 2 weeks after exposure to be effective. A health professional can decide what is best on the basis of your age and overall health.
What should I do if I ate at a restaurant that had an outbreak of Hepatitis A?
Talk to your health professional or a local health department official for guidance. Outbreaks usually result from one of two sources of contamination: an infected food handler or an infected food source. Your health department will investigate the cause of the outbreak.
Keep in mind that most people do not get sick when someone at a restaurant has Hepatitis A. However, if an infected food handler is infectious and has poor hygiene, the risk goes up for patrons of that restaurant. In such cases, health officials might try to identify patrons and provide Hepatitis A vaccine or immune globulin if they can find them within 2 weeks of exposure.
On rare occasions, the source of the infection can be traced to contaminated food. Foods can become contaminated at any point along the process: growing, harvesting, processing, handling, and even after cooking. In these cases, health officials will try to determine the source of the contamination and the best ways to minimize health threats to the public.
What is postexposure prophylaxis or PEP?
PEP or postexposure prophylaxis refers to trying to prevent or treat a disease after someone is exposed to it.
Who should get PEP after being exposed to Hepatitis A?
A health professional can decide whether or not a person needs PEP after exposure to Hepatitis A. People who might benefit from PEP include those who:
- Live with someone who has Hepatitis A
- Have recently had sexual contact with someone who has Hepatitis A
- Have recently shared injection or non-injection illegal drugs with someone who has Hepatitis A
- Have had ongoing, close personal contact with a person with Hepatitis A, such as a regular babysitter or caregiver
- Have been exposed to food or water known to be contaminated with Hepatitis A virus
If I have had Hepatitis A in the past, can I get it again?
No. Once you recover from Hepatitis A, you develop antibodies that protect you from the virus for life. An antibody is a substance found in the blood that the body produces in response to a virus. Antibodies protect the body from disease by attaching to the virus and destroying it.
Can I donate blood if I have had Hepatitis A?
If you had Hepatitis A when you were 11 years of age or older, you cannot donate blood. If you had Hepatitis A before age 11, you may be able donate blood. Check with your blood donation center.
How long does Hepatitis A virus survive outside the body?
The Hepatitis A virus is extremely hearty. It is able to survive the body’s highly acidic digestive tract and can live outside the body for months. High temperatures, such as boiling or cooking food or liquids for at least 1 minute at 185°F (85°C), kill the virus, although freezing temperatures do not.
Symptoms

Does Hepatitis A cause symptoms?
Not always. Some people get Hepatitis A and have no symptoms of the disease. Adults are more likely to have symptoms than children.
What are the symptoms of Hepatitis A?
Some people with Hepatitis A do not have any symptoms. If you do have symptoms, they may include the following:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice (a yellowing of the skin or eyes)
How soon after exposure to Hepatitis A will symptoms appear?
If symptoms occur, they usually appear anywhere from 2 to 6 weeks after exposure. Symptoms usually develop over a period of several days.
How long do Hepatitis A symptoms last?
Symptoms usually last less than 2 months, although some people can be ill for as long as 6 months.
Can a person spread Hepatitis A without having symptoms?
Yes. Many people, especially children, have no symptoms. In addition, a person can transmit the virus to others up to 2 weeks before symptoms appear.
How serious is Hepatitis A?
Almost all people who get Hepatitis A recover completely and do not have any lasting liver damage, although they may feel sick for months. Hepatitis A can sometimes cause liver failure and death, although this is rare and occurs more commonly in persons 50 years of age or older and persons with other liver diseases, such as Hepatitis B or C.
Diagnosis / Treatment
How will I know if I have Hepatitis A?
A doctor can determine if you have Hepatitis A by discussing your symptoms and taking a blood sample.
How is Hepatitis A treated?
There are no special treatments for Hepatitis A. Most people with Hepatitis A will feel sick for a few months before they begin to feel better. A few people will need to be hospitalized. During this time, doctors usually recommend rest, adequate nutrition, and fluids. People with Hepatitis A should check with a health professional before taking any prescription pills, supplements, or over-the-counter medications, which can potentially damage the liver. Alcohol should be avoided.
Prevention / Vaccination
Can Hepatitis A be prevented?
Yes. The best way to prevent Hepatitis A is through vaccination with the Hepatitis A vaccine. Vaccination is recommended for all children, for travelers to certain countries, and for people at high risk for infection with the virus. Frequent handwashing with soap and warm water after using the bathroom, changing a diaper, or before preparing food can help prevent the spread of Hepatitis A.
What is the Hepatitis A vaccine?
The Hepatitis A vaccine is a shot of inactive Hepatitis A virus that stimulates the body's natural immune system. After the vaccine is given, the body makes antibodies that protect a person against the virus. An antibody is a substance found in the blood that is produced in response to a virus invading the body. These antibodies are then stored in the body and will fight off the infection if a person is exposed to the virus in the future.
Who should get vaccinated against Hepatitis A?
Hepatitis A vaccination is recommended for:
- All children at age 1 year
- Travelers to countries that have high rates of Hepatitis A
- Men who have sexual contact with other men
- Users of injection and non-injection illegal drugs
- People with chronic (lifelong) liver diseases, such as Hepatitis B or Hepatitis C
- People who are treated with clotting-factor concentrates
- People who work with Hepatitis A infected animals or in a Hepatitis A research laboratory
How is the Hepatitis A vaccine given?
The Hepatitis A vaccine is given as 2 shots, 6 months apart. The Hepatitis A vaccine also comes in a combination form, containing both Hepatitis A and B vaccine, that can be given to persons 18 years of age and older. This form is given as 3 shots, over a period of 6 months.
Is the Hepatitis A vaccine effective?
Yes, the Hepatitis A vaccine is highly effective in preventing Hepatitis A virus infection. Protection begins approximately 2 to 4 weeks after the first injection. A second injection results in long-term protection.
Is the Hepatitis A vaccine safe?
Yes, the Hepatitis A vaccine is safe. No serious side effects have resulted from the Hepatitis A vaccine. Soreness at the injection site is the most common side effect reported. As with any medicine, there are very small risks that a serious problem could occur after someone gets the vaccine. However, the potential risks associated with Hepatitis A are much greater than the potential risks associated with the Hepatitis A vaccine. Before the Hepatitis A vaccine became available in the Unites States, more than 250,000 people were infected with Hepatitis A virus each year. Since the licensure of the first Hepatitis A vaccine in 1995, millions of doses of Hepatitis A vaccine have been given in the United States and worldwide.
Who should not receive the Hepatitis A vaccine?
People who have ever had a serious allergic reaction to the Hepatitis A vaccine or who are known to be allergic to any part of the Hepatitis A vaccine should not receive the vaccine. Tell your doctor if you have any severe allergies. Also, the vaccine is not licensed for use in infants under age 1 year.
Who should get the Hepatitis A vaccine before traveling?
Anyone traveling to or working in countries with high rates of Hepatitis A should talk to a health professional about getting vaccinated. He or she is likely to recommend vaccination or a shot of immune globulinbefore traveling to countries in Central or South America, Mexico, and certain parts of Asia, Africa, and Eastern Europe. CDC’s Travelers’ Health site provides detailed information about Hepatitis A and other recommended vaccines at wwwn.cdc.gov/travel/yellowBookCH4-Hep A.aspx.
What is immune globulin?
Immune globulin is a substance made from human blood plasma that contains antibodies that protect against infection. It is given as a shot and provides short-term protection (approximately 3 months) against Hepatitis A. Immune globulin can be given either before exposure to the Hepatitis A virus (such as before travel to a country where Hepatitis A is common) or to prevent infection after exposure to the Hepatitis A virus. Immune globulin must be given within 2 weeks after exposure for the best protection.
Why is the Hepatitis A vaccine recommended before traveling?
Traveling to places where Hepatitis A virus is common puts a person at high risk for Hepatitis A. The risk exists even for travelers to urban areas, those who stay in luxury hotels, and those who report that they have good hygiene and are careful about what they eat and drink. Travelers can minimize their risk by avoiding potentially contaminated water or food, such as drinking beverages (with or without ice) of unknown purity, eating uncooked shellfish, and eating uncooked fruits or vegetables that are not peeled or prepared by the traveler personally. Risk for infection increases with duration of travel and is highest for those who live in or visit rural areas, trek in back-country areas, or frequently eat or drink in settings with poor sanitation. Since a simple, safe vaccine exists, experts recommend that travelers to certain countries be vaccinated.
How soon before travel should the Hepatitis A vaccine be given?
The first dose of Hepatitis A vaccine should be given as soon as travel is planned. Two weeks or more before departure is ideal, but anytime before travel will provide some protection.
I'm leaving for my trip in a few days. Can I still get the Hepatitis A vaccine?
Experts now say that the first dose of Hepatitis A vaccine can be given at any time before departure. This will provide some protection for most healthy persons.
Will the Hepatitis A vaccine protect someone from other forms of hepatitis?
Hepatitis A vaccine will only protect someone from Hepatitis A. A separate vaccine is available for Hepatitis B. There is also a combination vaccine that protects a person from Hepatitis A and Hepatitis B. No vaccine is available for Hepatitis C at this time.
Can Hepatitis A vaccine be given to immunocompromised persons, such as hemodialysis patients or persons with AIDS?
Yes. Because Hepatitis A vaccine is inactivated (not “live”), it can be given to people with compromised immune systems.
Is it harmful to have an extra dose of Hepatitis A vaccine or to repeat the entire Hepatitis A vaccine series?
No, getting extra doses of Hepatitis A vaccine is not harmful.
What should be done if the last dose of Hepatitis A vaccine is delayed?
The second or last dose should be given by a health professional as soon as possible. The first dose does not need to be given again.
Where can I get the Hepatitis A vaccine?
Speak with your health professional or call your local public health department, may offer free or low-cost vaccines for adults. For children, check out http://www.cdc.gov/vaccines/programs/vfc/parents/default.htm.
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
SOURCE: NIAID, NIH
CONDITION: Hepatitis B
What is hepatitis?
“Hepatitis” means inflammation of the liver. Toxins, certain drugs, some diseases, heavy alcohol use, and bacterial and viral infections can all cause hepatitis. Hepatitis is also the name of a family of viral infections that affect the liver; the most common types are Hepatitis A, Hepatitis B, and Hepatitis C.
What is the difference between Hepatitis A, Hepatitis B, and Hepatitis C?

Hepatitis A, Hepatitis B, and Hepatitis C are diseases caused by three different viruses. Although each can cause similar symptoms, they have different modes of transmission and can affect the liver differently. Hepatitis A appears only as an acute or newly occurring infection and does not become chronic. People with Hepatitis A usually improve without treatment. Hepatitis B and Hepatitis C can also begin as acute infections, but in some people, the virus remains in the body, resulting in chronic disease and long-term liver problems. There are vaccines to prevent Hepatitis A and B; however, there is not one for Hepatitis C. If a person has had one type of viral hepatitis in the past, it is still possible to get the other types.
What is Hepatitis B?

Hepatitis B is a contagious liver disease that ranges in severity from a mild illness lasting a few weeks to a serious, lifelong illness. It results from infection with the Hepatitis B virus. Hepatitis B can be either “acute” or “chronic.”
Acute Hepatitis B virus infection is a short-term illness that occurs within the first 6 months after someone is exposed to the Hepatitis B virus. Acute infection can — but does not always — lead to chronic infection.
Chronic Hepatitis B virus infection is a long-term illness that occurs when the Hepatitis B virus remains in a person’s body.
Statistics
How common is acute Hepatitis B in the United States?
In 2007, there were an estimated 43,000 new Hepatitis B virus infections in the United States. However, the official number of reported Hepatitis B cases is much lower. Many people don’t know they are infected or may not have symptoms and therefore never seek the attention of medical or public health officials.
Has the number of people in the United States with acute Hepatitis B been decreasing?
Yes, rates of acute Hepatitis B in the United States have declined by approximately 82% since 1990. At that time, routine Hepatitis B vaccination of children was implemented and has dramatically decreased the rates of the disease in the United States, particularly among children.
How common is chronic Hepatitis B in the United States?
In the United States, an estimated 800,000 to 1.4 million persons have chronic Hepatitis B virus infection.
How common is chronic Hepatitis B outside the United States?
Globally, chronic Hepatitis B affects approximately 350 million people and contributes to an estimated 620,000 deaths worldwide each year.
Transmission / Exposure
How likely is it that acute Hepatitis B will become chronic?
The likelihood depends upon the age at which someone becomes infected. The younger a person is when infected with Hepatitis B virus, the greater his or her chance of developing chronic Hepatitis B. Approximately 90% of infected infants will develop chronic infection. The risk goes down as a child gets older. Approximately 25%–50% of children infected between the ages of 1 and 5 years will develop chronic hepatitis. The risk drops to 6%–10% when a person is infected over 5 years of age. Worldwide, most people with chronic Hepatitis B were infected at birth or during early childhood.
How is Hepatitis B spread?
Hepatitis B is spread when blood, semen, or other body fluid infected with the Hepatitis B virus enters the body of a person who is not infected. People can become infected with the virus during activities such as:
- Birth (spread from an infected mother to her baby during birth)
- Sex with an infected partner
- Sharing needles, syringes, or other drug-injection equipment
- Sharing items such as razors or toothbrushes with an infected person
- Direct contact with the blood or open sores of an infected person
- Exposure to blood from needlesticks or other sharp instruments
Can a person spread Hepatitis B and not know it?
Yes. Many people with chronic Hepatitis B virus infection do not know they are infected since they do not feel or look sick. However, they still can spread the virus to others and are at risk of serious health problems themselves.
Can Hepatitis B be spread through sex?
Yes. Among adults in the United States, Hepatitis B is most commonly spread through sexual contact and accounts for nearly two-thirds of acute Hepatitis B cases. In fact, Hepatitis B is 50–100 times more infectious than HIV and can be passed through the exchange of body fluids, such as semen, vaginal fluids, and blood.
Can Hepatitis B be spread through food?
Unlike Hepatitis A, it is not spread routinely through food or water. However, there have been instances in which Hepatitis B has been spread to babies when they have received food pre-chewed by an infected person.
What are ways Hepatitis B is not spread?
Hepatitis B virus is not spread by sharing eating utensils, breastfeeding, hugging, kissing, holding hands, coughing, or sneezing.
Who is at risk for Hepatitis B?
Although anyone can get Hepatitis B, some people are at greater risk, such as those who:
- Have sex with an infected person
- Have multiple sex partners
- Have a sexually transmitted disease
- Are men who have sexual contact with other men
- Inject drugs or share needles, syringes, or other drug equipment
- Live with a person who has chronic Hepatitis B
- Are infants born to infected mothers
- Are exposed to blood on the job
- Are hemodialysis patients
- Travel to countries with moderate to high rates of Hepatitis B
If I think I have been exposed to the Hepatitis B virus, what should I do?
If you are concerned that you might have been exposed to the Hepatitis B virus, call your health professional or your health department. If a person who has been exposed to Hepatitis B virus gets the Hepatitis B vaccine and/or a shot called “HBIG” (Hepatitis B immune globulin) within 24 hours, Hepatitis B infection may be prevented.
How long does the Hepatitis B virus survive outside the body?
Hepatitis B virus can survive outside the body at least 7 days. During that time, the virus can still cause infection if it enters the body of a person who is not infected.
How should blood spills be cleaned from surfaces to make sure that Hepatitis B virus is gone?
All blood spills — including those that have already dried — should be cleaned and disinfected with a mixture of bleach and water (one part household bleach to 10 parts water). Gloves should always be used when cleaning up any blood spills. Even dried blood can present a risk to others.
If I had Hepatitis B in the past, can I get it again?
No, once you recover from Hepatitis B, you develop antibodies that protect you from the virus for life. An antibody is a substance found in the blood that the body produces in response to a virus. Antibodies protect the body from disease by attaching to the virus and destroying it. However, some people, especially those infected during early childhood, remain infected for life because they never clear the virus from their bodies.
Can I donate blood, organs, or semen if I have Hepatitis B?
No, if you have ever tested positive for the Hepatitis B virus, experts recommend that you not donate blood, organs, or semen because this can put the recipient at great risk for getting hepatitis.
Symptoms
Does acute Hepatitis B cause symptoms?
Sometimes. Although a majority of adults develop symptoms from acute Hepatitis B virus infection, many young children do not. Adults and children over the age of 5 years are more likely to have symptoms. Seventy percent of adults will develop symptoms from the infection.
What are the symptoms of acute Hepatitis B?
Symptoms of acute Hepatitis B, if they appear, can include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice (yellow color in the skin or the eyes)
How soon after exposure to Hepatitis B will symptoms appear?
On average, symptoms appear 90 days (or 3 months) after exposure, but they can appear any time between 6 weeks and 6 months after exposure.
How long do acute Hepatitis B symptoms last?
Symptoms usually last a few weeks, but some people can be ill for as long as 6 months.
Can a person spread Hepatitis B without having symptoms?
Yes. Many people with Hepatitis B have no symptoms, but these people can still spread the virus.
What are the symptoms of chronic Hepatitis B?
Some people have ongoing symptoms similar to acute Hepatitis B, but most individuals with chronic Hepatitis B remain symptom free for as long as 20 or 30 years. About 15%–25% of people with chronic Hepatitis B develop serious liver conditions, such as cirrhosis (scarring of the liver) or liver cancer. Even as the liver becomes diseased, some people still do not have symptoms, although certain blood tests for liver function might begin to show some abnormalities.
How will I know if I have Hepatitis B?
Talk to your health professional. Since many people with Hepatitis B do not have symptoms, doctors diagnose the disease by one or more blood tests. These tests look for the presence of antibodies or antigens and can help determine whether you:
- have acute or chronic infection
- have recovered from infection
- are immune to Hepatitis B
- could benefit from vaccination
How serious is chronic Hepatitis B?
Chronic Hepatitis B is a serious disease that can result in long-term health problems, including liver damage, liver failure, liver cancer, or even death. Approximately 2,000–4,000 people die every year from Hepatitis B-related liver disease.
Tests
What are antigens and antibodies?
An antigen is a substance on the surface of a virus that causes a person's immune system to recognize and respond to it. When the body is exposed to an antigen, the body views it as foreign material and takes steps to neutralize the antigen by producing antibodies. An antibody is a substance found in the blood that the body produces in response to a virus. Antibodies protect the body from disease by attaching to the virus and destroying it.
What are the common blood tests available to diagnose Hepatitis B?
There are many different blood tests available to diagnose Hepatitis B. They can be ordered as an individual test or as a series of tests. Ask your health professional to explain what he or she hopes to learn from the tests and when you will get the results. Below are some of the common tests and their meanings. But remember: only your doctor can interpret your individual test results.
Hepatitis B Surface Antigen (HBsAg) is a protein on the surface of the Hepatitis B virus. It can be detected in the blood during acute or chronic Hepatitis B virus infection. The body normally produces antibodies to HBsAg as part of the normal immune response to infection.
A positive test means:
- A person has an acute or chronic Hepatitis B virus infection and can pass the virus to others
A negative test means:
- A person does not have the Hepatitis B virus in his or her blood
Hepatitis B Surface Antibody (anti-HBs) is an antibody that is produced by the body in response to the Hepatitis B surface antigen.
A positive test means:
- A person is protected or immune from getting the Hepatitis B virus for one of two reasons:
- he or she was successfully vaccinated against Hepatitis B
OR
- he or she recovered from an acute infection (and can’t get Hepatitis B again)
-
- Total Hepatitis B Core Antibody (anti-HBc) is an antibody that is produced by the body in response to a part of the Hepatitis B virus called the ”core antigen.” The meaning of this test often depends on the results of two other tests, anti-HBs and HBsAg.
A positive test means:
-
- A person is either currently infected with the Hepatitis B virus or was infected in the past
IgM Antibody to Hepatitis B Core Antigen (IgM anti-HBc) is used to detect an acute infection.
A positive test means:
- A person was infected with Hepatitis B virus within the last 6 months
Hepatitis B “e” Antigen (HBeAg) is a protein found in the blood when the Hepatitis B virus is present during an active Hepatitis B virus infection.
A positive test means:
- A person has high levels of virus in his or her blood and can easily spread the virus to others
This test is also used to monitor the effectiveness of treatment for chronic Hepatitis B.
Hepatitis B e Antibody (HBeAb or anti-HBe) is an antibody that is produced by the body in response to the Hepatitis B “e” antigen.
A positive test means:
- A person has chronic Hepatitis B virus infection but is at lower risk of liver problems due to low levels of Hepatitis B virus in his or her blood
Hepatitis B Viral DNA refers to a test to detect the presence of Hepatitis B virus DNA in a person’s blood.
A positive test means:
- The virus is multiplying in a person’s body and he or she is highly contagious and can pass the virus to others
- If a person has a chronic Hepatitis B virus infection, the presence of viral DNA means that a person is possibly at increased risk for liver damage
This test is also used to monitor the effectiveness of drug therapy for chronic Hepatitis B virus infection.
Treatment
How is acute Hepatitis B treated?
There is no medication available to treat acute Hepatitis B. During this short-term infection, doctors usually recommend rest, adequate nutrition, and fluids, although some people may need to be hospitalized.
How is chronic Hepatitis B treated?
It depends. People with chronic Hepatitis B virus infection should seek the care or consultation of a doctor with experience treating Hepatitis B. This can include some internists or family medicine practitioners, as well as specialists such as infectious disease physicians, gastroenterologists, or hepatologists (liver specialists). People with chronic Hepatitis B should be monitored regularly for signs of liver disease and evaluated for possible treatment. Several medications have been approved for Hepatitis B treatment, and new drugs are in development. However, not every person with chronic Hepatitis B needs to be on medication, and the drugs may cause side effects in some patients.
What can people with chronic Hepatitis B do to take care of their liver?
People with chronic Hepatitis B should be monitored regularly by a doctor experienced in caring for people with Hepatitis B. They should avoid alcohol because it can cause additional liver damage. They also should check with a health professional before taking any prescription pills, supplements, or over-the-counter medications, as these can potentially damage the liver.
Prevention / Vaccination
Can Hepatitis B be prevented?
Yes. The best way to prevent Hepatitis B is by getting the Hepatitis B vaccine. The Hepatitis B vaccine is safe and effective and is usually given as 3-4 shots over a 6-month period.
What is the Hepatitis B vaccine series?
The Hepatitis B vaccine series is a sequence of shots that stimulate a person’s natural immune system to protect against HBV. After the vaccine is given, the body makes antibodies that protect a person against the virus. An antibody is a substance found in the blood that is produced in response to a virus invading the body. These antibodies are then stored in the body and will fight off the infection if a person is exposed to the Hepatitis B virus in the future.
Who should get vaccinated against Hepatitis B
Hepatitis B vaccination is recommended for:
- All infants, starting with the first dose of Hepatitis B vaccine at birth
- All children and adolescents younger than 19 years of age who have not been vaccinated
- People whose sex partners have Hepatitis B
- Sexually active persons who are not in a long-term, mutually monogamous relationship.
- Persons seeking evaluation or treatment for a sexually transmitted disease
- Men who have sexual contact with other men
- People who share needles, syringes, or other drug-injection equipment
- People who have close household contact with someone infected with the Hepatitis B virus
- Health care and public safety workers at risk for exposure to blood or blood-contaminated body fluids on the job
- People with end-stage renal disease, including predialysis, hemodialysis, peritoneal dialysis, and home dialysis patients
- Residents and staff of facilities for developmentally disabled persons
- Travelers to regions with moderate or high rates of Hepatitis B
- People with chronic liver disease
- People with HIV infection
- Anyone who wishes to be protected from Hepatitis B virus infection
In order to reach individuals at risk for Hepatitis B, vaccination is also recommended for anyone in or seeking treatment from the following:
- Sexually transmitted disease treatment facilities
- HIV testing and treatment facilities
- Facilities providing drug-abuse treatment and prevention services
- Health care settings targeting services to injection drug users
- Health care settings targeting services to men who have sex with men
- Chronic hemodialysis facilities and end-stage renal disease programs
- Correctional facilities
- Institutions and nonresidential day care facilities for developmentally disabled persons
When should a person get the Hepatitis B vaccine series?
Children and Adolescents
- All children should get their first dose of Hepatitis B vaccine at birth and complete the vaccine series by 6–18 months of age.
- All children and adolescents younger than 19 years of age who have not yet gotten the vaccine should also be vaccinated. "Catch-up" vaccination is recommended for children and adolescents who were never vaccinated or who did not get the entire vaccine series.
Adults:
- Any adult who is at risk for Hepatitis B virus infection or who wants to be vaccinated should talk to a health professional about getting the vaccine series.
For more information about Hepatitis B and other vaccines, see http://www.cdc.gov/vaccines/recs/schedules/default.htm.
Is the Hepatitis B vaccine recommended before international travel
The risk for Hepatitis B virus infection in international travelers is generally low, although people traveling to certain countries are at risk. Travelers to regions with moderate or high rates of Hepatitis B should get the Hepatitis B vaccine.
How is the Hepatitis B vaccine series given?
The Hepatitis B vaccine is usually given as a series of 3 or 4 shots over a 6-month period.
Is the Hepatitis B vaccine series effective?
Yes, the Hepatitis B vaccine is very effective at preventing Hepatitis B virus infection. After receiving all three doses, Hepatitis B vaccine provides greater than 90% protection to infants, children, and adults immunized before being exposed to the virus.
Is the Hepatitis B vaccine safe?
Yes, the Hepatitis B vaccine is safe. Soreness at the injection site is the most common side effect reported. As with any medicine, there are very small risks that a serious problem could occur after getting the vaccine. However, the potential risks associated with Hepatitis B are much greater than the risks the vaccine poses. Since the vaccine became available in 1982, more than 100 million people have received Hepatitis B vaccine in the United States and no serious side effects have been reported.
Is it harmful to have an extra dose of Hepatitis B vaccine or to repeat the entire Hepatitis B vaccine series?
No, getting extra doses of Hepatitis B vaccine is not harmful.
What should be done if Hepatitis B vaccine series was not completed?
Talk to your health professional to resume the vaccine series as soon as possible. The series does not need to be restarted.
Who should not receive the Hepatitis B vaccine?
The Hepatitis B vaccine is not recommended for people who have had serious allergic reactions to a prior dose of Hepatitis B vaccine or to any part of the vaccine. Also, it not recommended for anyone who is allergic to yeast because yeast is used when making the vaccine. Tell your doctor if you have any severe allergies.
Are booster doses of Hepatitis B vaccine necessary?
It depends. A “booster” dose of Hepatitis B vaccine is a dose that increases or extends the effectiveness of the vaccine. Booster doses are recommended only for hemodialysis patients and can be considered for other people with a weakened immune system. Booster doses are not recommended for persons with normal immune status who have been fully vaccinated.
Is there a vaccine that will protect me from both Hepatitis A and Hepatitis B?
Yes, there is a combination vaccine that protects people from both Hepatitis A and Hepatitis B. The combined Hepatitis A and B vaccine is usually given as three separate doses over a 6-month period.
Can I get the Hepatitis B vaccine at the same time as other vaccines?
Yes. Getting two different vaccines at the same time has not been shown to be harmful.
Where can I get the Hepatitis B vaccine?
Talk to your doctor or health professional or call your health department. Some clinics offer free or low-cost vaccines.
What is Hepatitis B immune globulin (HBIG)?
Hepatitis B immune globulin is a substance made from human blood samples that contains antibodies against the Hepatitis B virus. It is given as a shot and can provide short-term protection (approximately 3 months) against Hepatitis B.
Pregnancy and Hepatitis B
Are pregnant women tested for Hepatitis B?
Yes. When a pregnant woman comes in for prenatal care, she will be given a series of routine blood tests, including one that checks for the presence of Hepatitis B virus infection. This test is important because women infected with this virus can pass Hepatitis B to their babies during birth. But this can be prevented by giving the infant HBIG and the first Hepatitis B vaccine at birth, and then completing the series.
What if a pregnant woman has Hepatitis B?
If a pregnant woman has Hepatitis B, she can pass the infection to her baby during birth. But this can be prevented through a series of vaccinations and HBIG for her baby beginning at birth. Without vaccination, babies born to women with Hepatitis B virus infection can develop chronic infection, which can lead to serious health problems.
How does a baby get Hepatitis B?
A baby can get Hepatitis B from an infected mother during childbirth.
Can a baby be protected from getting Hepatitis B from his or her mother during birth?
Yes, almost all cases of Hepatitis B can be prevented if a baby born to an infected woman receives the necessary shots at the recommended times The infant should receive a shot called Hepatitis B immune globulin (HBIG) and the first dose of Hepatitis B vaccine within 12 hours of birth. Two or 3 additional shots of vaccine are needed over the next 1–15 months to help prevent Hepatitis B. The timing and total number of shots will be influenced by several factors, including the type of vaccine and the baby's age and weight. In addition, experts recommend that the baby be tested after completion of the vaccine series to make sure he or she is protected from the disease. To best protect your baby, follow the advice of his or her doctor.
What happens if a baby gets Hepatitis B?
Most newborns who become infected with Hepatitis B virus do not have symptoms, but they have a 90% chance of developing chronic Hepatitis B. This can eventually lead to serious health problems, including liver damage, liver cancer, and even death.
Do babies need the Hepatitis B vaccine even if a pregnant woman does not have Hepatitis B?
Yes. The Hepatitis B vaccine is recommended for all infants. CDC recommends that the infant get the first shot before leaving the hospital.
Why is the Hepatitis B vaccine recommended for all babies?
Hepatitis B vaccine is recommended for all babies so that they will be protected from a serious but preventable disease. Babies and young children are at much greater risk for developing a chronic infection if infected, but the vaccine can prevent this.
Research Activities
NIAID supports and conducts research on each of the five known hepatitis viruses—A, B, C, D and E. During the past 60 years, NIAID-supported investigators have been involved in many important breakthroughs in hepatitis research, including the discovery of the hepatitis A and E viruses, the development of one of the first diagnostic tests for hepatitis A, and studies that led to the creation of the hepatitis A vaccine and laid the foundation for advanced development of a hepatitis E vaccine. In addition to basic research to understand the molecular processes of hepatitis infection, our research involves significant focus on the development of new treatments and vaccines to prevent acute and chronic hepatitis infection.
Hepatitis B
Although vaccine-preventable, hepatitis B-induced liver cirrhosis and liver cancer kill about 3,000 people in the United States and roughly 620,000 people worldwide each year. The virus can be spread from mother to child during childbirth; through sex with an infected partner; through contact with the blood of an infected person and by sharing needles, syringes, razors or toothbrushes with an infected person. Co-infection with hepatitis B and HIV is common.
NIAID is working with researchers in academia and the pharmaceutical industry to screen hundreds of new drug compounds for potential antiviral activity against hepatitis B. The goal is to find new treatments that will work alone or in combination with current drugs to reduce or resolve chronic infections. For example, one candidate drug has shown promise in transgenic mice and is now being evaluated in rats.
Hepatitis C
Hepatitis C is primarily spread through contact with the blood of an infected individual, such as through needle-sharing practices of injection drug users, unsafe injection practices in healthcare facilities, mother-to-child transmission during childbirth, and infrequently, through sexual contact with an infected partner. Currently available drugs cure only a proportion of treated individuals, but new drugs in trials may significantly improve treatment success rates. There is no vaccine to prevent hepatitis C.
In March, NIAID-supported researchers began a Phase I/II clinical trial of a promising candidate vaccine to evaluate its safety, tolerability and protective ability against hepatitis C. NIAID is supporting several studies, including research at five Hepatitis C Cooperative Research Centers across the country, that focus on the immune response to infection and how treatment might strengthen this response. Additionally, NIAID researchers have conducted preclinical work on several candidate antivirals targeting hepatitis C and are developing biomarkers for predicting progression to hepatitis C-associated liver cancer and HIV co-infection.
Hepatitis E
Spread via contact with contaminated water or food, hepatitis E is rare in the United States but prevalent in south and central Asia, sub-Saharan Africa and the Middle East.
Studies have found that in certain regions, when pregnant women are infected with hepatitis E virus during the second or third trimester, their babies are at increased risk of poor health and birth defects. NIAID-funded researchers are testing the hypothesis that mothers with micronutrient deficiencies are more likely to experience this effect and what potentially could be done to prevent it. Other NIAID-supported scientists are studying whether hepatitis E virus can become reactivated after a bout of acute disease. Successful trials of hepatitis E vaccines have also taken place, but none have yet been licensed for use in the United States. In 2012, NIAID co-hosted a research workshop, “Hepatitis E in the United States,” with the goal of increasing awareness of the virus among clinicians.
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
SOURCE: NIAID, NIH
CONDITION: Hepatitis C
What is hepatitis?
“Hepatitis” means inflammation of the liver. Toxins, certain drugs, some diseases, heavy alcohol use, and bacterial and viral infections can all cause hepatitis. Hepatitis is also the name of a family of viral infections that affect the liver; the most common types are Hepatitis A, Hepatitis B, and Hepatitis C.

What is the difference between Hepatitis A, Hepatitis B, and Hepatitis C?
Hepatitis A, Hepatitis B, and Hepatitis C are diseases caused by three different viruses. Although each can cause similar symptoms, they have different modes of transmission and can affect the liver differently. Hepatitis A appears only as an acute or newly occurring infection and does not become chronic. People with Hepatitis A usually improve without treatment. Hepatitis B and Hepatitis C can also begin as acute infections, but in some people, the virus remains in the body, resulting in chronic disease and long-term liver problems. There are vaccines to prevent Hepatitis A and B; however, there is not one for Hepatitis C. If a person has had one type of viral hepatitis in the past, it is still possible to get the other types.
What is Hepatitis C?
Hepatitis C is a contagious liver disease that ranges in severity from a mild illness lasting a few weeks to a serious, lifelong illness that attacks the liver. It results from infection with the Hepatitis C virus (HCV), which is spread primarily through contact with the blood of an infected person. Hepatitis C can be either “acute” or “chronic.”
Acute Hepatitis C virus infection is a short-term illness that occurs within the first 6 months after someone is exposed to the Hepatitis C virus. For most people, acute infection leads to chronic infection.
Chronic Hepatitis C virus infection is a long-term illness that occurs when the Hepatitis C virus remains in a person’s body. Hepatitis C virus infection can last a lifetime and lead to serious liver problems, including cirrhosis (scarring of the liver) or liver cancer.
Statistics
How common is acute Hepatitis C in the United States?
In 2009, there were an estimated 16,000 acute Hepatitis C virus infections reported in the United States.
How common is chronic Hepatitis C in the United States?
An estimated 3.2 million persons in the United States have chronic Hepatitis C virus infection. Most people do not know they are infected because they don’t look or feel sick.
How likely is it that acute Hepatitis C will become chronic?
Approximately 75%–85% of people who become infected with Hepatitis C virus develop chronic infection.
Transmission / Exposure
How is Hepatitis C spread?
Hepatitis C is usually spread when blood from a person infected with the Hepatitis C virus enters the body of someone who is not infected. Today, most people become infected with the Hepatitis C virus by sharing needles or other equipment to inject drugs. Before 1992, when widespread screening of the blood supply began in the United States, Hepatitis C was also commonly spread through blood transfusions and organ transplants.
People can become infected with the Hepatitis C virus during such activities as
- Sharing needles, syringes, or other equipment to inject drugs
- Needlestick injuries in health care settings
- Being born to a mother who has Hepatitis C
Less commonly, a person can also get Hepatitis C virus infection through
- Sharing personal care items that may have come in contact with another person’s blood, such as razors or toothbrushes
- Having sexual contact with a person infected with the Hepatitis C virus
Can Hepatitis C be spread through sexual contact?
Yes, but the risk of transmission from sexual contact is believed to be low. The risk increases for those who have multiple sex partners, have a sexually transmitted disease, engage in rough sex, or are infected with HIV. More research is needed to better understand how and when Hepatitis C can be spread through sexual contact.
Can you get Hepatitis C by getting a tattoo or piercing?
A few major research studies have not shown Hepatitis C to be spread through licensed, commercial tattooing facilities. However, transmission of Hepatitis C (and other infectious diseases) is possible when poor infection-control practices are used during tattooing or piercing. Body art is becoming increasingly popular in the United States, and unregulated tattooing and piercing are known to occur in prisons and other informal or unregulated settings. Further research is needed to determine if these types of settings and exposures are responsible for Hepatitis C virus transmission.
Can Hepatitis C be spread within a household?
Yes, but this does not occur very often. If Hepatitis C virus is spread within a household, it is most likely a result of direct, through-the-skin exposure to the blood of an infected household member.
How should blood spills be cleaned from surfaces to make sure that Hepatitis C virus is gone?
Any blood spills — including dried blood, which can still be infectious — should be cleaned using a dilution of one part household bleach to 10 parts water. Gloves should be worn when cleaning up blood spills.
How long does the Hepatitis C virus survive outside the body?
The Hepatitis C virus can survive outside the body at room temperature, on environmental surfaces, for at least 16 hours but no longer than 4 days.
What are ways Hepatitis C is not spread?
Hepatitis C virus is not spread by sharing eating utensils, breastfeeding, hugging, kissing, holding hands, coughing, or sneezing. It is also not spread through food or water.
Who is at risk for Hepatitis C?
Some people are at increased risk for Hepatitis C, including
- Current injection drug users (currently the most common way Hepatitis C virus is spread in the United States)
- Past injection drug users, including those who injected only one time or many years ago
- Recipients of donated blood, blood products, and organs (once a common means of transmission but now rare in the United States since blood screening became available in 1992)
- People who received a blood product for clotting problems made before 1987
- Hemodialysis patients or persons who spent many years on dialysis for kidney failure
- People who received body piercing or tattoos done with non-sterile instruments
- People with known exposures to the Hepatitis C virus, such as
- Health care workers injured by needlesticks
- Recipients of blood or organs from a donor who tested positive for the Hepatitis C virus
- HIV-infected persons
- Children born to mothers infected with the Hepatitis C virus
Less common risks include:
- Having sexual contact with a person who is infected with the Hepatitis C virus
- Sharing personal care items, such as razors or toothbrushes, that may have come in contact with the blood of an infected person
What is the risk of a pregnant woman passing Hepatitis C to her baby?
Hepatitis C is rarely passed from a pregnant woman to her baby. About 6 of every 100 infants born to mothers with Hepatitis C become infected with the virus. However, the risk becomes greater if the mother has both HIV infection and Hepatitis C.
Can a person get Hepatitis C from a mosquito or other insect bite?
Hepatitis C virus has not been shown to be transmitted by mosquitoes or other insects.
Can I donate blood, organs, or semen if I have Hepatitis C?
No, if you ever tested positive for the Hepatitis C virus (or Hepatitis B virus), experts recommend never donating blood, organs, or semen because this can spread the infection to the recipient.
Symptoms
What are the symptoms of acute Hepatitis C?
Approximately 70%–80% of people with acute Hepatitis C do not have any symptoms. Some people, however, can have mild to severe symptoms soon after being infected, including
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice (yellow color in the skin or eyes)
How soon after exposure to Hepatitis C do symptoms appear?
If symptoms occur, the average time is 6–7 weeks after exposure, but this can range from 2 weeks to 6 months. However, many people infected with the Hepatitis C virus do not develop symptoms.
Can a person spread Hepatitis C without having symptoms?
Yes, even if a person with Hepatitis C has no symptoms, he or she can still spread the virus to others.
Is it possible to have Hepatitis C and not know it?
Yes, many people who are infected with the Hepatitis C virus do not know they are infected because they do not look or feel sick.
What are the symptoms of chronic Hepatitis C?
Most people with chronic Hepatitis C do not have any symptoms. However, if a person has been infected for many years, his or her liver may be damaged. In many cases, there are no symptoms of the disease until liver problems have developed. In persons without symptoms, Hepatitis C is often detected during routine blood tests to measure liver function and liver enzyme (protein produced by the liver) level.
How serious is chronic Hepatitis C?
Chronic Hepatitis C is a serious disease that can result in long-term health problems, including liver damage, liver failure, liver cancer, or even death. It is the leading cause of cirrhosis and liver cancer and the most common reason for liver transplantation in the United States. Approximately 15,000 people die every year from Hepatitis C related liver disease.
What are the long-term effects of Hepatitis C?
Of every 100 people infected with the Hepatitis C virus, about
- 75–85 people will develop chronic Hepatitis C virus infection; of those,
- 60–70 people will go on to develop chronic liver disease
- 5–20 people will go on to develop cirrhosis over a period of 20–30 years
- 1–5 people will die from cirrhosis or liver cancer
Tests
Can a person have normal liver enzyme (e.g., ALT) results and still have Hepatitis C?
Yes. It is common for persons with chronic Hepatitis C to have a liver enzyme level that goes up and down, with periodic returns to normal or near normal. Some infected persons have liver enzyme levels that are normal for over a year even though they have chronic liver disease. If the liver enzyme level is normal, persons should have their enzyme level re-checked several times over a 6–12 month period. If the liver enzyme level remains normal, the doctor may check it less frequently, such as once a year.
Who should get tested for Hepatitis C?
Talk to your doctor about being tested for Hepatitis C if any of the following are true:
- You were born from 1945 through 1965
- You are a current or former injection drug user, even if you injected only one time or many years ago.
- You were treated for a blood clotting problem before 1987.
- You received a blood transfusion or organ transplant before July 1992.
- You are on long-term hemodialysis treatment.
- You have abnormal liver tests or liver disease.
- You work in health care or public safety and were exposed to blood through a needlestick or other sharp object injury.
- You are infected with HIV.
If you are pregnant, should you be tested for Hepatitis C?
No, getting tested for Hepatitis C is not part of routine prenatal care. However, if a pregnant woman has risk factors for Hepatitis C virus infection, she should speak with her doctor about getting tested.
What blood tests are used to test for Hepatitis C?
Several different blood tests are used to test for Hepatitis C. A doctor may order just one or a combination of these tests. Typically, a person will first get a screening test that will show whether he or she has developed antibodies to the Hepatitis C virus. (An antibody is a substance found in the blood that the body produces in response to a virus.) Having a positive antibody test means that a person was exposed to the virus at some time in his or her life. If the antibody test is positive, a doctor will most likely order a second test to confirm whether the virus is still present in the person's bloodstream.
Treatment
Can acute Hepatitis C be treated?
Yes, acute hepatitis C can be treated. Acute infection can clear on its own without treatment in about 25% of people. If acute hepatitis C is diagnosed, treatment does reduce the risk that acute hepatitis C will become a chronic infection. Acute hepatitis C is treated with the same medications used to treat chronic Hepatitis C. However, the optimal treatment and when it should be started remains uncertain.
Can chronic Hepatitis C be treated?
Yes. There are several medications available to treat chronic Hepatitis C, including new treatments that appear to be more effective and have fewer side effects than previous options. The Food and Drug Administration (FDA) maintains a complete list of approved treatments for Hepatitis C.
Is it possible to get over Hepatitis C?
Yes, approximately 15%–25% of people who get Hepatitis C will clear the virus from their bodies without treatment and will not develop chronic infection. Experts do not fully understand why this happens for some people.
What can a person with chronic Hepatitis C do to take care of his or her liver?
People with chronic Hepatitis C should be monitored regularly by an experienced doctor. They should avoid alcohol because it can cause additional liver damage. They also should check with a health professional before taking any prescription pills, supplements, or over-the-counter medications, as these can potentially damage the liver. If liver damage is present, a person should check with his or her doctor about getting vaccinated against Hepatitis A and Hepatitis B.
Vaccination
Is there a vaccine that can prevent Hepatitis C?
Not yet. Vaccines are available only for Hepatitis A and Hepatitis B. Research into the development of a vaccine is under way.
Hepatitis C and Employment
Should a person infected with the Hepatitis C virus be restricted from working in certain jobs or settings?
CDC's recommendationsfor prevention and control of the Hepatitis C virus infection state that people should not be excluded from work, school, play, child care, or other settings because they have Hepatitis C. There is no evidence that people can get Hepatitis C from food handlers, teachers, or other service providers without blood-to-blood contact.
Hepatitis C and Co-infection with HIV
What is HIV and Hepatitis C virus coinfection?
HIV and Hepatitis C virus coinfection refers to being infected with both HIV and the Hepatitis C virus. Coinfection is more common in persons who inject drugs. In fact, 50%–90% of HIV-infected persons who use injection drugs are also infected with the Hepatitis C virus. To learn more about coinfection, visit http://www.cdc.gov/hiv/resources/factsheets/hepatitis.htm.
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
Research Activities
NIAID supports and conducts research on each of the five known hepatitis viruses—A, B, C, D and E. During the past 60 years, NIAID-supported investigators have been involved in many important breakthroughs in hepatitis research, including the discovery of the hepatitis A and E viruses, the development of one of the first diagnostic tests for hepatitis A, and studies that led to the creation of the hepatitis A vaccine and laid the foundation for advanced development of a hepatitis E vaccine. In addition to basic research to understand the molecular processes of hepatitis infection, our research involves significant focus on the development of new treatments and vaccines to prevent acute and chronic hepatitis infection.
Hepatitis B
Although vaccine-preventable, hepatitis B-induced liver cirrhosis and liver cancer kill about 3,000 people in the United States and roughly 620,000 people worldwide each year. The virus can be spread from mother to child during childbirth; through sex with an infected partner; through contact with the blood of an infected person and by sharing needles, syringes, razors or toothbrushes with an infected person. Co-infection with hepatitis B and HIV is common.
NIAID is working with researchers in academia and the pharmaceutical industry to screen hundreds of new drug compounds for potential antiviral activity against hepatitis B. The goal is to find new treatments that will work alone or in combination with current drugs to reduce or resolve chronic infections. For example, one candidate drug has shown promise in transgenic mice and is now being evaluated in rats.
Hepatitis C
Hepatitis C is primarily spread through contact with the blood of an infected individual, such as through needle-sharing practices of injection drug users, unsafe injection practices in healthcare facilities, mother-to-child transmission during childbirth, and infrequently, through sexual contact with an infected partner. Currently available drugs cure only a proportion of treated individuals, but new drugs in trials may significantly improve treatment success rates. There is no vaccine to prevent hepatitis C.
In March, NIAID-supported researchers began a Phase I/II clinical trial of a promising candidate vaccine to evaluate its safety, tolerability and protective ability against hepatitis C. NIAID is supporting several studies, including research at five Hepatitis C Cooperative Research Centers across the country, that focus on the immune response to infection and how treatment might strengthen this response. Additionally, NIAID researchers have conducted preclinical work on several candidate antivirals targeting hepatitis C and are developing biomarkers for predicting progression to hepatitis C-associated liver cancer and HIV co-infection
Hepatitis E
Spread via contact with contaminated water or food, hepatitis E is rare in the United States but prevalent in south and central Asia, sub-Saharan Africa and the Middle East
Studies have found that in certain regions, when pregnant women are infected with hepatitis E virus during the second or third trimester, their babies are at increased risk of poor health and birth defects. NIAID-funded researchers are testing the hypothesis that mothers with micronutrient deficiencies are more likely to experience this effect and what potentially could be done to prevent it. Other NIAID-supported scientists are studying whether hepatitis E virus can become reactivated after a bout of acute disease. Successful trials of hepatitis E vaccines have also taken place, but none have yet been licensed for use in the United States. In 2012, NIAID co-hosted a research workshop, “Hepatitis E in the United States,” with the goal of increasing awareness of the virus among clinicians.
SOURCE: NIAID, NIH
CONDITION: Hepatitis D

Hepatitis D is a viral infection that damages the liver, but it can propagate only when the hepatitis B virus is also present. Approximately 15 million people worldwide are infected with hepatitis D.
Causes
Hepatitis D is caused by the hepatitis D virus, which is found in certain body fluids of infected people. However, hepatitis D virus remains in the body only if the hepatitis B virus is also present.
Transmission
Hepatitis D can be found in the blood, semen, vaginal fluids, and other body fluids of people who are infected. Transmission happens when infected body fluid enters another person’s body. The hepatitis D virus will remain in the body only if hepatitis B virus is also present.
Hepatitis D virus is most commonly transmitted in the same ways as hepatitis B.
- Sex with an infected partner
- Contact with the blood of an infected person
- Sharing of needles, syringes, razors, or toothbrushes with an infected person
- Mother-to-child transmission during childbirth
There are two types of hepatitis D infection:
- Co-infection, in which a person is infected with hepatitis D and hepatitis B at the same time
- Superinfection, in which a person who is already infected with chronic hepatitis B is then infected with hepatitis D
Hepatitis D is not transmitted through shaking hands, coughing, sneezing, breastfeeding, or sharing cups and utensils

Symptoms
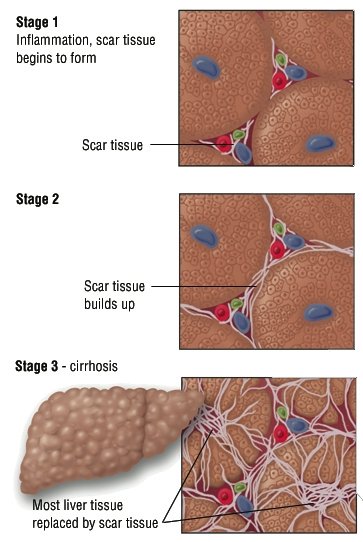
Symptoms include the following:
- Jaundice
- Fatigue
- Abdominal pain
- Nausea or vomiting
- Fever
- Loss of appetite
- Dark urine
- Joint pain
Diagnosis
Healthcare providers review symptoms and can diagnose hepatitis D with a blood test, which will reveal the presence of antibodies to the hepatitis D virus.
Treatment
The acute form of the hepatitis D virus is more likely to disappear on its own in co-infection cases, when a person gets infected with hepatitis B and hepatitis D at the same time. Fewer than 5 percent of people co-infected will develop chronic hepatitis D.
In superinfection cases, in which a person with chronic hepatitis B then gets hepatitis D, up to 80 percent of people will develop chronic hepatitis D. These cases may result in severe chronic hepatitis D that often progress to cirrhosis (end-stage liver disease) or cancer of the liver.
The drug interferon may be helpful in treating disease conditions in some patients.
Prevention
Because hepatitis D needs hepatitis B to propagate, the best way you can prevent hepatitis D infection is to be vaccinated against hepatitis B.
However, there is no vaccine to prevent those who already have developed chronic hepatitis B from getting hepatitis D. The best course of action for hepatitis B carriers is to avoid the high-risk behaviors associated with hepatitis D superinfection, including:
- Sex with an infected partner
- Contact with the blood of an infected person
- Sharing of needles, syringes, razors, or toothbrushes with an infected person
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
SOURCE: NIAID, NIH
CONDITION: Hepatitis E

PROPERTIES
Calicivirus-like virions
unenveloped RNA virus, 32-34nm in diameter
+ve stranded RNA genome, 7.6 kb in size.
very labile and sensitive
not yet cultured
Hepatitis E is a contagious, acute inflammatory disease of the liver. It does not develop into a chronic disease.
Causes
Hepatitis E is caused by the hepatitis E virus, which is found in the stool of an infected person.

Transmission
Transmission of the hepatitis E virus generally happens when someone drinks water that is contaminated with the fecal matter—even just microscopic traces—of an infected person. Major outbreaks typically happen in regions of the world where sanitation is poor.
Few cases of hepatitis E have resulted from person-to-person contact, and there is no evidence that the virus can be spread through sexual activity. Transmission through blood is rare.
Symptoms
Not all people infected with hepatitis E will show symptoms. However, 3 to 8 weeks after getting infected, those who do have symptoms may have the following:
- Jaundice
- Fatigue
- Abdominal pain
- Nausea or vomiting
- Diarrhea
- Fever
- Loss of appetite
- Dark urine
Diagnosis
Healthcare providers review symptoms and can diagnose hepatitis E with a blood test, which will reveal the presence of antibodies to the hepatitis E virus. However, the test is not available in the United States.
Treatment
There are no medicines for treating a hepatitis E infection after a person gets it. In milder cases, healthcare providers usually prescribe rest, plenty of fluids, and a nutritious diet. While the body fights hepatitis E, a person should avoid any medicines—over-the-counter or prescribed—that could damage the liver. Sufferers should also avoid alcohol during the recovery period, as alcohol may also damage the liver.
Prevention
The best way to prevent a hepatitis E infection is to avoid contaminated water, especially when traveling in countries where hepatitis E is common.
Currently, there is no approved vaccine for hepatitis E, though a promising candidate developed in part by the National Institute of Allergy and Infectious Diseases has been successful in clinical trials
Research Activities
NIAID supports and conducts research on each of the five known hepatitis viruses—A, B, C, D and E. During the past 60 years, NIAID-supported investigators have been involved in many important breakthroughs in hepatitis research, including the discovery of the hepatitis A and E viruses, the development of one of the first diagnostic tests for hepatitis A, and studies that led to the creation of the hepatitis A vaccine and laid the foundation for advanced development of a hepatitis E vaccine. In addition to basic research to understand the molecular processes of hepatitis infection, our research involves significant focus on the development of new treatments and vaccines to prevent acute and chronic hepatitis infection.
Hepatitis B
Although vaccine-preventable, hepatitis B-induced liver cirrhosis and liver cancer kill about 3,000 people in the United States and roughly 620,000 people worldwide each year. The virus can be spread from mother to child during childbirth; through sex with an infected partner; through contact with the blood of an infected person and by sharing needles, syringes, razors or toothbrushes with an infected person. Co-infection with hepatitis B and HIV is common.
NIAID is working with researchers in academia and the pharmaceutical industry to screen hundreds of new drug compounds for potential antiviral activity against hepatitis B. The goal is to find new treatments that will work alone or in combination with current drugs to reduce or resolve chronic infections. For example, one candidate drug has shown promise in transgenic mice and is now being evaluated in rats.
Hepatitis C
Hepatitis C is primarily spread through contact with the blood of an infected individual, such as through needle-sharing practices of injection drug users, unsafe injection practices in healthcare facilities, mother-to-child transmission during childbirth, and infrequently, through sexual contact with an infected partner. Currently available drugs cure only a proportion of treated individuals, but new drugs in trials may significantly improve treatment success rates. There is no vaccine to prevent hepatitis C.
In March, NIAID-supported researchers began a Phase I/II clinical trial of a promising candidate vaccine to evaluate its safety, tolerability and protective ability against hepatitis C. NIAID is supporting several studies, including research at five Hepatitis C Cooperative Research Centers across the country, that focus on the immune response to infection and how treatment might strengthen this response. Additionally, NIAID researchers have conducted preclinical work on several candidate antivirals targeting hepatitis C and are developing biomarkers for predicting progression to hepatitis C-associated liver cancer and HIV co-infection.
Hepatitis E
Spread via contact with contaminated water or food, hepatitis E is rare in the United States but prevalent in south and central Asia, sub-Saharan Africa and the Middle East.
Studies have found that in certain regions, when pregnant women are infected with hepatitis E virus during the second or third trimester, their babies are at increased risk of poor health and birth defects. NIAID-funded researchers are testing the hypothesis that mothers with micronutrient deficiencies are more likely to experience this effect and what potentially could be done to prevent it. Other NIAID-supported scientists are studying whether hepatitis E virus can become reactivated after a bout of acute disease. Successful trials of hepatitis E vaccines have also taken place, but none have yet been licensed for use in the United States. In 2012, NIAID co-hosted a research workshop, “Hepatitis E in the United States,” with the goal of increasing awareness of the virus among clinicians.
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
Source: NIAID, NIH
CONDITION: HIV/AIDS

HIV/AIDS : The Basics

Key Points
- HIV is the virus that causes HIV infection. AIDS is the most advanced stage of HIV infection.
- HIV is spread through contact with the blood, semen, pre-seminal fluid, rectal fluids, vaginal fluids, or breast milk of a person infected with HIV. In the United States, HIV is spread mainly by having anal or vaginal sex or sharing drug injection equipment with a person infected with HIV.
- The use of HIV medicines to treat HIV infection is called antiretroviral therapy (ART). ART involves taking a combination of HIV medicines (called an HIV regimen) every day.
- ART can’t cure HIV infection, but it can help people infected with HIV live longer, healthier lives. HIV medicines can also reduce the risk of transmission of HIV.
What is HIV/AIDS?

HIV stands for human immunodeficiency virus, which is the virus that causes HIV infection. The abbreviation “HIV” can refer to the virus or to HIV infection.
AIDS stands for acquired immunodeficiency syndrome. AIDS is the most advanced stage of HIV infection.
HIV attacks and destroys the infection-fighting CD4 cells of the immune system. The loss of CD4 cells makes it difficult for the body to fight infections and certain cancers. Without treatment, HIV can gradually destroy the immune system and advance to AIDS.

How is HIV spread?
HIV is spread through contact with certain body fluids from a person infected with HIV. These body fluids include:
- Blood
- Semen
- Pre-seminal fluid
- Vaginal fluids
- Rectal fluids
- Breast milk

The spread of HIV from person to person is called HIV transmission. The spread of HIV from an HIV-infected woman to her child during pregnancy, childbirth, or breastfeeding is called mother-to-child transmission of HIV.
In the United States, HIV is spread mainly by having sex with or sharing drug injection equipment with someone who is infected with HIV. To reduce your risk of HIV infection, use condoms correctly and consistently during sex, limit your number of sexual partners, and never share drug injection equipment.
Mother-to-child transmission is the most common way that children become infected with HIV. HIV medicines, given to HIV-infected women during pregnancy and childbirth and to their babies after birth, reduce the risk of mother-to-child transmission of HIV.
You can’t get HIV by shaking hands or hugging a person infected with HIV. You also can’t get HIV from contact with objects such as dishes, toilet seats, or doorknobs used by a person with HIV. HIV does not spread through the air or through mosquito, tick, or other insect bites.
What is the treatment for HIV?

The use of HIV medicines to treat HIV infection is called antiretroviral therapy (ART). ART involves taking a combination of HIV medicines (called an HIV regimen) every day. (HIV medicines are often called antiretrovirals or ARVs.)
ART prevents HIV from multiplying and reduces the amount of HIV in the body. Having less HIV in the body protects the immune system and prevents HIV infection from advancing to AIDS.
ART can’t cure HIV, but it can help people infected with HIV live longer, healthier lives. ART also reduces the risk of HIV transmission.
What are the symptoms of HIV/AIDS?
Soon after infection with HIV, some people have flu-like symptoms, such as fever, headache, or rash. The symptoms may come and go for a month or two after infection.
After this earliest stage of HIV infection, HIV continues to multiply but at very low levels. More severe symptoms of HIV infection, such as chronic diarrhea, rapid weight loss, and signs of opportunistic infections, generally don’t appear for many years. (Opportunistic infections are infections and infection-related cancers that occur more frequently or are more severe in people with weakened immune systems than in people with healthy immune systems.)
Without treatment, HIV can advance to AIDS. The time it takes for HIV to advance to AIDS varies, but it can take 10 years or more.
HIV transmission is possible at any stage of HIV infection—even if an HIV-infected person has no symptoms of HIV.
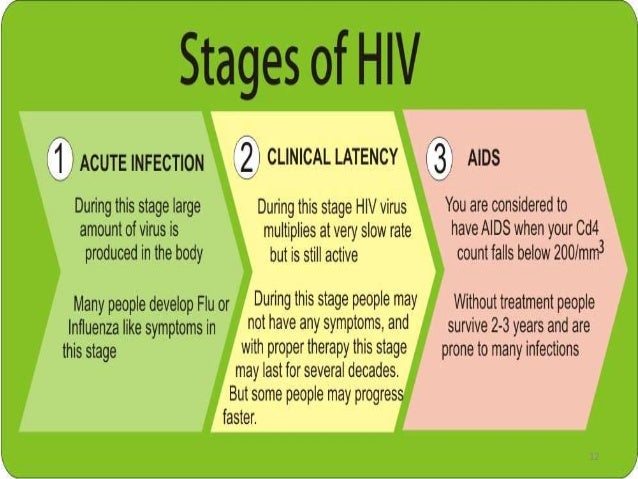
How is AIDS diagnosed?
The following criteria are used to determine if a person infected with HIV has AIDS:
- The person’s immune system is severely damaged, as indicated by a CD4 count of less than 200 cells/mm3. A CD4 count measures the number of CD4 cells in a sample of blood. The CD4 count of a healthy person ranges from 500 to 1,600 cells/mm3.
AND/OR
- The person has one or more opportunistic infections.
Where can I learn more about HIV/AIDS?
- How Do You Get HIV or AIDS? from AIDS.gov
- HIV 101 from the Centers for Disease Control and Prevention (CDC)
This fact sheet is based on information from the following sources:
- From CDC:
HIV Basics
- From the National Institute of Allergy and Infectious Diseases (NIAID):
HIV/AIDS
Source: AIDSInfo.Gov
HIV/AIDS at a Glance
- HIV is the infection that causes AIDS.
- HIV has few or no symptoms for up to 10 years or more before symptoms of AIDS develop.
- There is no cure for HIV/AIDS, but treatment is available.
- HIV can be spread during sex play.
- Latex and female condoms offer very good protection against HIV.
Want to get tested for HIV?Find a Health Center
We all want to protect ourselves and each other from infections like HIV. Learning more about HIV/AIDS is an important first step.
Here are some of the most common questions we hear people ask about HIV/AIDS. We hope you find the answers helpful, whether you think you may have HIV/AIDS, have been diagnosed with it, know someone who has it, or are just curious about it.
What Is HIV/AIDS?
You may have heard about HIV and AIDS, but many people don't know the basic facts about them.
HIV causes AIDS. HIV stands for human immunodeficiency virus. It breaks down the immune system — our body's protection against disease. HIV causes people to become sick with infections that normally wouldn't affect them.
AIDS is short for acquired immune deficiency syndrome. It is the most advanced stage of HIV disease.
In the United States, more than 980,000 cases of AIDS have been reported to the government. About 40,000 women and men in the United States get HIV each year.
What Are the Symptoms of HIV?
Some people develop HIV symptoms shortly after being infected. But it usually takes more than 10 years.
There are several stages of HIV disease. The first HIV symptoms may include swollen glands in the throat, armpit, or groin. Other early HIV symptoms include slight fever, headaches, fatigue, and muscle aches. These symptoms may last for only a few weeks. Then there are usually no HIV symptoms for many years. That is why it can be hard to know if you have HIV.
What Are the Symptoms of AIDS?
AIDS symptoms appear in the most advanced stage of HIV disease. In addition to a badly damaged immune system, a person with AIDS may also have
- thrush — a thick, whitish coating of the tongue or mouth that is caused by a yeast infection and sometimes accompanied by a sore throat
- severe or recurring vaginal yeast infections
- chronic pelvic inflammatory disease
- severe and frequent infections
- periods of extreme and unexplained tiredness that may be combined with headaches, lightheadedness, and/or dizziness
- quick loss of more than 10 pounds of weight that is not due to increased physical exercise or dieting
- bruising more easily than normal
- long periods of frequent diarrhea
- frequent fevers and/or night sweats
- swelling or hardening of glands located in the throat, armpit, or groin
- periods of persistent, deep, dry coughing
- increasing shortness of breath
- the appearance of discolored or purplish growths on the skin or inside the mouth
- unexplained bleeding from growths on the skin, from the mouth, nose, anus, or vagina, or from any opening in the body
- frequent or unusual skin rashes
- severe numbness or pain in the hands or feet, the loss of muscle control and reflex, paralysis, or loss of muscular strength
- confusion, personality change, or decreased mental abilities
How Can I Know If I Have HIV?
You cannot know for sure if you have HIV until you get tested. About 1 out of 6 people with HIV don't know they are infected, so testing is very important. Read more about HIV testing.
Is There a Cure for HIV/AIDS?
There is currently no cure for HIV/AIDS. But there are treatments for people living with HIV/AIDS.
If you have HIV/AIDS, you can take combinations of medicines called "cocktails." The drug cocktails are designed to strengthen the immune system to keep HIV from developing into AIDS or to relieve AIDS symptoms. These drugs are often very expensive, may have serious and very uncomfortable side effects, and may not be available to everyone. They only work for some people and may only work for limited periods of time.
But thanks to "cocktails" for the immune system and improved therapies for the symptoms of AIDS, people are now able to live with HIV/AIDS for many years. New treatments and research may help people live even longer.
How Is HIV Spread?
People have lots of questions about the ways you can get HIV. HIV is transmitted in blood, semen, vaginal fluids, and breast milk. The most common ways HIV is spread are by
- having vaginal or anal intercourse without a condom with someone who has HIV/AIDS
- sharing needles or syringes with someone who has HIV/AIDS
- being deeply punctured with a needle or surgical instrument contaminated with HIV
- getting HIV-infected blood, semen, or vaginal secretions into open wounds or sores
Babies born to women with HIV/AIDS can get HIV from their mothers during birth or from breastfeeding.
HIV is not transmitted by simple casual contact such as kissing, sharing drinking glasses, or hugging.
|
Getting and Giving Blood
Some people are concerned about the risk of HIV when getting or giving blood. Hospitals, blood banks, and health care providers in the United States are extremely careful. Syringes and needles are only used once. And blood is always tested before it's banked. So, today, there is practically no risk of getting or spreading HIV by giving or receiving blood.
|
How Can I Prevent Getting or Spreading HIV?
There are many ways you can protect yourself from HIV. The surest way is to abstain from sexual intercourse and from sharing needles and "works" if you use steroids, hormones, or other drugs.
Many people have been infected with HIV by sharing needles. If you are using needles for steroids, hormones, or other drugs
- Never share needles.
- Get into a needle-exchange program.
- Be sure to disinfect the needles you use.
Don't share personal items that may have blood on them. This includes toothbrushes, razors, needles for piercing or tattooing, and blades for cutting or scarring.
If you choose to have sex, have safer sex to reduce the risk of exchanging blood, semen, or vaginal fluids with your sex partner(s).
Safer Sex and HIV
Some kinds of sex play are "safer" because they have lower risk of infection than others. "Safer-sex" activities are those we choose to lower our risk of exchanging blood, semen, or vaginal fluids — the body fluids most likely to spread HIV. Each of us must decide what risks we will take for sexual pleasure.
Here are some common sexual behaviors grouped according to risk.
VERY LOW RISK — No reported HIV infections due to these behaviors
- fantasy, cyber sex, or phone sex
- using clean sex toys
- masturbation or mutual masturbation
- manual stimulation of one another
- touching or massage
- fondling or body rubbing
- kissing
- oral sex on a man with a condom
- oral sex on a woman with a Glyde dam or plastic wrap
LOW RISK — Very few reported HIV infections due to these behaviors
- deep kissing that causes bleeding
- vaginal intercourse with a condom or female condom
- anal intercourse with a condom or female condom
- oral sex
(Try not to get semen, vaginal fluids, or blood into the mouth or on broken skin.)
HIGH RISK — Millions of reported HIV infections due to these behaviors
- vaginal intercourse without a condom
- anal intercourse without a condom
Talk with your health care provider about testing and treatment for STDs. Women and men with open sores from herpes and other infections get HIV more easily than other people.
Where Can I Get a Test for HIV?
Tests are available from Planned Parenthood health centers and most physicians, hospitals, and health clinics. Local, state, and federal health departments offer free testing. You can also buy an HIV home test kit.
Read more about HIV testing.
Should I be tested?
HIV tests are a normal part of health care. If you think you may have been exposed to HIV, talk with a health care provider about testing. Talking about what risks you've taken can help you decide whether testing is right for you.
Want to get tested for HIV? Find a Health Center
What If I Have HIV/AIDS?
- Consult a health care provider who has experience treating HIV/AIDS.
- Inform sex partner(s) who may also be infected.
- Protect your sex partner(s) from HIV by following safer sex guidelines.
- Do not share needles or "works."
- Get psychological support with a therapist and/or join a support group for people with HIV/AIDS.
- Get information and social and legal support from an HIV/AIDS service organization.
- Don't share your HIV status with people who do not need to know. People with HIV may still face discrimination. Only tell people you can count on for support.
Maintain a strong immune system with regular medical checkups and a healthy lifestyle:
- Eat well.
- Get enough rest and exercise.
- Avoid illegal or recreational drugs, including alcohol and tobacco.
- Learn how to manage stress effectively.
Consider using medicines that may slow the progress of the infection.
What If I Have HIV/AIDS and I'm Pregnant?
If you have HIV and are pregnant, consult a health care provider who knows about HIV disease. Without treatment, about 25 out of 100 babies born to women with HIV are also infected. However, the use of HIV medicines, cesarean delivery, and refraining from breastfeeding can reduce the risk of transmission to less than 2 out of 100.
What's PrEP and how does it prevent HIV?
PrEP (Pre-Exposure Prophylaxis) is a way to help prevent HIV by taking a pill every day. It reduces your risk of getting infected. When PrEP is combined with condoms and other prevention methods it works even better. PrEP may not work if you skip doses. Even if used correctly, there's no guarantee that PrEP will work.
PrEP is only used for people who are at very high risk for HIV through sex or IV drug use. PrEP might be right for you if
- your partner is HIV-positive
- your partner is HIV-negative and either you or your partner has sex with someone whose HIV status isn't known
- you're a gay or bisexual man who has had anal sex without a condom or been told you have an STD in the past 6 months
- you're a heterosexual man or woman who doesn't use condoms every time you have sex with people who inject drugs or have bisexual male partners
- you have injected drugs in the past 6 months and have shared needles or been in drug treatment for IV drug use in the past 6 months.
Talk with your doctor or nurse about whether or not PrEP might be good for you. They can tell you more about how it works and what you can expect while taking it.
What's PEP and how does it prevent HIV?
PEP (Post Exposure Prophylaxis) is a way to prevent HIV after being exposed to it. With PEP, you take anti-HIV medicines as soon as possible after you may have been exposed to HIV to try to reduce your chance of becoming HIV positive. This could happen because of a sexual assault, or having unprotected sex with someone who has HIV, or sharing needles with someone who has HIV.
One or more medicines are taken several times a day for at least 28 days. The medicines work by keeping HIV from spreading through your body. Even if taken correctly, there's no guarantee that taking PEP will work.
It should only be used rarely, right after a possible exposure. Your doctor or nurse will help decide if PEP is right for you, depending on what happened, when it happened, and what you know about the HIV status of the person whose blood or body fluids you were exposed to.
Where Can I Learn More About HIV/AIDS?
Call the toll-free CDC-INFO hotline for information about HIV/AIDS in English and Spanish:
1-800-CDC-INFO (232-4636)
TTY: 1-888-232-6348
For more information, visit: https://aidsinfo.nih.gov
Source: AIDSinfo, NIH
CONDITION: Pelvic Inflammatory Disease (PID)

Key Facts
PID is a serious infection usually caused by sexually transmitted infections. It can cause problems including chronic pain and difficulty getting pregnant (infertility). It’s important to lessen your chance of STIs by not having sex, always using condoms if you do have sex, and getting screened for STIs by your health care provider.
What is PID?
PID is an infection of the female reproductive organs (the fallopian tubes, uterus, ovaries, vagina, and cervix). It’s usually caused by a STI.
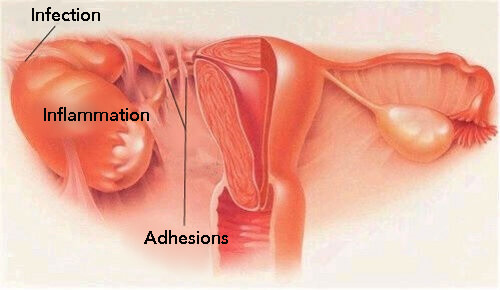
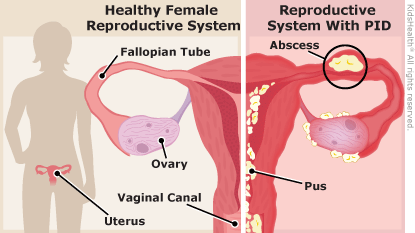
Who gets PID?
Any woman can get PID, but women who have multiple sexual partners and practice unsafe sex are most likely to get an STI that could cause PID.
How does someone get PID?
PID usually begins with an infection of the vagina and cervix (the opening to the uterus), caused by an STI such as gonorrhea or chlamydia. If the infections of the vagina and cervix aren’t treated with antibiotics, they can spread to the endometrium (lining of the uterus), and then to the fallopian tubes, ovaries, and abdomen.
PID rarely occurs after having certain surgical procedures, such as an abortion, or after treatment for an abnormal Pap test.
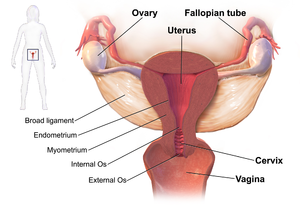
What are the symptoms of PID?
A woman with PID may not always have symptoms. If she does, she’ll likely feel pain in her lower abdomen (belly) area.
Symptoms of PID can include:
- Lower abdominal pain and/or lower back pain
- Longer and/or heavier menstrual periods
- Cramps or spotting throughout the month
- Unusual vaginal discharge (change in smell, color, or amount)
- Fever
- Vomiting, nausea
- Pain during sex and/or with a pelvic exam by your health care provider
- Pain or burning when passing urine
If you notice any symptoms of PID, you should call or see your health care provider right away. If you have a high fever or severe pain, go to the closest emergency room. The infection can get worse and cause more pain and damage to your reproductive organs in just a day or two.
How is PID diagnosed?
Your health care provider can likely tell if you have PID based on your symptoms, a pelvic exam, and blood tests. You may have tenderness when your health care provider moves your cervix or examines your ovaries or uterus. Sometimes an ultrasound (a test that uses soundwaves without radiation) is used to look inside at your reproductive organs to see if there’s any sign of an abscess or other condition. Occasionally, a laparoscopy (a minor surgery to look at your reproductive organs) will be needed if you’re not getting better.
How is PID treated?
Depending on how sick you are, you may be treated either in a hospital or as an outpatient (just going to your health care provider’s office for an appointment). If your health care provider feels you need to stay in the hospital, you’ll receive antibiotics through an IV (through your veins) and by mouth (a pill) until you feel better. After leaving the hospital, you’ll have to take antibiotics by mouth for a total of 2 weeks.
If you’re treated as an outpatient, you may receive a shot or pills to start the treatment, and then you have to take antibiotics by mouth for 2 weeks. It’s very important to take all of the pills, even if you start to feel better. If you don’t, you could get sicker. A few days after you start taking medicine, you’ll need to see your health care provider again. If you don’t get better, you may need to have more tests and/or take different medicine.
If you find out you have PID, you need to make sure your partner(s) get(s) tested and treated for gonorrhea and chlamydia. Your partner(s) must be treated for both kinds of STIs no matter what your test results or his/her test results show. Unless your partner is treated at the same time as you, you are likely to get infected again.
Is PID dangerous?
PID can be dangerous if not treated early. Scar tissue can form in the fallopian tubes and inside the abdomen. These scars can block the fallopian tubes, which can cause difficulty getting pregnant or infertility, but this isn’t always the case. If the tubes are partly blocked, fertilized eggs may not reach the uterus and the pregnancy can form in the fallopian tubes (known as a tubal or ectopic pregnancy). Scarring can cause pain that lasts for months or even years. If the effects of PID are very bad, surgery may be needed to treat scar tissue. PID is more likely to come back if you get an STI again. Also, the more times you have PID, the more likely you are to have problems that harm your body.
How can PID be prevented?
To prevent PID, you need to avoid getting an STI.
The best ways to prevent getting an STI are:
- Not having sex (vaginal, anal, and oral)
- Using a latex condom (polyurethane if allergic to latex) correctly every time you have sex
- Limiting the number of sexual partners you have, and making sure all of your partners get treated for STIs
- Not using douches. Douches can spread the bacteria further up the reproductive tract
- Don’t smoke cigarettes.
- Finishing all your antibiotics if you’re being treated for a cervical infection or PID
Remember, if you have any symptoms of an STI or PID, see your health care provider right away. Getting treated early (within 1-2 days) will greatly lower your chances of complications. Make sure you get tested for other STIs such as syphilis and HIV, too.
Source: Young Women’s Health
More on PID Pelvic Inflammatory Disease (PID)
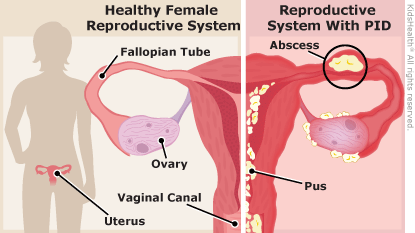
Pelvic inflammatory disease is an infection of a woman's womb (uterus), ovaries, or fallopian tubes.
Causes
Pelvic inflammatory disease (PID) is an infection caused by bacteria. When bacteria from the vagina or cervix travel to your womb, fallopian tubes, or ovaries they can cause an infection.
Most of the time, PID is caused by bacteria from chlamydia and gonorrhea. These are sexually transmitted infections (STIs). Having unprotected sex with someone who has an STI can cause PID.
Bacteria can also enter your body during a medical procedure such as:
- Childbirth
- Endometrial biopsy (removing a small piece of your womb lining to test for cancer)
- Getting an intrauterine device (IUD)
- Miscarriage
- Abortion
In the United States, nearly 1 million women have PID each year. About 1 in 8 sexually active girls will have PID before age 20.
You are more likely to get PID if:
- You have a sex partner with gonorrhea or chlamydia.
- You have sex with many different people.
- You have had an STI in the past.
- You have recently had PID.
- You have recently gotten an IUD.
- You have had sex before age 20.
Symptoms
Common symptoms of PID include:
- Fever
- Pain or tenderness in the pelvis, lower belly, or lower back
- Fluid from your vagina that has an unusual color, texture, or smell
Other symptoms that may occur with PID:
- Bleeding after intercourse
- Chills
- Being very tired
- Pain when you urinate
- Having to urinate often
- Period cramps that hurt more than usual or last longer than usual
- Unusual bleeding or spotting during your period
- Not feeling hungry
- Nausea and vomiting
- Skipping your period
- Pain when you have intercourse
You can have PID and not have any symptoms. For example, chlamydia can cause PID with no symptoms. Women who have an ectopic pregnancy or who are infertile often have PID caused by chlamydia. An ectopic pregnancy is when an egg grows outside of the uterus. It puts the mother's life in danger.
Exams and Tests
Your health care provider may do a pelvic exam to look for:
- Bleeding from your cervix. The cervix is the opening to your uterus.
- Fluid coming out of your cervix.
- Pain when your cervix is touched.
- Tenderness in your uterus, tubes, or ovaries.
You may have lab tests to check for signs of infection:
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- WBC count
Other tests include:
- A swab taken of your vagina or cervix. This sample will be checked for gonorrhea, chlamydia, or other causes of PID.
- Pelvic ultrasound or CT scan to see what else may be causing your symptoms. Appendicitis or pockets of infection around your tubes and ovaries may cause similar symptoms.
- Pregnancy test.
Treatment
Your provider will often have you start taking antibiotics while waiting for your test results.
If you have mild PID:
- Your provider will give you a shot containing an antibiotic.
- You will be sent home with antibiotic pills to take for up to 2 weeks.
- You will need to follow-up closely with your provider.
If you have more severe PID:
- You may need to stay in the hospital.
- You may be given antibiotics through a vein (IV).
- Later, you may be given antibiotic pills to take by mouth.
There are many different antibiotics that can treat PID. Some are safe for pregnant women. Which type you take depends on the cause of the infection. You may receive a different treatment if you have gonorrhea or chlamydia.
If your PID is caused by an STI like gonorrhea or chlamydia, your sexual partner must be treated as well.
- If you have more than 1 sexual partner, they must all be treated.
- If your partner is not treated, he or she can infect you again, or can infect other people in the future.
- Both you and your partner must finish taking all of the prescribed antibiotics.
- Use condoms until you both have finished taking antibiotics.
Possible Complications
PID infections can cause scarring of the pelvic organs. This can lead to:
- Chronic pelvic pain
- Ectopic pregnancy
- Infertility
- Tuboovarian abscess
If you have a serious infection that does not improve with antibiotics, you may need surgery.
When to Contact a Medical Professional
Call your provider if:
- You have symptoms of PID.
- You think you have been exposed to an STI.
- Treatment for a current STI does not seem to be working.
Prevention
Get prompt treatment for STIs.
You can prevent PID by practicing safe sex.
- The only absolute way to prevent an STI is to not have sex (abstinence).
- You can reduce your risk by having a sexual relationship with only 1 person. This is called being monogamous.
- Your risk will also be reduced if you and your sexual partners get tested for STIs before starting a sexual relationship.
- Using a condom every time you have sex also reduces your risk.
Here is how you can reduce your risk of PID:
- Get regular STI screening tests.
- If you are a new couple, get tested before starting to have sex. Testing can detect infections that are not causing symptoms.
- If you are a sexually active woman age 24 or younger, get screened each year for chlamydia and gonorrhea.
- All women with new sexual partners or multiple partners should also be screened.
Alternative Names
PID; Oophoritis; Salpingitis; Salpingo-oophoritis; Salpingo-peritonitis
Source: MedlinePlus, NLM, NIH
CDC: Pelvic Inflammatory Disease (PID)
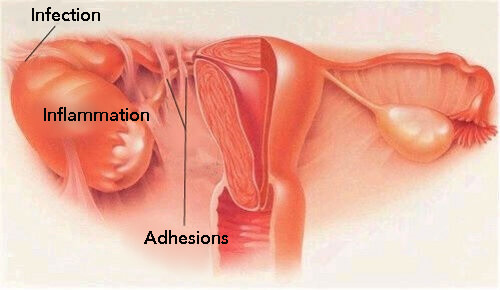
What happens if I don't get treated?
BV can cause some serious health risks, including
- Increasing your chance of getting HIV if you have sex with someone who is infected with HIV;
- If you are HIV positive, increasing your chance of passing HIV to your sex partner;
- Making it more likely that you will deliver your baby too early if you have BV while pregnant;
- Increasing your chance of getting other STDs, such as chlamydia and gonorrhea. These bacteria can sometimes cause pelvic inflammatory disease (PID), which can make it difficult or impossible for you to have children.
Where can I get more information?
Division of STD Prevention (DSTDP)
Centers for Disease Control and Prevention
www.cdc.gov/std
Order Publication Online at www.cdc.gov/std/pub
CDC-INFO Contact Center
1-800-CDC-INFO (1-800-232-4636)
TTY: (888) 232-6348
Contact CDC-INFO
CDC National Prevention Information Network (NPIN)
P.O. Box 6003
Rockville, MD 20849-6003
E-mail: npin-info@cdc.gov
Sources
Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2010. MMWR 2010;59(No. RR-12)
Hillier S and Holmes K. Bacterial vaginosis. In: K. Holmes, P. Sparling, P. Mardh et al (eds). Sexually Transmitted Diseases, 3rd Edition. New York: McGraw-Hill, 1999, 563-586.
Related Content
- STDs & Pregnancy Fact Sheet
- Pregnancy and HIV, Viral Hepatitis, and STD Prevention
- Pelvic Inflammatory Disease (PID) Fact Sheet
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see the system usage guidelines and disclaimer.
CDC: Centers for Disease Control and Prevention
Vaginal Yeast Infection & Vaginitis


Vaginal yeast infection

Two out of three women who buy yeast infection medicine don't really have a yeast infection. See your doctor or nurse first to make sure you have a yeast infection and not a more serious infection.
Most women will get a vaginal yeast infection at some point in their life. Symptoms of vaginal yeast infections include burning, itching, and thick, white discharge. Yeast infections are easy to treat, but it is important to see your doctor or nurse if you think you have an infection. Yeast infection symptoms are similar to other vaginal infections and sexually transmitted infections (STIs). If you have a more serious infection, and not a yeast infection, it can lead to major health problems.
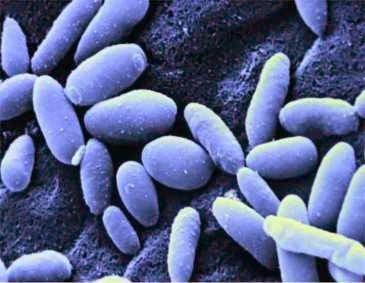
What is a vaginal yeast infection?
A vaginal yeast infection is an infection of the vagina that causes itching and burning of the vulva, the area around the vagina. Vaginal yeast infections are caused by an overgrowth of the fungus Candida.
Vaginal yeast infection

Who gets vaginal yeast infections?
Women and girls of all ages can get vaginal yeast infections. Three out of four women will have a yeast infection at some point in their life. Almost half of women have two or more infections.
Vaginal yeast infections are rare before puberty and after menopause.
Are some women more at risk for yeast infections?
Yes. Your risk for yeast infections is higher if:
- You are pregnant
- You have diabetes and your blood sugar is not under control
- You use a type of hormonal birth control that has higher doses of estrogen
- You douche or use vaginal sprays
- You recently took antibiotics such as amoxicillin or steroid medicines
- You have a weakened immune system, such as from HIV
What are the signs and symptoms of a vaginal yeast infection?
The most common symptom of a vaginal yeast infection is extreme itchiness in and around the vagina.
Other signs and symptoms include:
- Burning, redness, and swelling of the vagina and the vulva
- Pain when urinating
- Pain during sex
- Soreness
- A thick, white vaginal discharge that looks like cottage cheese and does not have a bad smell
You may have only a few of these symptoms. They may be mild or severe.
What causes yeast infections?
Yeast infections are caused by overgrowth of the microscopic fungus Candida.
Your vagina may have small amounts of yeast at any given time without causing any symptoms. But when too much yeast grows, you can get an infection.
Can I get a yeast infection from having sex?
Yes. A yeast infection is not considered an STI, because you can get a yeast infection without having sex. But you can get a yeast infection from your sexual partner. Condoms and dental dams may help prevent getting or passing yeast infections through vaginal, oral, or anal sex.
Should I call my doctor or nurse if I think I have a yeast infection?

Yes. Seeing your doctor or nurse is the only way to know for sure if you have a yeast infection and not a more serious type of infection.
The signs and symptoms of a yeast infection are a lot like symptoms of other more serious infections, such as STIs and bacterial vaginosis (BV). If left untreated, STIs and BV raise your risk of getting other STIs, including HIV, and can lead to problems getting pregnant. BV can also lead to problems during pregnancy, such as premature delivery.
How is a yeast infection diagnosed?
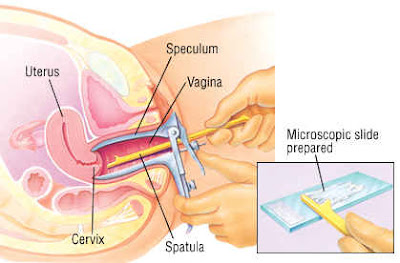
Your doctor will do a pelvic exam to look for swelling and discharge. Your doctor may also use a cotton swab to take a sample of the discharge from your vagina. A lab technician will look at the sample under a microscope to see whether there is an overgrowth of the fungus Candida that causes a yeast infection.
ow is a yeast infection treated?
Yeast infections are usually treated with antifungal medicine. See your doctor or nurse to make sure that you have a vaginal yeast infection and not another type of infection.
You can then buy antifungal medicine for yeast infections at a store, without a prescription. Antifungal medicines come in the form of creams, tablets, ointments, or suppositories that you insert into your vagina. You can apply treatment in one dose or daily for up to seven days, depending on the brand you choose.
Your doctor or nurse can also give you a single dose of antifungal medicine taken by mouth, such as fluconazole . If you get more than four vaginal yeast infections a year, or if your yeast infection doesn't go away after using over-the-counter treatment, you may need to take regular doses of antifungal medicine for up to six months.
Is it safe to use over-the-counter medicines for yeast infections?
Yes, but always talk with your doctor or nurse before treating yourself for a vaginal yeast infection. This is because:
- You may be trying to treat an infection that is not a yeast infection. Studies show that two out of three women who buy yeast infection medicine don't really have a yeast infection. Instead, they may have an STI or bacterial vaginosis (BV). STIs and BV require different treatments than yeast infections and, if left untreated, can cause serious health problems.
- Using treatment when you do not actually have a yeast infection can cause your body to become resistant to the yeast infection medicine. This can make actual yeast infections harder to treat in the future.
- Some yeast infection medicine may weaken condoms and diaphragms, increasing your chance of getting pregnant or an STI when you have sex. Talk to your doctor or nurse about what is best for you, and always read and follow the directions on the medicine carefully.
How do I treat a yeast infection if I'm pregnant?
During pregnancy, it's safe to treat a yeast infection with vaginal creams or suppositories that contain miconazole or clotrimazole.
Do not take the oral fluconazole tablet to treat a yeast infection during pregnancy. It may cause birth defects.
Can I get a yeast infection from breastfeeding?
Yes. Yeast infections can happen on your nipples or in your breast (commonly called "thrush") from breastfeeding. Yeast thrive on milk and moisture. A yeast infection you get while breastfeeding is different from a vaginal yeast infection. However, it is caused by an overgrowth of the same fungus.
Symptoms of thrush during breastfeeding include:
- Sore nipples that last more than a few days, especially after several weeks of pain-free breastfeeding
- Flaky, shiny, itchy, or cracked nipples
- Deep pink and blistered nipples
- Achy breast
- Shooting pain in the breast during or after feedings
If you have any of these signs or symptoms or think your baby might have thrush in his or her mouth, call your doctor. Learn more about thrush in our Breastfeeding section.
If I have a yeast infection, does my sexual partner need to be treated?
Maybe. Yeast infections are not STIs. But it is possible to pass yeast infections to your partner during vaginal, oral, or anal sex.
- If your partner is a man, the risk of infection is low. About 15% of men get an itchy rash on the penis if they have unprotected sex with a woman who has a yeast infection. If this happens to your partner, he should see a doctor. Men who haven't been circumcised and men with diabetes are at higher risk.
- If your partner is a woman, she may be at risk. She should be tested and treated if she has any symptoms.
How can I prevent a yeast infection?
You can take steps to lower your risk of getting yeast infections:
- Do not douche. Douching removes some of the normal bacteria in the vagina that protects you from infection.
- Do not use scented feminine products, including bubble bath, sprays, pads, and tampons.
- Change tampons, pads, and panty liners often.
- Do not wear tight underwear, pantyhose, pants, or jeans. These can increase body heat and moisture in your genital area.
- Wear underwear with a cotton crotch. Cotton underwear helps keep you dry and doesn't hold in warmth and moisture.
- Change out of wet swimsuits and workout clothes as soon as you can.
- After using the bathroom, always wipe from front to back.
- Avoid hot tubs and very hot baths.
- If you have diabetes, be sure your blood sugar is under control.
Does yogurt prevent or treat yeast infections?
Maybe. Studies suggest that eating eight ounces of yogurt with "live cultures" daily or taking Lactobacillus acidophilus capsules can help prevent infection.
But, more research still needs to be done to say for sure if yogurt with Lactobacillus or other probiotics can prevent or treat vaginal yeast infections. If you think you have a yeast infection, see your doctor or nurse to make sure before taking any over-the-counter medicine.
What should I do if I get repeat yeast infections?
If you get four or more yeast infections in a year, talk to your doctor or nurse.
About 5% of women get four or more vaginal yeast infections in one year. This is called recurrent vulvovaginal candidiasis (RVVC). RVVC is more common in women with diabetes or weak immune systems, such as with HIV, but it can also happen in otherwise healthy women.
Doctors most often treat RVVC with antifungal medicine for up to six months. Researchers also are studying the effects of a vaccine to help prevent RVVC.
More information about vaginal yeast infections
For more information on vaginal yeast infections, call the OWH Helpline at 800-994-9662 or contact the following organizations:
- Centers for Disease Control and Prevention (CDC), HHS
Phone Number: 800-232-4636
- National Institute of Allergy and Infectious Diseases (NIAID), NIH, HHS
Phone Number: 866-284-4107 (TDD: 800-877-8339)
- American College of Obstetricians and Gynecologists (ACOG)
Phone Number: 800-673-8444
- Planned Parenthood Federation of America
Phone Number: 800-230-7526
This fact sheet was reviewed by:
Michail S. Lionakis, M.D., Sc.D.,
Clinical Investigator, Chief, Fungal Pathogenesis Unit, Laboratory of Clinical Infectious Diseases, National Institute of Allergy & Infectious Diseases (NIAID), NIH
Lance Edwards, M.D.,
FACOG, Suffolk Obstetrics, Port Jefferson, New York
Source: Office on Women's Health, HHS
Summary of Vaginitis
Vaginitis Overview
Vaginitis is an inflammation of the vagina. It is often caused by infections, some of which are associated with serious diseases. The most common vaginal infections are
- Bacterial Vaginosis
- Trichomoniasis
- Vaginal Yeast Infection
Some vaginal infections are transmitted through sexual contact, but others, such as yeast infections, probably are not.

Micrograph of two epithelial cells, a normal cell, and an epithelial cell covered by bacteria giving the cell a roughened, stippled appearance known as a “clue cell.” Clue cells are a sign of bacterial vaginosis.
Credit: CDC/M. Rein

Other Causes of Vaginitis
Although most vaginal infections in women are due to bacterial vaginosis, trichomoniasis, or yeast, there may be other causes as well. These causes include other sexually transmitted diseases, allergic reactions, and irritations.
Allergic symptoms can be caused by spermicides, vaginal hygiene products, detergents, and fabric softeners. Inflammation of the cervix (opening to the womb) also is associated with abnormal vaginal discharge. Healthcare providers can tell them apart from true vaginal infections by doing lab tests.
Research
To control vaginitis, research is under way to determine the factors that promote the growth and disease-causing potential of vaginal microbes (germs). This information could help improve efforts to treat and prevent vaginitis. Vaginitis is the object of serious studies as scientists try to clarify its role in such conditions as pelvic inflammatory disease and pregnancy-related complications.
Vaginitis refers to disorders of the vagina caused by infection, inflammation, or changes in the normal vaginal flora. Symptoms include vaginal discharge, odor, itching, and/or discomfort. The three most common diseases diagnosed among women with these symptoms include bacterial vaginosis (40–45 percent), vulvovaginal candidiasis (20–25 percent), and trichomoniasis (15–20 percent). In some cases, there may be more than one disease present. Recurrent vaginitis is also common.
Research is under way to determine the factors that promote the growth and disease-causing potential of vaginal microbes and their role in vaginitis. These microbes include the sexually transmitted pathogen Trichomonas vaginalis, Candida species, and microbes associated with bacterial vaginosis, such as Gardnerella vaginalis.
NIAID-supported research has led to advances in knowledge about the normal microflora of the vagina, reproductive behavior of yeast, and the genetic code of T. vaginalis. For example, researchers have discovered an association between certain lactobacilli species in the normal microflora in the vagina and protection from bacterial vaginosis (BV). They are investigating a lactobacillus vaginal suppository aimed to help these beneficial bacteria grow in the vagina. Researchers also are studying the use of combination treatment with vaginal lactobacilli suppositories and oral medication to treat BV and prevent its recurrence.
Other NIAID-funded researchers have sequenced the genome of T. vaginalis. Understanding the genome of this pathogen will help researchers understand how it evolves, spreads, and causes disease. T. vaginalis is particularly interesting to medical researchers because it increases both transmission and acquisition of HIV among women. Additionally, both T. vaginalis? and BV are associated with adverse pregnancy outcomes including preterm birth and low birth weight. Knowledge gained from ongoing research could help improve efforts to treat and prevent vaginitis and also prevent its potential complications.
Vaginal Yeast Infection Summary
Vaginal yeast infection, or vulvovaginal candidiasis, is a common cause of vaginal irritation. Nearly 75 percent of all adult women have had at least one "yeast infection" in their lifetime, according to the Centers for Diseases Control and Prevention.

Micrograph showing Candida albicans from a patient with vaginal candidiasis, also known as moniliasis.?
Credit: CDC/Dr. Stuart Brown
Cause
This infection is caused by an overgrowth of a fungus called Candida albicans in the vagina. Candida is yeast, which is a type of fungus.
Yeast are always present in the vagina in small numbers, and symptoms only appear with overgrowth. Candida can multiply when an imbalance occurs, such as when the normal acidity of the vagina changes or when hormonal balance changes. When that happens, symptoms of candidiasis may appear.
Transmission
Several factors are associated with increased yeast infection in women, including
- Weakened or compromised immune systems
- Pregnancy
- Diabetes
- Long-term use of broad-spectrum antibiotics
- Use of corticosteroid medicines
Wearing tight, poorly ventilated clothing and underwear also can contribute to yeast infections. Women with chronic (recurring) yeast infections should work with their healthcare providers to find out possible underlying causes.
On rare occasions, men can also get genital candidiasis.
Symptoms
The most frequent symptoms of yeast infection in women are itching, burning, and irritation of the vagina. Painful urination and painful intercourse also are common.
Vaginal discharge is not always present and may only be present in small amounts. The thick, whitish-gray discharge is typically described as cottage-cheese-like, although it can vary from watery to thick.
Most male partners of women with yeast infections do not have any symptoms of the infection. Some men, however, have reported temporary rashes and burning sensations of the penis after intercourse if they did not use condoms.
Diagnosis
Because few specific signs and symptoms of yeast infections are usually present, healthcare providers can't diagnose this condition by a person’s medical history and physical examination. They usually diagnose yeast infection by examining vaginal secretions under a microscope for evidence of yeast.
Treatment
Various antifungal vaginal medicines are available to treat yeast infections. Women can buy antifungal creams to be applied directly to the area, tablets to be taken orally, or suppositories for use in the vagina.
Because bacterial vaginosis, trichomoniasis, and yeast infections are difficult to tell apart on the basis of symptoms alone, a woman with vaginal symptoms should see her healthcare provider for an accurate diagnosis before using these products.
For updated information about the treatment for vaginal yeast infections, read the Centers for Disease Control and Prevention Sexually Transmitted Diseases Treatment Guidelines.
Source: NIAID, NIH.
Vaginal Thrush
Introduction

Vaginal thrush is a common yeast infection that affects most women at some point.
It may be unpleasant and uncomfortable, but can usually be treated with medication available from pharmacies or on prescription from your GP.
However, for some women, vaginal thrush can be difficult to treat and keeps coming back.
This page covers:
Symptoms of vaginal thrush
What to do if you have vaginal thrush
How to treat vaginal thrush
What causes vaginal thrush?
Preventing vaginal thrush
Symptoms of vaginal thrush

Typical symptoms of vaginal thrush include:
- itching and soreness around the entrance of the vagina
- vaginal discharge – this is usually odourless and may be thick and white or thin and watery
- pain during sex, which may make you worry about having sex
- a stinging sensation when peeing
Sometimes the skin around the vagina can be red, swollen or cracked. Occasionally there may also be sores on the skin, although this is more often a sign of genital herpes.
You can use the vagina problems visual guide to help find out what could be causing your symptoms.
What to do if you have vaginal thrush
If you've had thrush before and think you have it again, you can normally treat it with medicines bought from a local pharmacy. See How to treat vaginal thrush below for more information.
It's a good idea to get medical advice from your GP or a sexual health clinic if:
- you have thrush for the first time
- you're under the age of 16 or over 60
- you're pregnant or breastfeeding – read more about thrush in pregnancy
- you have unusual symptoms, such as coloured or smelly discharge, or sores on the skin around your vagina
- you have abnormal vaginal bleeding or pain in your lower tummy
- you've had two episodes of thrush within the last six months
- you've reacted badly to antifungal treatment in the past, or it didn't work
- you or your partner have previously had a sexually transmitted infection (STI) and you think it might have returned
- your symptoms don't improve after 7-14 days of treatment
Thrush isn't usually anything to worry about in these cases, but your doctor may want to take a swab from your vagina to confirm the diagnosis and/or carry out tests to check for any underlying cause.
They can also advise you about the most suitable treatment and give you a prescription, if necessary.
How to treat vaginal thrush
Mild thrush can usually be treated with a short course of antifungal medication. The symptoms will usually clear up within a week or two.
Treatment may need to be continued for longer if you have repeated bouts of thrush.
Several thrush medicines can be bought over the counter from pharmacies, while others are only available on prescription from your GP.
The main types are:
- pessaries – a special pill that you insert into your vagina using a special applicator
- intravaginal creams – these are also placed into the vagina using an applicator
- capsules –these are swallowed and may be more convenient to use than pessaries or intravaginal cream, but can have more troublesome side effects, such as vomiting or an upset stomach
These treatments are all equally effective. You can usually choose the treatment you prefer, although pregnant or breastfeeding women shouldn't take the capsules.
You can also get creams to apply to the skin surrounding the entrance of your vagina. These can help relieve itchiness and soreness, although you may find that an ordinary emollient (moisturiser) works just as well.
Read more about treating vaginal thrush.
What causes vaginal thrush?
Vaginal thrush is caused by yeasts from a group of fungi called Candida.
Many women have Candida in their vagina without it causing any problems, but thrush can develop if the natural balance of micro-organisms in the vagina is disrupted and Candida multiplies.
You're more likely to get thrush if you:
- are in your twenties and thirties – thrush is less common in girls who haven't started their periods and women who have been through the menopause
- are pregnant
- have sex when you're not fully aroused or you're worried it may hurt – this can lead to vaginal dryness and tightness during sex, which can trigger thrush
- take antibiotics
- have poorly controlled diabetes
- have a weakened immune system – for example, because of a condition such as HIV or a treatment such as chemotherapy
Vaginal thrush isn't classed as an STI, but it can be triggered by sex – particularly if you have trouble relaxing and your vagina is dry – and can occasionally be passed on to sexual partners.
Preventing vaginal thrush
If you get thrush frequently, you can:
- use water and an emollient (moisturiser) soap substitute to clean the skin around your vagina, but avoid cleaning this area more than once a day
- apply a greasier moisturiser to the skin around your vagina several times a day to protect it (but be aware that these moisturisers can weaken condoms)
- avoid potential irritants in perfumed soaps, shower gels, vaginal deodorants, wipes and douches
- avoid wearing tight-fitting underwear or tights – some women find that special silk underwear designed for people with eczema and thrush is helpful
- ensure your blood sugar level is kept under control, if you have diabetes
Some women eat probiotic yoghurt or supplements to prevent vaginal thrush, but there's little evidence to suggest this works.
Treatment for vaginal thrush

Source: Top10HomeRemedies
Vaginal thrush is treated with medications you can buy over the counter from a pharmacy, or get on prescription from your GP.
If you've had thrush before and think you have it again, you can normally treat it with medication bought from a local pharmacy. Otherwise, you should see your GP for advice.
Find your local pharmacy.
Read about when to get medical advice for vaginal thrush.
Thrush medications
Thrush is treated with antifungal medicines that are available as pessaries, intravaginal creams or capsules.
All these medications are equally effective, but you may find that one is more convenient to use than another.
Pessaries and intravaginal creams
A pessary is a pill that you insert into your vagina using a special applicator. Intravaginal creams are applied inside your vagina.
The main types used to treat thrush are:
- clotrimazole – available over the counter from pharmacies
- econazole, miconazole and fenticonazole – available on prescription
Over-the-counter pessaries are usually used daily for one to six days. Intravaginal cream is normally used once. Possible side effects include a mild burning sensation, slight redness or itching.
These treatments can also damage latex condoms and diaphragms, so you may want to avoid having sex, or use another form of contraception during treatment and for up to five days afterwards.
Capsules
If you would prefer not to use pessaries or intravaginal cream, antifungal capsules are available.
The main types used to treat thrush are:
- fluconazole – available over the counter from pharmacies
- itraconazole –available on prescription
Over-the-counter thrush capsules usually come as a single dose.
Possible side effects can include feeling sick, an upset stomach, diarrhoea and headaches.
Skin creams
If the skin around the entrance to your vagina is also sore or itchy, you may find it helpful to use an antifungal skin cream in addition to one of the treatments above.
- Creams containing clotrimazole can be bought over the counter from pharmacies.
- They're available in packs that also include antifungal pessaries, intravaginal cream or capsules.
- They're normally applied to the skin two or three times a day for at least two weeks.
- Possible side effects include irritation, a stinging sensation or itching.
Alternatively, you could try using an ordinary emollient (moisturiser) near your vagina. This can help relieve your symptoms and causes fewer side effects than antifungal cream.
Emollients and antifungal skin cream can weaken latex condoms and diaphragms, so you may want to avoid having sex, or use another form of contraception during treatment and for up to five days afterwards.
Sex and sexual partners
Vaginal thrush isn't classed as a sexually transmitted infection (STI), so sexual partners don't need to be informed, tested or treated if they don't have any symptoms.
However, there's a very small risk of passing the condition on during sex, so you may want to avoid having sex until it's cleared up.
Some treatments can also weaken latex condoms and diaphragms (see above), so you may want to avoid having sex or use another form of contraception during treatment and for a few days afterwards.
If thrush keeps coming back
Speak to your GP if you experience frequent bouts of thrush.
They might run some tests to confirm the diagnosis and check for any possible underlying cause, such as diabetes.
They may also give you a prescription you can use whenever the symptoms return, or suggest trying a longer course of treatment lasting up to six months.
If you're pregnant or breastfeeding
Visit your GP if you have thrush and you're pregnant or breastfeeding.
Your GP will probably suggest using pessaries or an intravaginal cream. Capsules aren't recommended because they could harm your baby.
If you're pregnant, take care when using an applicator to insert a pessary or intravaginal cream, as there's a small risk of injuring your cervix (neck of the womb).
Antifungal skin cream or moisturisers can normally be used safely if you're pregnant or breastfeeding and the area around the entrance to your vagina is sore or itchy.
Alternative treatments
Some women with thrush try complementary therapies, such as bathing with diluted tea tree oil gel, eating probiotic yoghurts or supplements, or applying probiotic yoghurt to the genital area.
However, there's little evidence to suggest that tea tree oil is helpful, and it can sometimes irritate the skin.
Probiotics are unlikely to have any side effects, but there's also little evidence to suggest they can help.
Page last reviewed: 04/03/2016
Next review due: 04/03/2018
Source: NHS Choice, UK
More on Vaginal Thrush
Source: www.Savvychecktest.co.uk
More on Vaginal Yeast Infections

Most women will get a vaginal yeast infection at some point in their life. Symptoms of vaginal yeast infections include burning, itching, and thick, white discharge. Yeast infections are easy to treat, but it is important to see your doctor or nurse if you think you have an infection. Yeast infection symptoms are similar to other vaginal infections and sexually transmitted infections (STIs). If you have a more serious infection, and not a yeast infection, it can lead to major health problems.
What is a vaginal yeast infection?
A vaginal yeast infection is an infection of the vagina that causes itching and burning of the vulva, the area around the vagina. Vaginal yeast infections are caused by an overgrowth of the fungus Candida.

Who gets vaginal yeast infections?

Women and girls of all ages can get vaginal yeast infections. Three out of four women will have a yeast infection at some point in their life. Almost half of women have two or more infections.1
Vaginal yeast infections are rare before puberty and after menopause.
Are some women more at risk for yeast infections?
Yes. Your risk for yeast infections is higher if:2
- You are pregnant
- You have diabetes and your blood sugar is not under control
- You use a type of hormonal birth control that has higher doses of estrogen
- You douche or use vaginal sprays
- You recently took antibiotics such as amoxicillin or steroid medicines
- You have a weakened immune system, such as from HIV
What are the symptoms of vaginal yeast infections?
The most common symptom of a vaginal yeast infection is extreme itchiness in and around the vagina.
Other signs and symptoms include:
- Burning, redness, and swelling of the vagina and the vulva
- Pain when urinating
- Pain during sex
- Soreness
- A thick, white vaginal discharge that looks like cottage cheese and does not have a bad smell
You may have only a few of these symptoms. They may be mild or severe.
What causes yeast infections?
Yeast infections are caused by overgrowth of the microscopic fungus Candida.
Your vagina may have small amounts of yeast at any given time without causing any symptoms. But when too much yeast grows, you can get an infection.
Can I get a yeast infection from having sex?
Yes. A yeast infection is not considered an STI, because you can get a yeast infection without having sex. But you can get a yeast infection from your sexual partner. Condoms and dental dams may help prevent getting or passing yeast infections through vaginal, oral, or anal sex.
Should I call my doctor or nurse if I think I have a yeast infection?
Yes. Seeing your doctor or nurse is the only way to know for sure if you have a yeast infection and not a more serious type of infection.
The signs and symptoms of a yeast infection are a lot like symptoms of other more serious infections, such as STIs and bacterial vaginosis (BV). If left untreated, STIs and BV raise your risk of getting other STIs, including HIV, and can lead to problems getting pregnant. BV can also lead to problems during pregnancy, such as premature delivery.
How is a yeast infection diagnosed?
Your doctor will do a pelvic exam to look for swelling and discharge. Your doctor may also use a cotton swab to take a sample of the discharge from your vagina. A lab technician will look at the sample under a microscope to see whether there is an overgrowth of the fungus Candida that causes a yeast infection.
How is a yeast infection treated?
Yeast infections are usually treated with antifungal medicine. See your doctor or nurse to make sure that you have a vaginal yeast infection and not another type of infection.
You can then buy antifungal medicine for yeast infections at a store, without a prescription. Antifungal medicines come in the form of creams, tablets, ointments, or suppositories that you insert into your vagina. You can apply treatment in one dose or daily for up to seven days, depending on the brand you choose.
Your doctor or nurse can also give you a single dose of antifungal medicine taken by mouth, such as fluconazole (floo-CON-uh-zohl). If you get more than four vaginal yeast infections a year, or if your yeast infection doesn't go away after using over-the-counter treatment, you may need to take regular doses of antifungal medicine for up to six months.
Is it safe to use over-the-counter medicines for yeast infections?
Yes, but always talk with your doctor or nurse before treating yourself for a vaginal yeast infection. This is because:
- You may be trying to treat an infection that is not a yeast infection. Studies show that two out of three women who buy yeast infection medicine don't really have a yeast infection.2 Instead, they may have an STI or bacterial vaginosis (BV). STIs and BV require different treatments than yeast infections and, if left untreated, can cause serious health problems.
- Using treatment when you do not actually have a yeast infection can cause your body to become resistant to the yeast infection medicine. This can make actual yeast infections harder to treat in the future.
- Some yeast infection medicine may weaken condoms and diaphragms, increasing your chance of getting pregnant or an STI when you have sex. Talk to your doctor or nurse about what is best for you, and always read and follow the directions on the medicine carefully.
How do I treat a yeast infection if I'm pregnant?
During pregnancy, it's safe to treat a yeast infection with vaginal creams or suppositories that contain miconazole or clotrimazole.
Do not take the oral fluconazole tablet to treat a yeast infection during pregnancy. It may cause birth defects.3
Can I get a yeast infection from breastfeeding?
Yes. Yeast infections can happen on your nipples or in your breast (commonly called "thrush") from breastfeeding. Yeast thrive on milk and moisture. A yeast infection you get while breastfeeding is different from a vaginal yeast infection. However, it is caused by an overgrowth of the same fungus.
Symptoms of thrush during breastfeeding include:
- Sore nipples that last more than a few days, especially after several weeks of pain-free breastfeeding
- Flaky, shiny, itchy, or cracked nipples
- Deep pink and blistered nipples
- Achy breast
- Shooting pain in the breast during or after feedings
If you have any of these signs or symptoms or think your baby might have thrush in his or her mouth, call your doctor. Learn more about thrush in our Breastfeeding section.
If I have a yeast infection, does my sexual partner need to be treated?
Maybe. Yeast infections are not STIs. But it is possible to pass yeast infections to your partner during vaginal, oral, or anal sex.
- If your partner is a man, the risk of infection is low. About 15% of men get an itchy rash on the penis if they have unprotected sex with a woman who has a yeast infection. If this happens to your partner, he should see a doctor. Men who haven't been circumcised and men with diabetes are at higher risk.
- If your partner is a woman, she may be at risk. She should be tested and treated if she has any symptoms.
How can I prevent a yeast infection?
You can take steps to lower your risk of getting yeast infections:
- Do not douche. Douching removes some of the normal bacteria in the vagina that protects you from infection.
- Do not use scented feminine products, including bubble bath, sprays, pads, and tampons.
- Change tampons, pads, and panty liners often.
- Do not wear tight underwear, pantyhose, pants, or jeans. These can increase body heat and moisture in your genital area.
- Wear underwear with a cotton crotch. Cotton underwear helps keep you dry and doesn't hold in warmth and moisture.
- Change out of wet swimsuits and workout clothes as soon as you can.
- After using the bathroom, always wipe from front to back.
- Avoid hot tubs and very hot baths.
- If you have diabetes, be sure your blood sugar is under control.
Does yogurt prevent or treat yeast infections?
Maybe. Studies suggest that eating eight ounces of yogurt with "live cultures" daily or taking Lactobacillus acidophilus capsules can help prevent infection.4,5
But, more research still needs to be done to say for sure if yogurt with Lactobacillus or other probiotics can prevent or treat vaginal yeast infections. If you think you have a yeast infection, see your doctor or nurse to make sure before taking any over-the-counter medicine.
What should I do if I get repeat yeast infections?
If you get four or more yeast infections in a year, talk to your doctor or nurse.
About 5% of women get four or more vaginal yeast infections in one year. This is called recurrent vulvovaginal candidiasis (RVVC). RVVC is more common in women with diabetes or weak immune systems, such as with HIV, but it can also happen in otherwise healthy women.
Doctors most often treat RVVC with antifungal medicine for up to six months. Researchers also are studying the effects of a vaccine to help prevent RVVC (link is external).
Did we answer your question about vaginal yeast infections?
For more information on vaginal yeast infections, call the OWH Helpline at 800-994-9662 or contact the following organizations:
- Centers for Disease Control and Prevention (CDC), HHS
Phone Number: 800-232-4636
- National Institute of Allergy and Infectious Diseases (NIAID), NIH, HHS
Phone Number: 866-284-4107 (TDD: 800-877-8339)
- American College of Obstetricians and Gynecologists (ACOG) (link is external)
Phone Number: 800-673-8444
- Planned Parenthood Federation of America (link is external)
Phone Number: 800-230-7526
Sources
- Achkar, J.M., Fries, B.C. (2010). Candida Infections of the Genitourinary Tract. Clinical Microbiology Reviews; 23(2): 253–273.
- Ferris, D.G., Nyirjesy, P., Sobel, J.D., Soper, D., Pavletic, A., Litaker, M.S. (2002). Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstetrics and Gynecology; 99(3): 419–25
Page last updated: April 18, 2017.
Source: Office on Women's Health, HHS
Lymphogranuloma Venereum (LGV)

What is lymphogranuloma venereum (LGV)?

LGV is a sexually transmitted disease (STD) or infection involving the lymph glands in the genital area.
It is caused by a specific strain of Chlamydia. Who gets LGV?
The incidence is highest among sexually active people living in tropical or subtropical climates.
It has also occurred in some areas of the southern United States. How is LGV spread?
The infection is spread by sexual contact.
What are the symptoms of LGV?
The first symptom may be a small, painless pimple or lesion occurring on the penis or vagina. It is often unnoticed. The infection then spreads to the lymph nodes in the groin area and from there to the surrounding tissue. Complications may include inflamed and swollen lymph glands which may drain and bleed. How soon do symptoms appear?
The onset of symptoms varies widely.
The initial lesion may appear from three to 30 days after exposure. When and for how long is a person able to spread LGV?
An individual remains infectious as long as there are active lesions.
What is the treatment for LGV?
Treatment involves the use of certain antibiotics, specifically tetracycline or sulfamethoxazole.
What can be done to prevent the spread of LGV?
There are a number of ways to prevent the spread of LGV: Limit your number of sex partners.
Use a male or female condom. Carefully wash genitals after sexual relations.
If you think you are infected, avoid any sexual contact and visit your local STD clinic, a hospital or your doctor.
Notify all sexual contacts immediately so they can obtain examination and treatment.
Last Reviewed: November 2006
Source: New York State Department of Health
CONDITION: Scabies

Last Reviewed: October 2011
What is scabies?
Scabies is a fairly common infectious disease of the skin caused by a mite. Scabies mites burrow into the skin producing pimple-like irritations or burrows.
Who gets scabies?

Child with Scabies
Scabies infestations can affect people from all socioeconomic levels without regard to age, sex, race or standards of personal hygiene. Clusters of cases or outbreaks are occasionally seen in nursing homes, institutions and child care centers.
How is scabies spread?
Scabies mites are transferred by direct skin-to-skin contact. Indirect transfer from undergarments or bedclothes can occur only if these have been contaminated by infested people immediately beforehand. Scabies can also be transmitted during sexual contact.
What are the symptoms of scabies?
Bedbugs
The most prominent symptom of scabies is intense itching particularly at night. The areas of the skin most affected by scabies include the webs and sides of the fingers, around the wrists, elbows and armpits, waist, thighs, genitalia, nipples, breasts and lower buttocks.
Can Bedbugs Cause Scabies?
Can Bedbugs Cause Scabies?
Can Bedbugs Cause Scabies?

No, bedbugs do not cause scabies. Both of these are completely different infestations. Let’s learn more.
Before delving into the differences, check the main points of matches between the bedbug bites and scabies
- Both of them can cause itchy rashes on our skin
- The itchiness is usually worse at nighttime.
- In both the cases, if you are in doubt of getting any of them, immediate diagnosis and professional treatment accordingly is important.
Now, here are the points of differences between scabies and bedbug bites:
- See more at: http://www.drscabies.com/can-bedbugs-cause-scabie#sthash.XFVKpIiN.dpuf
Can Bedbugs Cause Scabies?
No, bedbugs do not cause scabies. Both of these are completely different infestations. Let’s learn more.
Before delving into the differences, check the main points of matches between the bedbug bites and scabies
- Both of them can cause itchy rashes on our skin
- The itchiness is usually worse at nighttime.
- In both the cases, if you are in doubt of getting any of them, immediate diagnosis and professional treatment accordingly is important.
Now, here are the points of differences between scabies and bedbug bites:
- See more at: http://www.drscabies.com/can-bedbugs-cause-scabie#sthash.XFVKpIiN.dpuf
No, bedbugs do not cause scabies. Both are completely different infestations.
How soon do symptoms appear?
Symptoms will appear from four to six weeks in people who have not previously been exposed to scabies infestations. People who have had a previous bout with scabies mites may show symptoms within one to four days after subsequent re-exposures.
When and for how long is a person able to spread scabies?
A person is able to spread scabies until mites and eggs are destroyed by treatment.
What is the treatment for scabies?
Skin lotions or creams containing scabicides are available through a physician's prescription for the treatment of scabies. The lotions are applied to the whole body below the head. Sometimes, itching may persist but should not be regarded as treatment failure or reinfestation. Persons who have had skin contact with an infested person (including family members, roommates, direct care providers and sexual contacts) should also be treated.
What can be done to prevent the spread of scabies?
Avoid physical contact with infested individuals and their belongings, especially clothing and bedding. Health education on the life history of scabies, proper treatment and the need for early diagnosis and treatment of infested individuals and contacts is extremely important.
NYS Health Dept.
Pubic lice and Scabies
Pubic lice are tiny parasitic insects that live in coarse body hair, such as pubic hair. They are yellow-grey and about 2mm long. They have a crab-like appearance, so they are often known as crabs. The eggs appear as brownish dots fixed to coarse body hair. Pubic lice are different from the head lice which some people get on their scalp.
Scabies is caused by tiny parasitic mites. They are smaller than a pinhead and burrow into the skin and lay eggs. A more severe and uncommon form of the condition occurs when there are many mites in the skin. This is called crusted scabies, and can affect older people and people with certain illnesses, such as HIV infection.
Getting pubic lice and scabies is common. These infections are easily passed from one person to another through close body contact or sexual contact. Both men and women can get and pass them on, and it is possible for children to get scabies through close body contact.
CONDITION: Pubic Lice (Crabs)


Download a PDF version of the Crabs Fact Sheet
Other languages:[Español]

Image Source: Scitechdaily.com
Crabs (also called pubic lice) are small, wingless insects that infest pubic hair. Both men and women can get crabs.
How causes crabs?

Crabs are usually spread through sexual contact.They can also be spread through contaminated clothing and bedding.
What are the symptoms of crabs?
Symptoms, which usually appear within five days of being exposed, include itching in the groin area.The crabs look like small flakes of skin to the naked eye, but you can actually see the insects with a magnifying glass.You may also see white or gray dots in your pubic hair; these are louse eggs.
How will I know if I have crabs?
Your doctor or other health care provider can tell if you have crabs by examining the infested area.
How are crabs treated?
- Medicated creams and shampoos can cure crabs. Some of these treatments are available without a prescription at the drug store. Follow directions carefully.
- You do not need to shave your pubic hair to remove crabs.
- Clothes, bedding, towels, and other items that may contain the lice should be machinewashed and dried on a hot cycle setting, or dry-cleaned.
- Articles that cannot be washed can be sealed in a plastic bag for 72 hours. Fumigation of living areas is not necessary.
- A person can become re-infested after treatment if exposed to crabs again.
What if I don't get treated?
In addition to the discomfort of the infestation, repeated scratching of the infested area can result in a serious skin infection. If you have symptoms or think you've been exposed to crabs, get examined and treated immediately to avoid any complications and continued transmission.
Do my sex partners have to be treated?
Yes. If you're diagnosed with crabs, it's important to tell everyone you've had sex with recently, so they can be examined and treated, too.
- Take all your medication as directed, even if you feel better before the medicine is finished.
- Don't have sex until you and the people you've had sex with have been completely treated and all of your symptoms have disappeared, oryou could infest each other again.
- Household members, including children, should also be examined, even if they have no symptoms.
What if I'm pregnant?
We don't know of any serious effects - on the mother or the baby - of having crabs during pregnancy, but you should tell your provider that you're pregnant when you seek treatment for crabs.
- Some medicated shampoos and creams used to treat crabs could be dangerous to an unborn baby and should not be used by women who are pregnant or breast-feeding, so you should tell your healthcare provider if you're pregnant or breast-feeding when you seek treatment for crabs.
- All pregnant women should be tested for other sexually transmitted diseases (STDs), including HIV, as early as possible in pregnancy.
- You should be tested again during your pregnancy if you are at higher risk for getting an STD. For example, you are at higher risk if you have a new partner during pregnancy, or if you have more than one partner.
- If left untreated, STDs can be devastating for your baby.To protect yourself and your baby against HIV and other STDs, use a latex condom whenever you have sex.
How can I avoid a yeast infection?
Latex condoms may be helpful in preventing the sexual transmission of crabs, but only when the infestation is covered or protected by the condom. Infections that are sexually transmitted can be avoided by not having sex. If you are sexually active, you can reduce your risk of getting crabs and most other sexually transmitted diseases (STDs), including HIV, by having sex only in a mutually monogamous relationship with a partner you are sure is not infected. If you are having sex outside of such a relationship, you can reduce your risk of STDs by:
1. Always using a latex condom (or other type of latex barrier) whenever you have sex - vaginal, anal, or oral. Condoms made of 'natural'materials, such as lambskin, protect against pregnancy, but not against STDs. If you are allergic to latex, you can use condoms made of polyurethane or other synthetic materials..
2. Limiting the number of people you have sex with. The more partners you have, the higher your risk.
3. Avoiding alcohol and drugs when you have sex. Drinking or getting high makes it much harder to remember to use condoms to protect yourself and others. For free, confidential help with a substance abuse problem, call (888) NYC-WELL (888-692-9355), or call 311.
More Information
Free, confidential STD exams and treatment, and confidential or anonymous HIV counseling and testing, are available at Health Department clinics in all 5 boroughs of New York City. Health insurance, proof of citizenship, and parental consent are NOT required. See a list of clinics and hours online or call 311 .
Source: NYS Health Department
CONDITION: Pediculosis (head lice, body lice, pubic lice, cooties, crabs)


What is pediculosis?
Pediculosis is an infestation of the hairy parts of the body or clothing with the eggs, larvae or adults of lice. The crawling stages of this insect feed on human blood, which can result in severe itching. Head lice are usually located on the scalp, crab lice in the pubic area and body lice along seams of clothing. Body lice travel to the skin to feed and return back to the clothing.

Who gets pediculosis?
Anyone may become louse infested under suitable conditions of exposure. Pediculosis is easily transmitted from person to person during direct contact. Head lice infestations are frequently found in school settings or institutions. Crab lice infestations can be found among sexually active individuals. Body lice infestation can be found in people living in crowded, unsanitary conditions where clothing is infrequently changed or laundered.
How is pediculosis spread?
For both head lice and body lice, transmission can occur during direct contact with an infested individual. Sharing of clothing and combs or brushes may also result in transmission of these insects. While other means are possible, crab lice are most often transmitted through sexual contact.
What are the symptoms of pediculosis?



Peduculosis capitis
Usually, the first indication of an infestation is the itching or scratching in the area of the body where the lice feed. Scratching at the back of the head or around the ears should lead to an examination for head louse eggs (nits) on the hair. Itching around the genital area should lead to an examination for crab lice or their eggs. Scratching can be sufficiently intense to result in secondary bacterial infection in these areas.
How soon do symptoms appear?
It may take as long as two to three weeks or longer for a person to notice the intense itching associated with this infestation.
For how long is a person able to spread pediculosis?
Pediculosis can be spread as long as lice or eggs remain alive on the infested person or clothing.
What is the treatment for pediculosis?
Medicated shampoos or cream rinses containing pyrethrins or permethrin are preferred for treating people with head lice. Products containing pyrethrins, permethrin or malathion are available over-the-counter, but those containing lindane or malathion are available only through a physician's prescription. Lindane-based shampoos are not recommended for infants, young children, pregnant women, lactating women, the elderly, persons with HIV or seizure disorders, persons who have very irritated skin or sores where the lidane will be applied and persons who weigh less than 110 pounds. Retreatment after 7 to 10 days is often recommended to ensure that no eggs have survived. Nit combs are available to help remove nits from hair. Dose and duration of shampoo treatment should be followed carefully according to label instructions.
What can be done to prevent the spread of pediculosis?
Physical contact with infested individuals and their belongings, especially clothing, headgear and bedding, should be avoided. Health education on the life history of lice, proper treatment and the importance of laundering clothing and bedding in hot water or dry cleaning to destroy lice and eggs is extremely valuable. In addition, regular direct inspection of children for head lice, and when indicated, of body and clothing, particularly of children in schools, institutions, nursing homes and summer camps, is important.
Source: NYS Health Department
Pubic Lice (“Crabs”) and Scabies
(Pubic lice caused by Phthirus pubis, the crab louse, and Scabies caused by Sarcoptes scabiei, a mite)
Sexually Transmitted Disease Facts
Signs and Symptoms
- Severe itching
- Sometimes lice can be seen in hairy parts of body
Transmission
- Sexual contact
- Close physical contact
- Infested towels, bedding and clothing
Transmission from toilet seats is unlikely.
Complications
If left untreated:
- Can spread to sex partners
- Pubic lice can spread from pubic hair to other hairy areas
- Scabies can spread through a family
Prevention
- Avoiding vaginal, oral or anal sex is the best way to prevent STDs.
- Limit the number of sex partners.
- Notify sex partners immediately if infested.
- Infested sex partners should be treated.
- Avoid sleeping in the same bed or sharing towels or clothes with someone who is infested.
Testing and Treatment
Treatment of Pubic Lice and Scabies:
- Get a test from a medical provider if infection is suspected.
- Can be killed using medication prescribed by a medical provider or, in the case of pubic lice, over-the-counter products.
- Partners should be treated at same time.
- Wash all clothes and bedding in hot water.
- Vacuum furniture.
NOTE: A person can be reinfected after treatment.
For more information, contact:
STD, HIV and TB Section
Minnesota Department of Health
651-201-5414
Minnesota Family Planning and STD Hotline
1-800-783-2287 Voice/TTY; 651-645-9360 (Metro)
American Social Health Association (ASHA)
CDC National STD and AIDS Hotlines
1-800-CDC-INFO; 1-888-232-6348 TTY
1-800-344-7432 (Spanish)
Content Notice: This site contains HIV or STD prevention messages that may not be appropriate for all audiences. Since HIV and other STDs are spread primarily through sexual practices or by sharing needles, prevention messages and programs may address these topics. If you are not seeking such information or may be offended by such materials, please exit this web site.
Frequently Asked Questions (FAQs)
On this Page
- What are pubic lice?
- What do pubic lice look like?
- Where are pubic lice found?
- What are the signs and symptoms of pubic lice?
- How did I get pubic lice?
- How is pubic lice infestation diagnosed?
- How is a pubic lice infestation treated?
What are pubic lice?
Also called crab lice or "crabs," pubic lice are parasitic insects found primarily in the pubic or genital area of humans. Pubic lice infestation is found worldwide and occurs in all races, ethnic groups, and levels of society.
What do pubic lice look like?
Pubic lice have three forms: the egg (also called a nit), the nymph, and the adult.
Nit: Nits are lice eggs. They can be hard to see and are found firmly attached to the hair shaft. They are oval and usually yellow to white. Pubic lice nits take about 6–10 days to hatch.
Nymph: The nymph is an immature louse that hatches from the nit (egg). A nymph looks like an adult pubic louse but it is smaller. Pubic lice nymphs take about 2–3 weeks after hatching to mature into adults capable of reproducing. To live, a nymph must feed on blood.
Adult: The adult pubic louse resembles a miniature crab when viewed through a strong magnifying glass. Pubic lice have six legs; their two front legs are very large and look like the pincher claws of a crab. This is how they got the nickname "crabs." Pubic lice are tan to grayish-white in color. Females lay nits and are usually larger than males. To live, lice must feed on blood. If the louse falls off a person, it dies within 1–2 days.
Where are pubic lice found?
Pubic lice usually are found in the genital area on pubic hair; but they may occasionally be found on other coarse body hair, such as hair on the legs, armpits, mustache, beard, eyebrows, or eyelashes. Pubic lice on the eyebrows or eyelashes of children may be a sign of sexual exposure or abuse. Lice found on the head generally are head lice, not pubic lice.
Animals do not get or spread pubic lice.
What are the signs and symptoms of pubic lice?
Signs and symptoms of pubic lice include
- Itching in the genital area
- Visible nits (lice eggs) or crawling lice
How did I get pubic lice?
Pubic lice usually are spread through sexual contact and are most common in adults. Pubic lice found on children may be a sign of sexual exposure or abuse. Occasionally, pubic lice may be spread by close personal contact or contact with articles such as clothing, bed linens, or towels that have been used by an infested person. A common misconception is that pubic lice are spread easily by sitting on a toilet seat. This would be extremely rare because lice cannot live long away from a warm human body and they do not have feet designed to hold onto or walk on smooth surfaces such as toilet seats.
Persons infested with pubic lice should be examined for the presence of other sexually transmitted diseases.
How is a pubic lice infestation diagnosed?
A pubic lice infestation is diagnosed by finding a "crab" louse or egg (nit) on hair in the pubic region or, less commonly, elsewhere on the body (eyebrows, eyelashes, beard, mustache, armpit, perianal area, groin, trunk, scalp). Pubic lice may be difficult to find because there may be only a few. Pubic lice often attach themselves to more than one hair and generally do not crawl as quickly as head and body lice. If crawling lice are not seen, finding nits in the pubic area strongly suggests that a person is infested and should be treated. If you are unsure about infestation or if treatment is not successful, see a health care provider for a diagnosis. Persons infested with pubic lice should be investigated for the presence of other sexually transmitted diseases.
Although pubic lice and nits can be large enough to be seen with the naked eye, a magnifying lens may be necessary to find lice or eggs.
How is a pubic lice infestation treated?
Treatment
A lice-killing lotion containing 1% permethrin or a mousse containing pyrethrins and piperonyl butoxide can be used to treat pubic ("crab") lice. These products are available over-the-counter without a prescription at a local drug store or pharmacy. These medications are safe and effective when used exactly according to the instructions in the package or on the label.
Lindane shampoo is a prescription medication that can kill lice and lice eggs. However, lindane is not recommended as a first-line therapy. Lindane can be toxic to the brain and other parts of the nervous system; its use should be restricted to patients who have failed treatment with or cannot tolerate other medications that pose less risk. Lindane should not be used to treat premature infants, persons with a seizure disorder, women who are pregnant or breast-feeding, persons who have very irritated skin or sores where the lindane will be applied, infants, children, the elderly, and persons who weigh less than 110 pounds.
Malathion* lotion 0.5% (Ovide*) is a prescription medication that can kill lice and some lice eggs; however, malathion lotion (Ovide*) currently has not been approved by the U.S. Food and Drug Administration (FDA) for treatment of pubic ("crab") lice.
Both topical and oral ivermectin have been used successfully to treat lice; however, only topical ivermectin lotion currently is approved by the U.S. Food and Drug Administration (FDA) for treatment of lice. Oral ivermectin is not FDA-approved for treatment of lice.
How to treat pubic lice infestations: (Warning: See special instructions for treatment of lice and nits on eyebrows or eyelashes. The lice medications described in this section should not be used near the eyes.)
- Wash the infested area; towel dry.
- Carefully follow the instructions in the package or on the label. Thoroughly saturate the pubic hair and other infested areas with lice medication. Leave medication on hair for the time recommended in the instructions. After waiting the recommended time, remove the medication by following carefully the instructions on the label or in the box.
- Following treatment, most nits will still be attached to hair shafts. Nits may be removed with fingernails or by using a fine-toothed comb.
- Put on clean underwear and clothing after treatment.
- To kill any lice or nits remaining on clothing, towels, or bedding, machine-wash and machine-dry those items that the infested person used during the 2–3 days before treatment. Use hot water (at least 130°F) and the hot dryer cycle.
- Items that cannot be laundered can be dry-cleaned or stored in a sealed plastic bag for 2 weeks.
- All sex partners from within the previous month should be informed that they are at risk for infestation and should be treated.
- Persons should avoid sexual contact with their sex partner(s) until both they and their partners have been successfully treated and reevaluated to rule out persistent infestation.
- Repeat treatment in 9–10 days if live lice are still found.
- Persons with pubic lice should be evaluated for other sexually transmitted diseases (STDs).
Special instructions for treatment of lice and nits found on eyebrows or eyelashes:
- If only a few live lice and nits are present, it may be possible to remove these with fingernails or a nit comb.
- If additional treatment is needed for lice or nits on the eyelashes, careful application of ophthalmic-grade petrolatum ointment (only available by prescription) to the eyelid margins 2–4 times a day for 10 days is effective. Regular petrolatum (e.g., Vaseline)* should not be used because it can irritate the eyes if applied.
*Use of trade names is for identification purposes only and does not imply endorsement by the Public Health Service or by the U.S. Department of Health and Human Services.
Source: CDC
Pediculosis (lice, head lice, body lice, pubic lice, cooties, crabs)
What is pediculosis?
Pediculosis is an infestation of the hairy parts of the body or clothing with the eggs, larvae or adults of lice. The crawling stages of this insect feed on human blood, which can result in severe itching. Head lice are usually located on the scalp, crab lice in the pubic area and body lice along seams of clothing. Body lice travel to the skin to feed and return back to the clothing.
Who gets pediculosis?
Anyone may become louse infested under suitable conditions of exposure. Pediculosis is easily transmitted from person to person during direct contact. Head lice infestations are frequently found in school settings or institutions. Crab lice infestations can be found among sexually active individuals. Body lice infestation can be found in people living in crowded, unsanitary conditions where clothing is infrequently changed or laundered.
How is pediculosis spread?
For both head lice and body lice, transmission can occur during direct contact with an infested individual. Sharing of clothing and combs or brushes may also result in transmission of these insects. While other means are possible, crab lice are most often transmitted through sexual contact.
What are the symptoms of pediculosis?
Usually, the first indication of an infestation is the itching or scratching in the area of the body where the lice feed. Scratching at the back of the head or around the ears should lead to an examination for head louse eggs (nits) on the hair. Itching around the genital area should lead to an examination for crab lice or their eggs. Scratching can be sufficiently intense to result in secondary bacterial infection in these areas.
How soon do symptoms appear?
It may take as long as two to three weeks or longer for a person to notice the intense itching associated with this infestation.
For how long is a person able to spread pediculosis?
Pediculosis can be spread as long as lice or eggs remain alive on the infested person or clothing.
What is the treatment for pediculosis?
Medicated shampoos or cream rinses containing pyrethrins or permethrin are preferred for treating people with head lice. Products containing pyrethrins, permethrin or malathion are available over-the-counter, but those containing lindane or malathion are available only through a physician's prescription. Lindane-based shampoos are not recommended for infants, young children, pregnant women, lactating women, the elderly, persons with HIV or seizure disorders, persons who have very irritated skin or sores where the lidane will be applied and persons who weigh less than 110 pounds. Retreatment after 7 to 10 days is often recommended to ensure that no eggs have survived. Nit combs are available to help remove nits from hair. Dose and duration of shampoo treatment should be followed carefully according to label instructions.
What can be done to prevent the spread of pediculosis?
Physical contact with infested individuals and their belongings, especially clothing, headgear and bedding, should be avoided. Health education on the life history of lice, proper treatment and the importance of laundering clothing and bedding in hot water or dry cleaning to destroy lice and eggs is extremely valuable. In addition, regular direct inspection of children for head lice, and when indicated, of body and clothing, particularly of children in schools, institutions, nursing homes and summer camps, is important.
MDH (Minnesota Dept. of Health)
CONDITION: Syphilis

Credit: NIAID, NIH
Treponema pallidum, the bacteria that cause syphilis.Credit: NIAID
Treponema pallidum, the bacteria that cause syphilis.

Syphilis is a sexually transmitted bacterial infection that causes genital ulcers (sores) in its early stages. If untreated, syphilis can also lead to more serious symptoms.




An ancient disease, syphilis is still of major importance today. The Centers for Disease Control and Prevention estimates that each year 55,400 people in the United States get new syphilis infections. During 2012, there were 49,903 reported new cases.
In addition, HIV infection and syphilis are linked. Syphilis increases the risk of transmitting as well as getting infected with HIV.?
Cause
Syphilis is caused by a bacterium called Treponema pallidum.
Transmission
The most common way to get syphilis is by having sexual contact with an infected person. If you are infected, you can pass the bacteria from infected skin or mucous membranes (linings), usually your genital area, lips, mouth, or anus, to the mucous membranes or skin of your sexual partner.
The bacteria are fragile, so you cannot get syphilis from sharing food or utensils, or from using tubs, pools, or toilets.
Syphilis can be passed from mother to infant during pregnancy, causing a disease called congenital syphilis.?
Symptoms
Syphilis is sometimes called "the great imitator." This is because it has so many possible symptoms, and its symptoms are like those of many other diseases. Having HIV infection at the same time as syphilis can change the symptoms of syphilis and how the disease develops.
Syphilis (other than congenital syphilis) occurs in four stages that sometimes overlap.
Primary Syphilis
The first symptom of primary syphilis is often a small, round, firm ulcer (sore) called a chancre ("shanker") at the place where the bacteria entered your body. This place is usually the penis, vulva, or vagina, but chancres also can develop on the cervix, tongue, lips, or other parts of the body. Usually there is only one chancre, but sometimes there may be many. Nearby lymph glands are often swollen. (Lymph glands, or nodes, are small bean-shaped organs of your immune system containing cells that help fight off germs. They are found throughout your body.) The chancre usually appears about three weeks after you're infected with the bacteria, but it can occur any time from 9 to 90 days after you have been infected.
Because a chancre is usually painless and can appear inside your body, you might not notice it. The chancre disappears in about three to six weeks whether or not you are treated. Therefore, you can have primary syphilis without symptoms or with only brief symptoms that you may overlook.
If primary syphilis is not treated, however, the infection moves to the secondary stage.
Secondary syphilis
Most people with secondary syphilis have a skin rash that doesn't itch. The rash is usually on the palms of your hands and soles of your feet. However, it may cover your whole body or appear only in a few areas. The rash appears 2 to 10 weeks after the chancre, generally when the chancre is healing or already healed. Other common symptoms include
- Sore throat
- Tiredness
- Headache
- Swollen lymph glands
Other symptoms that happen less often include fever, aches, weight loss, hair loss, aching joints, or lesions (sores) in the mouth or genital area.
Your symptoms may be mild. The lesions of secondary syphilis contain many bacteria, and anyone who has contact with them can get syphilis. As with primary syphilis, secondary syphilis will seem to disappear even without treatment, but secondary syphilis can return. Without treatment, however, the infection will move to the next stages.
Latent syphilis
The latent (hidden) stage of syphilis begins when symptoms of secondary syphilis are over.
In early latent syphilis, you might notice that signs and symptoms disappear, but the infection remains in your body. When you are in this stage, you can still infect a sexual partner.
In late part of latent syphilis, the infection is quiet and the risk of infecting a sexual partner is low or not present.
If you don't get treated for latent syphilis, you may move on to tertiary syphilis, the most serious stage of the disease.
Tertiary syphilis
Even without treatment, only a small number of infected people develop the severe complications known as tertiary, or late, syphilis. In this stage, the bacteria will damage your heart, eyes, brain, nervous system, bones, joints, or almost any other part of your body. This damage can happen years or even decades after the primary stage.
Late syphilis can result in mental illness, blindness, deafness, memory loss or other neurologic problems, heart disease, and death.
Late neurosyphilis (brain or spinal cord damage) is one of the most severe complications of this stage.
Diagnosis
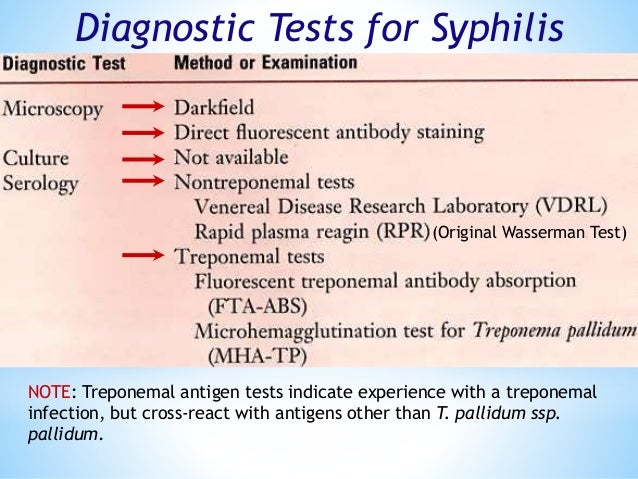
It can be very difficult for your healthcare provider to diagnose syphilis based on symptoms. This is because symptoms and signs of the disease might be absent, go away without treatment, or be confused with those of other diseases. Because syphilis can be hard to diagnose, you should
- Visit your healthcare provider if you have a lesion (sore) in your genital area or a widespread rash
- Get tested periodically for syphilis if your sexual behaviors put you at risk for sexually transmitted diseases (STDs)
- Get tested for syphilis if you have been treated for another STD such as gonorrhea or HIV infection
Laboratory Tests
Your healthcare provider can diagnose early syphilis by seeing a chancre or rash and then confirming the diagnosis with laboratory tests. Because latent syphilis has no symptoms, it is diagnosed only by laboratory tests.
There are two methods for diagnosing syphilis through a laboratory.
- Identifying the bacteria under a microscope in a sample of tissue (a group of cells) taken from a chancre
- Performing a blood test for syphilis
If your healthcare provider thinks you might have neurosyphilis, your spinal fluid will be tested as well.
Treatment
Syphilis is easy to cure in its early stages. Penicillin, an antibiotic, injected into the muscle, is the best treatment for syphilis. If you are allergic to penicillin, your healthcare provider may give you another antibiotic to take by mouth.
If you have neurosyphilis, you may need to get daily doses of penicillin intravenously (in the vein) and you may need to be treated in the hospital.
If you have late syphilis, damage done to your body organs cannot be reversed.
While you are being treated, you should abstain from sex until any sores are completely healed. You should also notify your sex partners so they can be tested for syphilis and treated if necessary.
For updated information on treatment for syphilis, read the Centers for Disease Control and Prevention Sexually Transmitted Diseases Treatment Guidelines.
Prevention
To prevent getting syphilis, you must avoid contact with infected tissue and body fluids of an infected person. However, syphilis is usually transmitted by people who have no sores that can be seen or rashes and don't know they are infected.
If you aren't infected with syphilis and are sexually active, having mutually monogamous sex with an uninfected partner is the best way to prevent syphilis.
Using condoms properly and consistently during sex reduces your risk of getting syphilis.
Washing or douching after sex won't prevent syphilis.
Even if you have been treated for syphilis and cured, you can be re-infected by having sex with an infected partner.
To prevent passing congenital syphilis to their unborn babies, all pregnant women should be tested for syphilis. Most cases of congenital syphilis can be avoided with appropriate screening and treatment of pregnant women.
Complications
Pregnancy
Syphilis can cause miscarriages, premature births, or stillbirths. It can also cause death of newborn babies. Some infants with congenital syphilis have symptoms at birth, but most develop symptoms later.
Untreated babies with congenital syphilis can have deformities, delays in development, or seizures, along with many other problems such as rash, fever, swollen liver and spleen, anemia, and jaundice. Sores on infected babies are infectious. Rarely, the symptoms of early-stage syphilis may go unseen in infants and they may subsequently develop the symptoms of late-stage syphilis, including damage to their bones, teeth, eyes, ears, and brains.
HIV infection
People infected with syphilis have a two- to five-fold increase risk of getting infected with HIV. Strong evidence shows the increased odds of getting and transmitting HIV in the presence of other STDs as well. You should discuss this and other STDs with your healthcare provider.
Last Updated October 27, 2014
Source: NIAID, NIH
CDC: Symptoms of Syphilis (Click images to view full size)

Darkfield micrograph of Treponema pallidum.

Primary stage syphilis sore (chancre) on the surface of a tongue.

Lesions of secondary syphilis.
Secondary stage syphilis sores (lesions) on the palms of the hands. Referred to as "palmar lesions."
Secondary stage syphilis sores (lesions) on the bottoms of the feet. Referred to as "plantar lesions."

Secondary syphilis rash on the back.WARNING: the images below depicts the symptoms of STDs and are intended for educational use only. Parental caution is advised.
 Primar
Primar

Primary stage syphilis sore (chancre) inside the vaginal opening.
Source: CDC
More on Syphilis
What is syphilis?
Syphilis is a bacterial infection, primarily a sexually transmitted disease (STD).
Who gets syphilis?
Any sexually active person can be infected with syphilis, although there is a greater incidence among young people between the ages of 15 and 30 years. It is more prevalent in urban than rural areas.
How is syphilis spread?
Syphilis is spread by sexual contact with an infected individual, with the exception of congenital syphilis, which is spread from mother to fetus. Transmission by sexual contact requires exposure to moist lesions of skin or mucous membranes.
What are the symptoms of syphilis?
The symptoms of syphilis occur in stages called primary, secondary and late. The first or primary sign of syphilis is usually a sore(s), which is painless and appears at the site of initial contact. It may be accompanied by swollen glands, which develop within a week after the appearance of the initial sore. The sore may last from one to five weeks, and may disappear by itself even if no treatment is received. Approximately six weeks after the sore first appears, a person will enter the second stage of the disease. The most common symptom during this stage is a rash, which may appear on any part of the body including trunk, arms, legs, palms, soles, etc. Other symptoms may occur such as tiredness, fever, sore throat, headaches, hoarseness, loss of appetite, patchy hair loss and swollen glands. These signs and symptoms will last two to six weeks and generally disappear in the absence of adequate treatment. The third stage, called late syphilis (syphilis of over four years' duration), may involve illness in the skin, bones, central nervous system and heart.
How soon do symptoms appear?
Symptoms can appear from 10 to 90 days after a person becomes infected, but usually within three to four weeks. Symptoms are often not noticed or are thought to be minor abrasions or heat rash and medical care is not sought.
When and for how long is a person able to spread syphilis?
Syphilis is considered to be communicable for a period of up to two years, possibly longer. The extent of communicability depends on the existence of infectious lesions (sores), which may or may not be visible.
Does past infection with syphilis make a person immune?
There is no natural immunity to syphilis and past infection offers no protection to the patient.
What is the treatment for syphilis?
Syphilis is treated with penicillin or tetracycline. The amount of treatment depends on the stage of syphilis the patient is in. Pregnant women with a history of allergic reaction to penicillin should undergo penicillin desensitization followed by appropriate penicillin therapy. A baby born with the disease needs daily penicillin treatment for 10 days.
What are the complications associated with syphilis?
Untreated syphilis can lead to destruction of soft tissue and bone, heart failure, blindness and a variety of other conditions which may be mild to incapacitating. More important, a female with untreated syphilis may transmit the disease to her unborn child, which may result in death or deformity of the child. Physicians and hospitals are required to test pregnant females for syphilis at prenatal visits. Tests of newborns or their mothers are required at the time of delivery.
What can be done to prevent the spread of syphilis?
There are number of ways to prevent the spread of syphilis:
- Limit your number of sex partners;
- Use a male or female condom**;
- If you think you are infected, avoid sexual contact and visit your local STD clinic, a hospital or your doctor;
- Notify all sexual contacts immediately so they can obtain examination and treatment;
- All pregnant women should receive at least one prenatal blood test for syphilis.
** Remember that use of condoms may prevent the disease if the initial contact sore is on the penis or in the vaginal area. However, transmission can occur if the sore is outside the areas covered by the condom.
NYS Health Dept.
CONDITION: Treponematosis (endemic)

Situation and trends

Endemic treponematoses are a group of chronic bacterial infections caused by treponemes. These infections are:
- Yaws (also known as framboesia or pian) caused by Treponema pallidum subspecies Pertenue, the most common of these infections. Transmission occurs mainly in poor communities in warm, humid tropical regions of Africa, Asia, Latin America and the Pacific.
- Endemic syphilis (also known as bejel) caused by T. pallidum subspecies endemicum. Transmission occurs principally in the Sahel region of Africa and the Arabian Peninsula.
- Pinta caused by T. carateum. Transmission occurs only in the American region.
A review of the historic documents from 1950 to 2013 shows that 99 countries and territories are endemic for yaws; 22 are endemic for bejel and 19 are endemic for pinta.
Since 1990, formal reporting of data on endemic treponematoses to WHO is not mandatory and the availability of data is therefore limited. Only 15 of the 99 endemic countries and territories have recent data on yaws based on the routine surveillance system; however, these data may indicate only the presence of the disease and not its full extent. Ghana, Papua New Guinea and the Solomon Islands each report more than 10 000 cases per year. Ecuador and India appear to have interrupted transmission. There are no recent data reported on the number of cases of bejel and pinta.
Source: WHO
Background

Treponematosis, also known as treponemiasis, traditionally refers to the group of nonvenereal diseases (including endemic syphilis [nonvenereal syphilis]) caused by Treponema species that are morphologically and serologically identical to each other and to Treponema pallidum subspecies pallidum, the cause of venereal syphilis. They differ only in their clinical manifestations. Treponema species typically associated with nonvenereal disease are transmitted among children living in tropical, subtropical, or warm arid climates, chiefly by direct contact. In humans, the pathogenic treponemes include T pallidum pallidum, Treponema pertenue (yaws), Treponema endemicum (bejel or endemic syphilis), and Treponema carateum (pinta).
Pathophysiology
Treponemes usually invade traumatized cutaneous or mucosal surfaces that come in contact with a draining open sore of the index case. A primary cutaneous lesion appears at the site of inoculation following an incubation period of a few weeks. Treponema may be spread from this site either topically (by scratching) orematogenously. These lesions often heal spontaneously. Treponematosis can remain latent or it may recur.
The secondary stage of any of these diseases follows the dissemination of the treponemes. It may begin while the primary lesion is still present or after a variable latent period. It may also resolve spontaneously, recur, or persist. The long-term effects of these infections include multiple cutaneous lesions and destruction of bones or cartilage.
Epidemiology
Frequency
Although treponematosis does not occur in the United States, imported cases have been documented. It may be found in children immigrating from areas of endemicity, and the US Centers for Disease Control and Prevention (CDC) has recommended screening of all refugee children from endemic regions with a nontreponemal test at initial health screening.
International
In 1997, the World Health Organization (WHO) estimated that 460,000 new cases of endemic treponematosis occurred worldwide. Currently, more than 2.5 million people may be infected.
Endemic syphilis (bejel) (T pallidum endemicum) is typically spread among children, most commonly in the Middle East and the southern regions of the Sahara Desert. In Europe, cases have been diagnosed in children who have moved from endemic areas. In one study, 12% of children younger than 5 years in Niger were seropositive. High rates of seropositivity are also observed in Mali, Burkina Faso, and Senegal. Pinta (T carateum), which occurs in the Caribbean and in Central and South America, is more common in young adults.
Yaws (T pallidum pertenue) occurs mainly in equatorial regions and can be found in South America, Central America, the Caribbean, Africa, and Southeast Asia. It is associated with high humidity and rainfall. Fifty years ago, the WHO recognized that endemic treponematoses—yaws in particular—were a major cause of disfigurement and disability and a significant economic burden in poor countries.
In Haiti and the Dominican Republic, a pilot project was initiated to eradicate the disease with mass applications of penicillin. This project was so successful that it was extended to 46 other countries. Overall, the incidence of yaws was reduced to isolated foci of endemicity. As public health priorities changed and support for the eradication programs lapsed, the disease saw a resurgence in the 1970s and 1980s. The introduction of mass treatment has been necessary in some areas. In a WHO survey in 2012, the status of yaws was unknown in many of the countries where it had previously been known to be endemic.
Now that an oral treatment has been recommended for first-line therapy, a new eradication campaign is being planned by the WHO.
Mortality/Morbidity
Untreated treponematosis may cause disfiguring cutaneous lesions and deformities of bone, cartilage (particularly the nose), and skin, potentially leading to significant disfigurement, pain, and disability. Affected children can become socially ostracized and often miss school. Thickening and cracking of the soles may make walking difficult. Treponematosis can extract a significant economic toll on already-disadvantaged populations. Fortunately, with penicillin or azithromycin therapy, cure rates of 95-97% are possible.
Race
Treponematosis has no reported racial predilection in terms of frequency or severity.
Sex
Treponematosis has no reported sexual predilection in terms of frequency or severity.
Age
Although individuals of any age can acquire treponematosis, endemic syphilis and yaws are more common in children younger than 10 years, whereas pinta is more common in young adults. Yaws most often infects children and peaks in those aged 2-10 years. Of new cases, 75% arise in children younger than 15 years. Congenital infections with the endemic treponemes are unusual because most primary infections occur in children. Primary treponematosis during pregnancy is rare.
Source: eMedicine
CONDITION: Trichomoniasis (Trich)- CDC Fact Sheet



Most people who have trichomoniasis do not have any symptoms.
What is trichomoniasis?

Trichomoniasis (or “trich”) is a very common sexually transmitted disease (STD) that is caused by infection with a protozoan parasite called Trichomonas vaginalis. Although symptoms of the disease vary, most women and men who have the parasite cannot tell they are infected.
How common is trichomoniasis?

Trichomoniasis is considered the most common curable STD. In the United States, an estimated 3.7 million people have the infection, but only about 30% develop any symptoms of trichomoniasis. Infection is more common in women than in men, and older women are more likely than younger women to have been infected.
Two Trichomonas vaginalis parasites, magnified (seen under a microscope)
How do people get trichomoniasis?
The parasite is passed from an infected person to an uninfected person during sex. In women, the most commonly infected part of the body is the lower genital tract (vulva, vagina, or urethra), and in men, the most commonly infected body part is the inside of the penis (urethra). During sex, the parasite is usually transmitted from a penis to a vagina, or from a vagina to a penis, but it can also be passed from a vagina to another vagina. It is not common for the parasite to infect other body parts, like the hands, mouth, or anus. It is unclear why some people with the infection get symptoms while others do not, but it probably depends on factors like the person’s age and overall health. Infected people without symptoms can still pass the infection on to others.

What are the signs and symptoms of trichomoniasis?
About 70% of infected people do not have any signs or symptoms. When trichomoniasis does cause symptoms, they can range from mild irritation to severe inflammation. Some people with symptoms get them within 5 to 28 days after being infected, but others do not develop symptoms until much later. Symptoms can come and go.
Men with trichomoniasis may feel itching or irritation inside the penis, burning after urination or ejaculation, or some discharge from the penis.
Women with trichomoniasis may notice itching, burning, redness or soreness of the genitals, discomfort with urination, or a thin discharge with an unusual smell that can be clear, white, yellowish, or greenish.
Having trichomoniasis can make it feel unpleasant to have sex. Without treatment, the infection can last for months or even years.
STDs & Pregnancy

What are the complications of trichomoniasis?
Trichomoniasis can increase the risk of getting or spreading other sexually transmitted infections. For example, trichomoniasis can cause genital inflammation that makes it easier to get infected with the HIV virus, or to pass the HIV virus on to a sex partner.
How does trichomoniasis affect a pregnant woman and her baby?
Pregnant women with trichomoniasis are more likely to have their babies too early (preterm delivery). Also, babies born to infected mothers are more likely to have an officially low birth weight (less than 5.5 pounds).
How is trichomoniasis diagnosed?
It is not possible to diagnose trichomoniasis based on symptoms alone. For both men and women, your primary care doctor or another trusted health care provider must do a check and a laboratory test to diagnose trichomoniasis.

What is the treatment for trichomoniasis?
Trichomoniasis can be cured with a single dose of prescription antibiotic medication (either metronidazole or tinidazole), pills which can be taken by mouth. It is okay for pregnant women to take this medication. Some people who drink alcohol within 24 hours after taking this kind of antibiotic can have uncomfortable side effects.
People who have been treated for trichomoniasis can get it again. About 1 in 5 people get infected again within 3 months after treatment. To avoid getting reinfected, make sure that all of your sex partners get treated too, and wait to have sex again until all of your symptoms go away (about a week). Get checked again if your symptoms come back.
How can trichomoniasis be prevented?
Using latex condoms correctly every time you have sex will help reduce the risk of getting or spreading trichomoniasis. However, condoms don’t cover everything, and it is possible to get or spread this infection even when using a condom.
The only sure way to prevent sexually transmitted infections is to avoid having sex entirely. Another approach is to talk about these kinds of infections before you have sex with a new partner, so that you can make informed choices about the level of risk you are comfortable taking with your sex life.
If you or someone you know has questions about trichomoniasis or any other STD, especially with symptoms like unusual discharge, burning during urination, or a sore in the genital area, check in with a health care provider and get some answers.
Where can I get more information?
Division of STD Prevention (DSTDP)
Centers for Disease Control and Prevention
www.cdc.gov/std
American Sexual Health Association (ASHA)
P. O. Box 13827
Research Triangle Park, NC 27709-3827
1-800-783-9877
Source: CDC
CONDITION: Zika virus infection

Key facts
- Zika virus disease is caused by a virus transmitted primarily by Aedes mosquitoes.
- People with Zika virus disease can have symptoms including mild fever, skin rash, conjunctivitis, muscle and joint pain, malaise or headache. These symptoms normally last for 2-7 days.
- There is scientific consensus that Zika virus is a cause of microcephaly and Guillain-Barré syndrome. Links to other neurological complications are also being investigated.
Introduction
Zika virus is a mosquito-borne flavivirus that was first identified in Uganda in 1947 in monkeys through a network that monitored yellow fever. It was later identified in humans in 1952 in Uganda and the United Republic of Tanzania. Outbreaks of Zika virus disease have been recorded in Africa, the Americas, Asia and the Pacific. From the 1960s to 1980s, human infections were found across Africa and Asia, typically accompanied by mild illness. The first large outbreak of disease caused by Zika infection was reported from the Island of Yap (Federated States of Micronesia) in 2007. In July 2015 Brazil reported an association between Zika virus infection and Guillain-Barré syndrome. In October 2015 Brazil reported an association between Zika virus infection and microcephaly.
- More on the history of Zika virus
- Read the latest situation report
Signs and Symptoms
The incubation period (the time from exposure to symptoms) of Zika virus disease is not clear, but is likely to be a few days. The symptoms are similar to other arbovirus infections such as dengue, and include fever, skin rashes, conjunctivitis, muscle and joint pain, malaise, and headache. These symptoms are usually mild and last for 2-7 days.
Clinical Resources:

Measuring Head Circumference
- English[PDF – 1 page]
- Spanish[PDF – 1 page]
- Portuguese[PDF – 1 page]
- French[PDF – 1 page]
- Creole[PDF – 1 page]
Complications of Zika virus disease
Based on a systematic review of the literature up to 30 May 2016, WHO has concluded that Zika virus infection during pregnancy is a cause of congenital brain abnormalities, including microcephaly; and that Zika virus is a trigger of Guillain-Barré syndrome. Intense efforts are continuing to investigate the link between Zika virus and a range of neurological disorders, within a rigorous research framework.
Transmission

Zika virus is primarily transmitted to people through the bite of an infected mosquito from the Aedes genus, mainly Aedes aegypti in tropical regions. Aedes mosquitoes usually bite during the day, peaking during early morning and late afternoon/evening. This is the same mosquito that transmits dengue, chikungunya and yellow fever. Sexual transmission of Zika virus is also possible. Other modes of transmission such as blood transfusion are being investigated.
Diagnosis
Infection with Zika virus may be suspected based on symptoms and recent history of travel (e.g. residence in or travel to an area with active Zika virus transmission). A diagnosis of Zika virus infection can only be confirmed through laboratory tests on blood or other body fluids, such as urine, saliva or semen.
Treatment
Zika virus disease is usually mild and requires no specific treatment. People sick with Zika virus should get plenty of rest, drink enough fluids, and treat pain and fever with common medicines. If symptoms worsen, they should seek medical care and advice. There is currently no vaccine available.
Prevention
Mosquito bites
Protection against mosquito bites is a key measure to prevent Zika virus infection. This can be done by wearing clothes (preferably light-coloured) that cover as much of the body as possible; using physical barriers such as window screens or closing doors and windows; sleeping under mosquito nets; and using insect repellent containing DEET, IR3535 or icaridin according to the product label instructions. Special attention and help should be given to those who may not be able to protect themselves adequately, such as young children, the sick or elderly. Travellers and those living in affected areas should take the basic precautions described above to protect themselves from mosquito bites.
It is important to cover, empty or clean potential mosquito breeding sites in and around houses such as buckets, drums, pots, gutters, and used tyres. Communities should support local government efforts to reduce mosquitoes in their locality. Health authorities may also advise that spraying of insecticides be carried out.
- Vector control operations framework for Zika virus
Sexual transmission
Zika virus can be transmitted through sexual intercourse. This is of concern due to an association between Zika virus infection and adverse pregnancy and fetal outcomes.
For regions with active transmission of Zika virus, all people with Zika virus infection and their sexual partners (particularly pregnant women) should receive information about the risks of sexual transmission of Zika virus. WHO recommends that sexually active men and women be correctly counselled and offered a full range of contraceptive methods to be able to make an informed choice about whether and when to become pregnant in order to prevent possible adverse pregnancy and fetal outcomes. Women who have had unprotected sex and do not wish to become pregnant due to concerns about Zika virus infection should have ready access to emergency contraceptive services and counselling. Pregnant women should practice safer sex (including correct and consistent use of condoms) or abstain from sexual activity for at least the whole duration of the pregnancy.
For regions with no active transmission of Zika virus, WHO recommends practising safer sex or abstinence for a period of six months for men and women who are returning from areas of active transmission to prevent Zika virus infection through sexual intercourse. Sexual partners of pregnant women, living in or returning from areas where local transmission of Zika virus occurs should practice safer sex or abstain from sexual activity throughout the pregnancy.
WHO response
WHO is supporting countries to control Zika virus disease by taking actions outlined in the “Zika Strategic Response Framework":
- Define and prioritize research into Zika virus disease by convening experts and partners.
- Enhance surveillance of Zika virus and potential complications.
- Strengthen capacity in risk communication to engage communities to better understand risks associated with Zika virus.
- Strengthen the capacity of laboratories to detect the virus.
- Support health authorities to implement vector control strategies aimed at reducing Aedes mosquito populations.
- Prepare recommendations for the clinical care and follow-up of people with complications related to Zika virus infection, in collaboration with experts and other health agencies.
Source: WHO
Zika Overview-About Zika
History of Zika
Zika virus was first discovered in 1947 and is named after the Zika Forest in Uganda. In 1952, the first human cases of Zika were detected and since then, outbreaks of Zika have been reported in tropical Africa, Southeast Asia, and the Pacific Islands. Zika outbreaks have probably occurred in many locations. Before 2007, at least 14 cases of Zika had been documented, although other cases were likely to have occurred and were not reported. Because the symptoms of Zika are similar to those of many other diseases, many cases may not have been recognized.
What we know
- Zika is spread mostly by the bite of an infected Aedes species mosquito (Ae. aegypti and Ae. albopictus). These mosquitoes bite during the day and night.
- Zika can be passed from a pregnant woman to her fetus. Infection during pregnancy can cause certain birth defects.
- There is no vaccine or medicine for Zika.
- Local mosquito-borne Zika virus transmission has been reported in the continental United States. Learn more.
How Zika spreads
Zika can be transmitted
- Through mosquito bites
- From a pregnant woman to her fetus
- Through sex
- Through blood transfusion (very likely but not confirmed)
Learn how Zika is transmitted >>
Zika symptoms
Many people infected with Zika virus won’t have symptoms or will only have mild symptoms. The most common symptoms of Zika are
- Fever
- Rash
- Headache
- Joint pain
- Red eyes
- Muscle pain
Symptoms can last for several days to a week. People usually don’t get sick enough to go to the hospital, and they very rarely die of Zika. Once a person has been infected with Zika, they are likely to be protected from future infections.
Why Zika is risky for some people
Zika infection during pregnancy can cause a birth defect of the brain called microcephaly and other severe brain defects. It is also linked to other problems, such as miscarriage, stillbirth, and other birth defects. There have also been increased reports of Guillain-Barré syndrome, an uncommon sickness of the nervous system, in areas affected by Zika.
How to prevent Zika
There is no vaccine to prevent Zika. The best way to prevent diseases spread by mosquitoes is to protect yourself and your family from mosquito bites.
Clothing
- Wear long-sleeved shirts and long pants.
- Treat your clothing and gear with permethrin or buy pre-treated items.
Insect repellent
- Use Environmental Protection Agency (EPA)-registered insect repellents with one of the following active ingredients:
DEET, picaridin, IR3535, oil of lemon eucalyptus or para-menthane-diol, or 2-undecanone. Always follow the product label instructions.
- When used as directed, these insect repellents are proven safe and effective even for pregnant and breastfeeding women.
- Do not use insect repellents on babies younger than 2 months old.
- Do not use products containing oil of lemon eucalyptus or para-menthane-diol on children younger than 3 years old.
At Home
- Stay in places with air conditioning and window and door screens to keep mosquitoes outside.
- Take steps to control mosquitoes inside and outside your home.
- Mosquito netting can be used to cover babies younger than 2 months old in carriers, strollers, or cribs.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
Sexual transmission
- Prevent sexual transmission of Zika by using condoms or not having sex.
Learn about prevention >>
How Zika is diagnosed
- Diagnosis of Zika is based on a person’s recent travel history, symptoms, and test results.
- A blood or urine test can confirm a Zika infection.
- Symptoms of Zika are similar to other illnesses spread through mosquito bites, like dengue and chikungunya.
- Your doctor or other healthcare provider may order tests to look for several types of infections.
What to do if you have Zika
There is no specific medicine or vaccine for Zika virus. Treat the symptoms:
- Get plenty of rest.
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen to reduce fever and pain.
- Do not take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs).
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
Symptoms
Measuring Head Circumference
- English[PDF – 1 page]
- Spanish[PDF – 1 page]
- Portuguese[PDF – 1 page]
- French[PDF – 1 page]
- Creole[PDF – 1 page]

Many people infected with Zika virus won’t have symptoms or will only have mild symptoms. The most common symptoms of Zika are
- Fever
- Rash
- Headache
- Joint pain
- Conjunctivitis (red eyes)
- Muscle pain
How long symptoms last
Zika is usually mild with symptoms lasting for several days to a week. People usually don’t get sick enough to go to the hospital, and they very rarely die of Zika. For this reason, many people might not realize they have been infected. Symptoms of Zika are similar to other viruses spread through mosquito bites, like dengue and chikungunya.
How soon you should be tested
Zika virus usually remains in the blood of an infected person for about a week. See your doctor or other healthcare provider if you develop symptoms and you live in or have recently traveled to an area with risk of Zika. Your doctor or other healthcare provider may order blood tests to look for Zika or other similar viruses like dengue or chikungunya. Once a person has been infected, he or she is likely to be protected from future infections.
When to see a doctor or healthcare provider
See your doctor or other healthcare provider if you have the symptoms described above and have visited an area with risk of Zika. This is especially important if you are pregnant. Be sure to tell your doctor or other healthcare provider where you traveled.
Zika primarily spreads through infected mosquitoes. You can also get Zika through sex.
Many areas in the United States have the type of mosquitoes that can spread Zika virus. These mosquitoes bite during the day and night. Zika can also be passed through sex from a person who has Zika to his or her sex partners.
The best way to prevent Zika is to prevent mosquito bites.
- Use EPA-registered insect repellent. It works!
- Wear long-sleeved shirts and long pants.
- Stay in places with air conditioning or window and door screens.
- Remove standing water around your home.
Zika is linked to birth defects.
Zika infection during pregnancy can cause a serious birth defect called microcephaly that is a sign of incomplete brain development. Doctors have also found other problems in pregnancies and among fetuses and infants infected with Zika virus before birth. If you are pregnant and have a partner who lives in or has traveled to an area with risk of Zika, do not have sex, or use condoms the right way, every time, during your pregnancy.
Pregnant women should not travel to areas with risk of Zika.
If you must travel to one of these areas, talk to your healthcare provider first and strictly follow steps to prevent mosquito bites and sexual transmission during your trip. See CDC’s domestic guidance for information on travel within the continental US and Hawaii.
Returning travelers infected with Zika can spread the virus through mosquito bites.
During the first week of infection, Zika virus can be found in a person’s blood and can pass from an infected person to a mosquito through mosquito bites. An infected mosquito can then spread the virus to other people.
Couples with a partner who lives in or has traveled to an area with risk of Zika should take steps to protect during sex.
If you think you have Zika
- See your doctor or other healthcare provider for a diagnosis.
- Learn what you can do for treatment.
- Learn how you can protect others if you have Zika.
Through mosquito bites
Zika virus is transmitted to people primarily through the bite of an infected Aedes species mosquito (Ae. aegypti and Ae. albopictus). These are the same mosquitoes that spread dengue and chikungunya viruses.
- These mosquitoes typically lay eggs in and near standing water in things like buckets, bowls, animal dishes, flower pots and vases. They prefer to bite people, and live indoors and outdoors near people.Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.
- Mosquitoes that spread chikungunya, dengue, and Zika are aggressive daytime biters, but they can also bite at night.
From mother to child
- A pregnant woman can pass Zika virus to her fetus during pregnancy. Zika is a cause of microcephaly and other severe fetal brain defects. We are studying the full range of other potential health problems that Zika virus infection during pregnancy may cause.
- A pregnant woman already infected with Zika virus can pass the virus to her fetus during the pregnancy or around the time of birth.
- To date, there are no reports of infants getting Zika virus through breastfeeding. Because of the benefits of breastfeeding, mothers are encouraged to breastfeed even in areas with risk of Zika.
Through sex
- Zika can be passed through sex from a person who has Zika to his or her partners. Zika can be passed through sex, even if the infected person does not have symptoms at the time. Learn how to protect yourself during sex.Studies are underway to find out how long Zika stays in the semen and vaginal fluids of people who have Zika, and how long it can be passed to sex partners. We know that Zika can remain in semen longer than in other body fluids, including vaginal fluids, urine, and blood.
- It can be passed from a person with Zika before their symptoms start, while they have symptoms, and after their symptoms end.
- Though not well documented, the virus may also be passed by a person who carries the virus but never develops symptoms.
Through blood transfusion
- To date, there have not been any confirmed blood transfusion transmission cases in the United States.
- There have been multiple reports of blood transfusion transmission cases in Brazil. These reports are currently being investigated.
- During the French Polynesian outbreak, 2.8% of blood donors tested positive for Zika and in previous outbreaks, the virus has been found in blood donors.
Through laboratory and healthcare setting exposure
- Prior to the current outbreak, there were four reports of laboratory acquired Zika virus infections, although the route of transmission was not clearly established in all cases.
- As of June 15, 2016, there has been one reported case of laboratory-acquired Zika virus disease in the United States.
- To date, no cases of confirmed Zika virus transmission in healthcare settings have been reported in the United States. Recommendations are available for healthcare providers to help prevent exposure to Zika virus in healthcare settings.
Risks
- Anyone who lives in or travels to an area with risk of Zika and has not already been infected with Zika virus can get it from mosquito bites. Once a person has been infected, he or she is likely to be protected from future infections.
Why Zika is risky for some people
Zika infection during pregnancy can cause a birth defect of the brain called microcephaly and other severe brain defects. It is also linked to other problems, such as miscarriage, stillbirth, and other birth defects. There have also been increased reports of Guillain-Barré syndrome, an uncommon sickness of the nervous system, in areas affected by Zika.
How to prevent Zika
There is no vaccine to prevent Zika. The best way to prevent diseases spread by mosquitoes is to protect yourself and your family from mosquito bites.
Clothing
- Wear long-sleeved shirts and long pants.
- Treat your clothing and gear with permethrin or buy pre-treated items.
Insect repellent
- Use Environmental Protection Agency (EPA)-registered insect repellents with one of the following active ingredients:
DEET, picaridin, IR3535, oil of lemon eucalyptus or para-menthane-diol, or 2-undecanone. Always follow the product label instructions.
- When used as directed, these insect repellents are proven safe and effective even for pregnant and breastfeeding women.
- Do not use insect repellents on babies younger than 2 months old.
- Do not use products containing oil of lemon eucalyptus or para-menthane-diol on children younger than 3 years old.
At Home
- Stay in places with air conditioning and window and door screens to keep mosquitoes outside.
- Take steps to control mosquitoes inside and outside your home.
- Mosquito netting can be used to cover babies younger than 2 months old in carriers, strollers, or cribs.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
Sexual transmission
- Prevent sexual transmission of Zika by using condoms or not having sex.
Learn about prevention >>
How Zika is diagnosed
- Diagnosis of Zika is based on a person’s recent travel history, symptoms, and test results.
- A blood or urine test can confirm a Zika infection.
- Symptoms of Zika are similar to other illnesses spread through mosquito bites, like dengue and chikungunya.
- Your doctor or other healthcare provider may order tests to look for several types of infections.
What to do if you have Zika
There is no specific medicine or vaccine for Zika virus. Treat the symptoms:
- Get plenty of rest.
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen to reduce fever and pain.
- Do not take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs).
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
There is no specific medicine or vaccine for Zika virus.
- Treat the symptoms.
- Get plenty of rest.
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen (Tylenol®) to reduce fever and pain.
- Do not take aspirin and other non-steroidal anti-inflammatory drugs (NSAIDS) until dengue can be ruled out to reduce the risk of bleeding.
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
If you think you may have or had Zika
Tell your doctor or healthcare provider and take these steps to protect others.
If you are caring for a person with Zika
Take steps to protect yourself from exposure to the person’s blood and body fluids (urine, stool, vomit). If you are pregnant, you can care for someone with Zika if you follow these steps.
- Do not touch blood or body fluids or surfaces with these fluids on them with exposed skin.
- Wash hands with soap and water immediately after providing care.
- Immediately remove and wash clothes if they get blood or body fluids on them. Use laundry detergent and water temperature specified on the garment label. Using bleach is not necessary.
- Clean the sick person’s environment daily using household cleaners according to label instructions.
- Immediately clean surfaces that have blood or other body fluids on them using household cleaners and disinfectants according to label instructions.
If you visit a family member or friend with Zika in a hospital, you should avoid contact with the person’s blood and body fluids and surfaces with these fluids on them. Helping the person sit up or walk should not expose you. Make sure to wash your hands before and after touching the person.
History of Zika
Zika virus was first discovered in 1947 and is named after the Zika Forest in Uganda. In 1952, the first human cases of Zika were detected and since then, outbreaks of Zika have been reported in tropical Africa, Southeast Asia, and the Pacific Islands. Zika outbreaks have probably occurred in many locations. Before 2007, at least 14 cases of Zika had been documented, although other cases were likely to have occurred and were not reported. Because the symptoms of Zika are similar to those of many other diseases, many cases may not have been recognized.
Related Resources
Zika 101 Presentation
- English[PPT - 3.7 MB]
- Spanish[PPT - 3.6 MB]
- Portuguese[PPT - 3.6 MB]
Zika: The Basics of the Virus and How to Protect Against It

What we know
- No vaccine exists to prevent Zika.
- Prevent Zika by avoiding mosquito bites.
- Mosquitoes that spread Zika virus bite during the day and night.
- Mosquitoes that spread Zika virus also spread dengue and chikungunya viruses.
- Zika can be passed through sex from a person who has Zika to his or her sex partners. Condoms can reduce the chance of getting Zika from sex. Condoms include male and female condoms.
- Local mosquito-borne Zika virus transmission has been reported in the continental United States.
What you can do to protect yourself and others
No, bedbugs do not cause scabies. Both of these are completely different infestations. Let’s learn more.
Before delving into the differences, check the main points of matches between the bedbug bites and scabies
- Both of them can cause itchy rashes on our skin
- The itchiness is usually worse at nighttime.
- In both the cases, if you are in doubt of getting any of them, immediate diagnosis and professional treatment accordingly is important.
Now, here are the points of differences between scabies and bedbug bites:
- See more at: http://www.drscabies.com/can-bedbugs-cause-scabie#sthash.XFVKpIiN.dpuf
Source: CDC









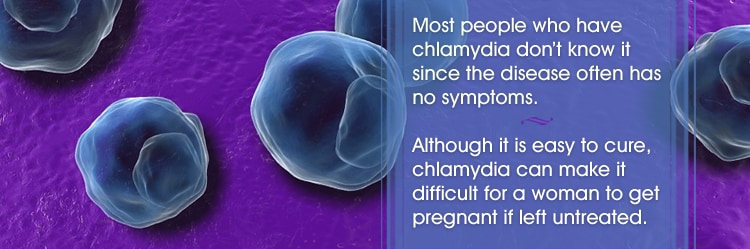















![Granuloma inguinale (klik op foto voor vergroting) [bron: Wikipedia] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-1z.jpg)
![Granuloma inguinale (klik op foto voor vergroting) [bron: www.tuasaude.com] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-2z.jpg)
![Granuloma inguinale (klik op foto voor vergroting) [bron: www.genitaldischarge.com] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-3z.jpg)
![Granuloma inguinale (klik op foto voor vergroting) [bron: www.studyblue.com] Granuloma inguinale](https://www.huidziekten.nl/afbeeldingen/soa/granuloma-inguinale-4z.jpg)